1. Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients.
Kidney Int 1999;55:648–658.


2. Amdur RL, Feldman HI, Gupta J, et al. Inflammation and progression of CKD: the CRIC study.
Clin J Am Soc Nephrol 2016;11:1546–1556.



3. Yang Y, Zhang Y, Xu Y, et al. Dietary methionine restriction improves the gut microbiota and reduces intestinal permeability and inflammation in high-fat-fed mice.
Food Funct 2019;10:5952–5968.


4. Andersen K, Kesper MS, Marschner JA, et al. Intestinal dysbiosis, barrier dysfunction, and bacterial translocation account for CKD-related systemic inflammation.
J Am Soc Nephrol 2017;28:76–83.


5. Yang J, Lim SY, Ko YS, et al. Intestinal barrier disruption and dysregulated mucosal immunity contribute to kidney fibrosis in chronic kidney disease.
Nephrol Dial Transplant 2019;34:419–428.


6. Hill C, Guarner F, Reid G, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic.
Nat Rev Gastroenterol Hepatol 2014;11:506–514.


7. Soleimani A, Zarrati Mojarrad M, Bahmani F, et al. Probiotic supplementation in diabetic hemodialysis patients has beneficial metabolic effects.
Kidney Int 2017;91:435–442.


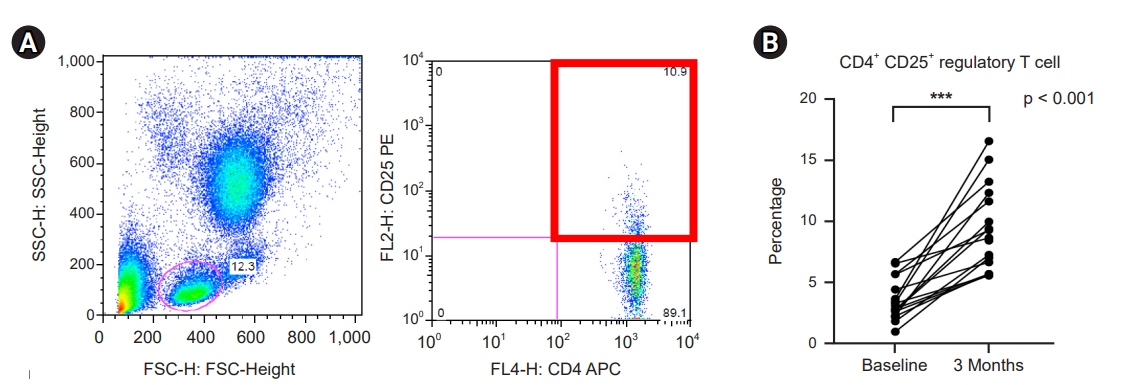
8. Smigiel KS, Srivastava S, Stolley JM, Campbell DJ. Regulatory T-cell homeostasis: steady-state maintenance and modulation during inflammation.
Immunol Rev 2014;259:40–59.



9. Heine GH, Ortiz A, Massy ZA, et al. Monocyte subpopulations and cardiovascular risk in chronic kidney disease.
Nat Rev Nephrol 2012;8:362–369.


10. Lee JW, Cho E, Kim MG, Jo SK, Cho WY, Kim HK. Proinflammatory CD14(+)CD16(+) monocytes are associated with vascular stiffness in predialysis patients with chronic kidney disease.
Kidney Res Clin Pract 2013;32:147–152.



11. Caporaso JG, Kuczynski J, Stombaugh J, et al. QIIME allows analysis of high-throughput community sequencing data.
Nat Methods 2010;7:335–336.



12. Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJ, Holmes SP. DADA2: high-resolution sample inference from Illumina amplicon data.
Nat Methods 2016;13:581–583.



13. DeSantis TZ, Hugenholtz P, Larsen N, et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB.
Appl Environ Microbiol 2006;72:5069–5072.



14. McDonald D, Price MN, Goodrich J, et al. An improved Greengenes taxonomy with explicit ranks for ecological and evolutionary analyses of bacteria and archaea.
ISME J 2012;6:610–618.


15. Chen YY, Chen DQ, Chen L, et al. Microbiome-metabolome reveals the contribution of gut-kidney axis on kidney disease.
J Transl Med 2019;17:5.



16. Sampaio-Maia B, Simões-Silva L, Pestana M, Araujo R, Soares-Silva IJ. The role of the gut microbiome on chronic kidney disease.
Adv Appl Microbiol 2016;96:65–94.


17. Jia L, Jia Q, Yang J, Jia R, Zhang H. Efficacy of probiotics supplementation on chronic kidney disease: a systematic review and meta-analysis.
Kidney Blood Press Res 2018;43:1623–1635.


18. Park MS, Kwon B, Ku S, Ji GE. The efficacy of Bifidobacterium longum BORI and Lactobacillus acidophilus AD031 probiotic treatment in infants with rotavirus infection.
Nutrients 2017;9:887.



19. Seo JM, Ji GE, Cho SH, Park MS, Lee HJ. Characterization of a Bifidobacterium longum BORI dipeptidase belonging to the U34 family.
Appl Environ Microbiol 2007;73:5598–5606.



20. Ku S, Park MS, Ji GE, You HJ. Review on Bifidobacterium bifidum BGN4: functionality and nutraceutical applications as a probiotic microorganism.
Int J Mol Sci 2016;17:1544.



21. Yu DS, Jeong H, Lee DH, et al. Complete genome sequence of the probiotic bacterium Bifidobacterium bifidum strain BGN4.
J Bacteriol 2012;194:4757–4758.



22. Kim MJ, Ku S, Kim SY, et al. Safety evaluations of Bifidobacterium bifidum BGN4 and Bifidobacterium longum BORI.
Int J Mol Sci 2018;19:1422.



23. McIntyre CW, Harrison LE, Eldehni MT, et al. Circulating endotoxemia: a novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease.
Clin J Am Soc Nephrol 2011;6:133–141.



24. Wu HJ, Wu E. The role of gut microbiota in immune homeostasis and autoimmunity.
Gut Microbes 2012;3:4–14.



25. Ziegler-Heitbrock L, Ancuta P, Crowe S, et al. Nomenclature of monocytes and dendritic cells in blood.
Blood 2010;116:e74–e80.


26. Mahajan D, Wang Y, Qin X, et al. CD4+CD25+ regulatory T cells protect against injury in an innate murine model of chronic kidney disease.
J Am Soc Nephrol 2006;17:2731–2741.


27. Pastrana JL, Sha X, Virtue A, et al. Regulatory T cells and atherosclerosis.
J Clin Exp Cardiolog 2012;2012(Suppl 12):2.


28. Wang J, Li XB, Huang P, Huang MY, Gu XJ. Change of peripheral blood Treg/Thl7 in cognitive impairment with chronic renal failure patients.
Cell Physiol Biochem 2018;45:281–290.


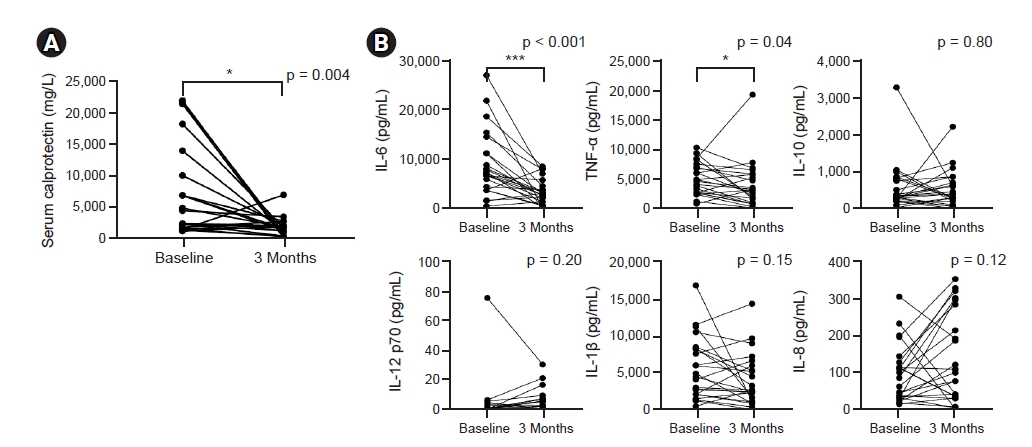
29. Azramezani Kopi T, Shahrokh S, Mirzaei S, Asadzadeh Aghdaei H, Amini Kadijani A. The role of serum calprotectin as a novel biomarker in inflammatory bowel diseases: a review study.
Gastroenterol Hepatol Bed Bench 2019;12:183–189.


30. Gray RD, Imrie M, Boyd AC, Porteous D, Innes JA, Greening AP. Sputum and serum calprotectin are useful biomarkers during CF exacerbation.
J Cyst Fibros 2010;9:193–198.


31. Kawasaki Y, Ohara S, Abe Y, et al. The role of serum myeloid-related protein 8/14 complex in Henoch-Schönlein purpura nephritis.
Pediatr Nephrol 2012;27:65–71.


32. Martinez Valenzuela L, Draibe J, Quero Ramos M, et al. Calprotectin as a smoldering activity detection tool and renal prognosis biomarker in ANCA associated vasculitis.
PLoS One 2018;13:e0205982.



33. Su H, Lei CT, Zhang C. Interleukin-6 signaling pathway and its role in kidney disease: an update.
Front Immunol 2017;8:405.



34. Huber SA, Sakkinen P, Conze D, Hardin N, Tracy R. Interleukin-6 exacerbates early atherosclerosis in mice.
Arterioscler Thromb Vasc Biol 1999;19:2364–2367.


35. Wang IK, Wu YY, Yang YF, et al. The effect of probiotics on serum levels of cytokine and endotoxin in peritoneal dialysis patients: a randomised, double-blind, placebo-controlled trial.
Benef Microbes 2015;6:423–430.


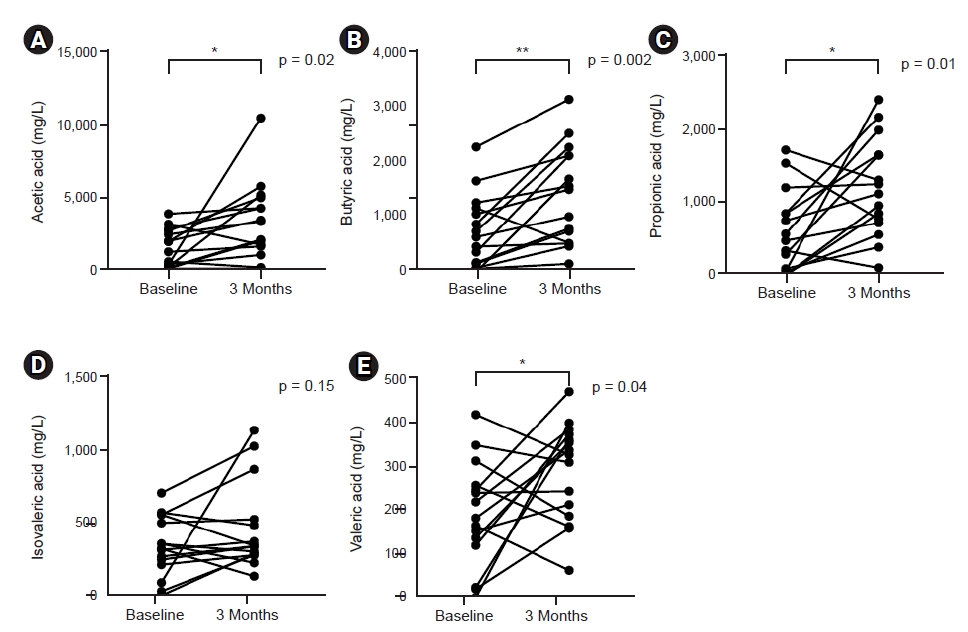
36. Markowiak-Kopeć P, Śliżewska K. The effect of probiotics on the production of short-chain fatty acids by human intestinal microbiome.
Nutrients 2020;12:1107.



37. van der Beek CM, Dejong CHC, Troost FJ, Masclee AAM, Lenaerts K. Role of short-chain fatty acids in colonic inflammation, carcinogenesis, and mucosal protection and healing.
Nutr Rev 2017;75:286–305.


38. Kanitsoraphan C, Rattanawong P, Charoensri S, Senthong V. Trimethylamine N-oxide and risk of cardiovascular disease and mortality.
Curr Nutr Rep 2018;7:207–213.


39. Wong J, Piceno YM, DeSantis TZ, Pahl M, Andersen GL, Vaziri ND. Expansion of urease- and uricase-containing, indole- and p-cresol-forming and contraction of short-chain fatty acid-producing intestinal microbiota in ESRD.
Am J Nephrol 2104;39:230–237.

40. Li L, Ma L, Fu P. Gut microbiota-derived short-chain fatty acids and kidney diseases.
Drug Des Devel Ther 2017;11:3531–3542.


















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















