1. Tinajero MG, Malik VS. An update on the epidemiology of type 2 diabetes: a global perspective.
Endocrinol Metab Clin North Am 2021;50:337–355.

2. Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities.
Clin J Am Soc Nephrol 2017;12:2032–2045.


3. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications.
Nat Rev Endocrinol 2018;14:88–98.



4. Tang S, Yiu WH. Innate immunity in diabetic kidney disease.
Nat Rev Nephrol 2020;16:206–222.



5. Heise T, Seewaldt-Becker E, Macha S, et al. Safety, tolerability, pharmacokinetics and pharmacodynamics following 4 weeks’ treatment with empagliflozin once daily in patients with type 2 diabetes.
Diabetes Obes Metab 2013;15:613–621.


7. Weber MA, Mansfield TA, Cain VA, Iqbal N, Parikh S, Ptaszynska A. Blood pressure and glycaemic effects of dapagliflozin versus placebo in patients with type 2 diabetes on combination antihypertensive therapy: a randomised, double-blind, placebo-controlled, phase 3 study.
Lancet Diabetes Endocrinol 2016;4:211–220.


8. Tikkanen I, Narko K, Zeller C, et al. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension.
Diabetes Care 2015;38:420–428.



9. Rosenstock J, Jelaska A, Frappin G, et al. Improved glucose control with weight loss, lower insulin doses, and no increased hypoglycemia with empagliflozin added to titrated multiple daily injections of insulin in obese inadequately controlled type 2 diabetes.
Diabetes Care 2014;37:1815–1823.



10. Ye N, Jardine MJ, Oshima M, et al. Blood pressure effects of canagliflozin and clinical outcomes in type 2 diabetes and chronic kidney disease: insights from the CREDENCE trial.
Circulation 2021;143:1735–1749.


11. Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy.
N Engl J Med 2019;380:2295–2306.


12. Heerspink H, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease.
N Engl J Med 2020;383:1436–1446.


13. Wanner C, Lachin JM, Inzucchi SE, et al. Empagliflozin and clinical outcomes in patients with type 2 diabetes mellitus, established cardiovascular disease, and chronic kidney disease.
Circulation 2018;137:119–129.


14. Sarafidis P, Ferro CJ, Morales E, et al. SGLT-2 inhibitors and GLP-1 receptor agonists for nephroprotection and cardioprotection in patients with diabetes mellitus and chronic kidney disease. A consensus statement by the EURECA-m and the DIABESITY working groups of the ERA-EDTA.
Nephrol Dial Transplant 2019;34:208–230.


15. Moore TJ, Conlin PR, Ard J, Svetkey LP. DASH (dietary approaches to stop hypertension) diet is effective treatment for stage 1 isolated systolic hypertension.
Hypertension 2001;38:155–158.


16. Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease.
Kidney Int 2020;98:S1–S115.


17. Liew A, Bavanandan S, Prasad N, et al. Asian Pacific Society of Nephrology clinical practice guideline on diabetic kidney disease: executive summary.
Nephrology (Carlton) 2020;25 Suppl 2:3–11.



18. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group.
Lancet 1998;352:854–865.

19. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes.
N Engl J Med 2008;359:1577–1589.


20. ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes.
N Engl J Med 2008;358:2560–2572.


21. Zoungas S, Chalmers J, Neal B, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes.
N Engl J Med 2014;371:1392–1406.


22. Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes.
N Engl J Med 2009;360:129–139.


23. Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis.
JAMA 2015;313:603–615.


24. ACCORD Study Group, Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus.
N Engl J Med 2010;362:1575–1585.



25. Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier.
Ann Intern Med 2011;154:541–548.


26. Imai E, Ito S, Haneda M, et al. Effects of blood pressure on renal and cardiovascular outcomes in Asian patients with type 2 diabetes and overt nephropathy: a post hoc analysis (ORIENT-blood pressure).
Nephrol Dial Transplant 2016;31:447–454.



27. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease.
Kidney Int 2021;99:S1–S87.


28. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes.
N Engl J Med 2001;345:851–860.


29. ONTARGET Investigators, Yusuf S, Teo KK, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events.
N Engl J Med 2008;358:1547–1559.


30. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy.
N Engl J Med 2001;345:861–869.


31. Haller H, Ito S, Izzo JL Jr, et al. Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes.
N Engl J Med 2011;364:907–917.


32. Asmar A, Cramon PK, Asmar M, et al. The renal extraction and the natriuretic action of GLP-1 in humans depend on interaction with the GLP-1 receptor.
J Clin Endocrinol Metab 2021;106:e11–e19.



33. von Websky K, Reichetzeder C, Hocher B. Physiology and pathophysiology of incretins in the kidney.
Curr Opin Nephrol Hypertens 2014;23:54–60.


34. Yin QH, Zhang R, Li L, et al. Exendin-4 ameliorates lipotoxicity-induced glomerular endothelial cell injury by improving ABC transporter A1-mediated cholesterol efflux in diabetic apoE knockout mice.
J Biol Chem 2016;291:26487–26501.



35. Yamada S, Tanabe J, Ogura Y, et al. Renoprotective effect of GLP-1 receptor agonist, liraglutide, in early-phase diabetic kidney disease in spontaneously diabetic Torii fatty rats.
Clin Exp Nephrol 2021;25:365–375.



36. Abdel-Latif RG, Ahmed AF, Heeba GH. Low-dose lixisenatide protects against early-onset nephropathy induced in diabetic rats.
Life Sci 2020;263:118592.


39. Li W, Cui M, Wei Y, Kong X, Tang L, Xu D. Inhibition of the expression of TGF-β1 and CTGF in human mesangial cells by exendin-4, a glucagon-like peptide-1 receptor agonist.
Cell Physiol Biochem 2012;30:749–757.


40. Huang L, Lin T, Shi M, Chen X, Wu P. Liraglutide suppresses production of extracellular matrix proteins and ameliorates renal injury of diabetic nephropathy by enhancing Wnt/β-catenin signaling.
Am J Physiol Renal Physiol 2020;319:F458–F468.


41. Moellmann J, Klinkhammer BM, Onstein J, et al. Glucagon-like peptide 1 and its cleavage products are renoprotective in murine diabetic nephropathy.
Diabetes 2018;67:2410–2419.



42. Kodera R, Shikata K, Kataoka HU, et al. Glucagon-like peptide-1 receptor agonist ameliorates renal injury through its anti-inflammatory action without lowering blood glucose level in a rat model of type 1 diabetes.
Diabetologia 2011;54:965–978.



43. Moschovaki Filippidou F, Kirsch AH, Thelen M, et al. Glucagon-like peptide-1 receptor agonism improves nephrotoxic serum nephritis by inhibiting T-cell proliferation.
Am J Pathol 2020;190:400–411.


44. Farah LX, Valentini V, Pessoa TD, Malnic G, McDonough AA, Girardi AC. The physiological role of glucagon-like peptide-1 in the regulation of renal function.
Am J Physiol Renal Physiol 2016;310:F123–F127.



45. Kim M, Platt MJ, Shibasaki T, et al. GLP-1 receptor activation and Epac2 link atrial natriuretic peptide secretion to control of blood pressure.
Nat Med 2013;19:567–575.



46. von Scholten BJ, Persson F, Rosenlund S, et al. The effect of liraglutide on renal function: a randomized clinical trial.
Diabetes Obes Metab 2017;19:239–247.



51. Habib HA, Heeba GH, Khalifa M. Effect of combined therapy of mesenchymal stem cells with GLP-1 receptor agonist, exenatide, on early-onset nephropathy induced in diabetic rats.
Eur J Pharmacol 2021;892:173721.


52. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes.
N Engl J Med 2016;375:311–322.



53. Mann JFE, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and renal outcomes in type 2 diabetes.
N Engl J Med 2017;377:839–848.


54. Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes.
N Engl J Med 2016;375:1834–1844.


55. Gerstein HC, Sattar N, Rosenstock J, et al. Cardiovascular and renal outcomes with efpeglenatide in type 2 diabetes.
N Engl J Med 2021;385:896–907.


56. Muskiet M, Tonneijck L, Huang Y, et al. Lixisenatide and renal outcomes in patients with type 2 diabetes and acute coronary syndrome: an exploratory analysis of the ELIXA randomised, placebo-controlled trial.
Lancet Diabetes Endocrinol 2018;6:859–869.


57. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial.
Lancet 2019;394:131–138.

58. Tuttle KR, Lakshmanan MC, Rayner B, et al. Dulaglutide versus insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease (AWARD-7): a multicentre, open-label, randomised trial.
Lancet Diabetes Endocrinol 2018;6:605–617.


60. Leehey DJ, Rahman MA, Borys E, Picken MM, Clise CE. Acute kidney injury associated with semaglutide.
Kidney Med 2021;3:282–285.



61. Scheen AJ. Pharmacokinetics and clinical use of incretin-based therapies in patients with chronic kidney disease and type 2 diabetes.
Clin Pharmacokinet 2015;54:1–21.



62. Ocello A, La Rosa S, Fiorini F, et al. [Antifibrotic renal role of mineralcorticoid receptor antagonists]. G Ital Nefrol 2019 36:2019-vol4.In Italian.
63. Buonafine M, Bonnard B, Jaisser F. Mineralocorticoid receptor and cardiovascular disease.
Am J Hypertens 2018;31:1165–1174.


64. Grune J, Beyhoff N, Smeir E, et al. Selective mineralocorticoid receptor cofactor modulation as molecular basis for finerenone’s antifibrotic activity.
Hypertension 2018;71:599–608.


66. Sarafidis PA, Memmos E, Alexandrou ME, Papagianni A. Mineralocorticoid receptor antagonists for nephroprotection: current evidence and future perspectives.
Curr Pharm Des 2018;24:5528–5536.


67. Guo C, Martinez-Vasquez D, Mendez GP, et al. Mineralocorticoid receptor antagonist reduces renal injury in rodent models of types 1 and 2 diabetes mellitus.
Endocrinology 2006;147:5363–5373.



68. Kolkhof P, Delbeck M, Kretschmer A, et al. Finerenone, a novel selective nonsteroidal mineralocorticoid receptor antagonist protects from rat cardiorenal injury.
J Cardiovasc Pharmacol 2014;64:69–78.


69. Katayama S, Yamada D, Nakayama M, et al. A randomized controlled study of finerenone versus placebo in Japanese patients with type 2 diabetes mellitus and diabetic nephropathy.
J Diabetes Complications 2017;31:758–765.


70. Bakris GL, Agarwal R, Chan JC, et al. Effect of finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial.
JAMA 2015;314:884–894.


71. Ito S, Kashihara N, Shikata K, et al. Esaxerenone (CS-3150) in patients with type 2 diabetes and microalbuminuria (ESAX-DN): phase 3 randomized controlled clinical trial.
Clin J Am Soc Nephrol 2020;15:1715–1727.


73. Bakris GL, Agarwal R, Anker SD, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes.
N Engl J Med 2020;383:2219–2229.


74. Filippatos G, Anker SD, Agarwal R, et al. Finerenone and cardiovascular outcomes in patients with chronic kidney disease and type 2 diabetes.
Circulation 2021;143:540–552.



75. Agarwal R, Joseph A, Anker SD, et al. Hyperkalemia risk with finerenone: results from the FIDELIO-DKD trial.
J Am Soc Nephrol 2022;33:225–237.



76. Pitt B, Filippatos G, Agarwal R, et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes.
N Engl J Med 2021;385:2252–2263.


77. Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy.
N Engl J Med 2013;369:1892–1903.


78. Parving HH, Brenner BM, McMurray JJ, et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes.
N Engl J Med 2012;367:2204–2213.


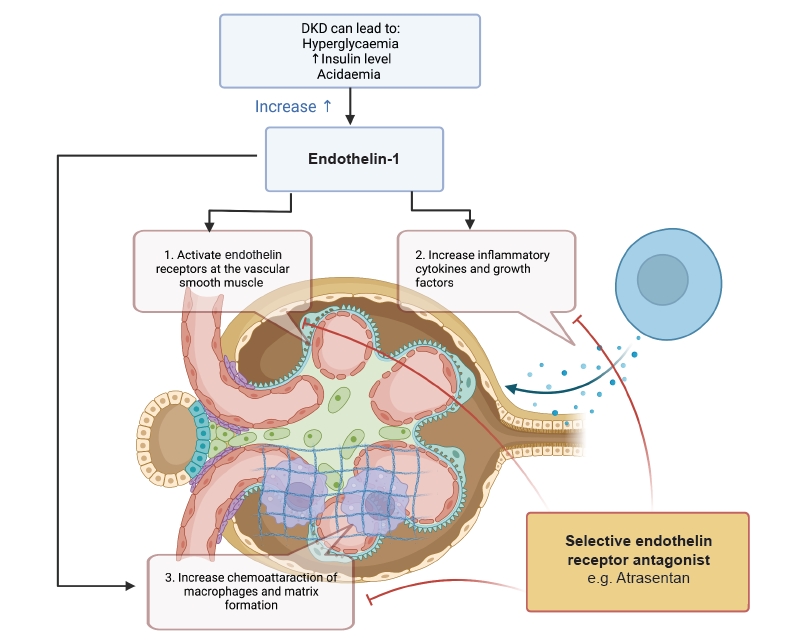
79. Dhaun N, Yuzugulen J, Kimmitt RA, et al. Plasma pro-endothelin-1 peptide concentrations rise in chronic kidney disease and following selective endothelin A receptor antagonism.
J Am Heart Assoc 2015;4:e001624.



80. Sasser JM, Sullivan JC, Hobbs JL, et al. Endothelin A receptor blockade reduces diabetic renal injury via an anti-inflammatory mechanism.
J Am Soc Nephrol 2007;18:143–154.



81. Rafnsson A, Böhm F, Settergren M, Gonon A, Brismar K, Pernow J. The endothelin receptor antagonist bosentan improves peripheral endothelial function in patients with type 2 diabetes mellitus and microalbuminuria: a randomised trial.
Diabetologia 2012;55:600–607.



82. Mann JF, Green D, Jamerson K, et al. Avosentan for overt diabetic nephropathy.
J Am Soc Nephrol 2010;21:527–535.



83. Wenzel RR, Littke T, Kuranoff S, et al. Avosentan reduces albumin excretion in diabetics with macroalbuminuria.
J Am Soc Nephrol 2009;20:655–664.



84. Farrah TE, Anand A, Gallacher PJ, et al. Endothelin receptor antagonism improves lipid profiles and lowers PCSK9 (proprotein convertase subtilisin/kexin type 9) in patients with chronic kidney disease.
Hypertension 2019;74:323–330.



85. Dhaun N, MacIntyre IM, Kerr D, et al. Selective endothelin-A receptor antagonism reduces proteinuria, blood pressure, and arterial stiffness in chronic proteinuric kidney disease.
Hypertension 2011;57:772–779.


86. Dhaun N, Macintyre IM, Melville V, et al. Blood pressure-independent reduction in proteinuria and arterial stiffness after acute endothelin-a receptor antagonism in chronic kidney disease.
Hypertension 2009;54:113–119.


87. Weber MA, Black H, Bakris G, et al. A selective endothelin-receptor antagonist to reduce blood pressure in patients with treatment-resistant hypertension: a randomised, double-blind, placebo-controlled trial.
Lancet 2009;374:1423–1431.


88. de Zeeuw D, Coll B, Andress D, et al. The endothelin antagonist atrasentan lowers residual albuminuria in patients with type 2 diabetic nephropathy.
J Am Soc Nephrol 2014;25:1083–1093.



89. Heerspink H, Parving HH, Andress DL, et al. Atrasentan and renal events in patients with type 2 diabetes and chronic kidney disease (SONAR): a double-blind, randomised, placebo-controlled trial.
Lancet 2019;393:1937–1947.



90. Waijer SW, de Vries ST, Busch R, et al. Large between-patient variability in eGFR decline before clinical trial enrollment and impact on atrasentan\'s efficacy: a post hoc analysis from the SONAR trial.
J Am Soc Nephrol 2021;32:2731–2734.

91. Kohan DE, Pritchett Y, Molitch M, et al. Addition of atrasentan to renin-angiotensin system blockade reduces albuminuria in diabetic nephropathy.
J Am Soc Nephrol 2011;22:763–772.











 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















