Introduction
Tumoral calcinosis is a rare condition characterized by calcium phosphate deposits in subcutaneous soft tissues usually around the joints. The prevalence of uremic tumoral calcinosis in patients undergoing peritoneal dialysis (PD) was estimated by a Japanese study [1] to be 1.6%, roughly equivalent to its prevalence in hemodialysis patients. Although the pathogenesis of uremic tumoral calcinosis is not yet fully understood, it is commonly associated with a buildup of calcium-phosphate product and hyperparathyroidism.
Here, we present the case of a patient on PD in whom severe tumoral calcinosis with infection developed. Near-complete resolution of deposits was achieved following administration of antibiotics, low-calcium dialysate, and sevelamer treatment.
Case report
A 25-year-old man treated with PD for >9 years presented with painful masses on both buttocks and hip joints. The patient had end-stage renal disease secondary to Schönlein–Henoch purpura, and underwent a kidney transplant 16 years previously. Following gradual deterioration of allograft function, PD had been initiated 7 years after transplantation. The PD schedule comprised four exchanges of 1.5 L dialysate (Perisis, Boryung, Korea) with 3.5 mEq/L calcium. A calcium acetate phosphate binder (2,130 mg) had been added during the past 5 years of PD, and active vitamin D3 was administered intermittently. The patient was anuric with weekly Kt/V urea values of 1.633.
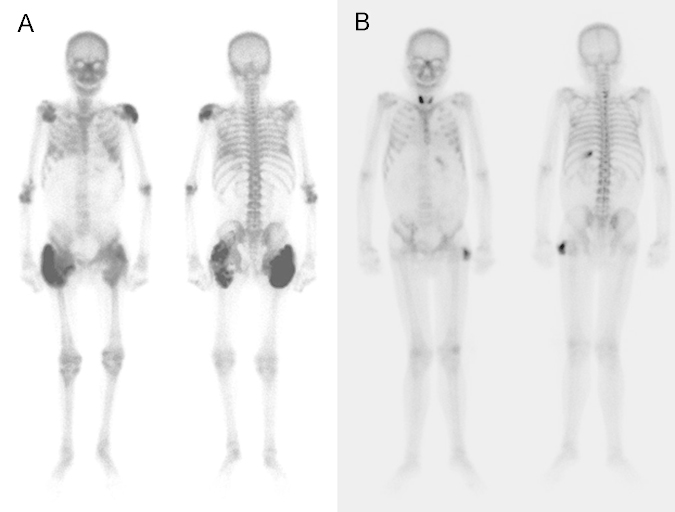
On admission, physical examination revealed painful nodular masses around both hip joints and buttocks. The masses were firm and lobular with signs of soft-tissue infection. Laboratory findings were as follows: hemoglobin, 7.5 g/dL; total calcium, 9.9 mg/dL; phosphate, 3.7 mg/dL; intact parathyroid hormone (iPTH), 417.6 pg/mL; and C-reactive protein (CRP), 31.2 mg/dL. Microbiologic blood culture results were positive for Staphylococcus haemolyticus. Pelvic radiography revealed tumoral calcinosis in both hip joints (Fig. 1). A technetium 99m scan showed increased uptake in both hip joints and shoulders (Fig. 2A).
First-generation cephalosporin was administered, and calcium acetate was replaced with sevelamer, a non-calcium containing phosphate binder. After 1 month, the serum calcium and ionized calcium levels were 10.7 mg/dL and 2.56 mEq/L, respectively. PD fluid was switched to low-calcium dialysate (2.5 mEq/L calcium). After 12 months, the patient was symptom free and serum calcium levels reduced to 8.8 mg/dL. After 17 months, the patient remained asymptomatic, although serum calcium levels were reduced to 8.5 mg/dL, and iPTH levels were increased to 734.1 pg/mL. Active vitamin D3 was readministered. Over the following 12 months, serum calcium level remained between 9.2 mg/dL and 10 mg/dL, phosphate level between 4.0 mg/dL and 6.0 mg/dL, and iPTH level <350 pg/mL. By 36 months, a follow-up bone scan confirmed striking resolution of tumoral calcinosis, with only a small residual lesion near the left femoral head (Fig. 2B).
Currently, the patient is asymptomatic, with serum calcium level of 9.3 mg/dL, serum phosphate level of 5.6 mg/dL, and serum iPTH level of 226 pg/mL (Fig. 3).
Discussion
We presented a case of uremic tumoral calcinosis in a patient undergoing PD with moderate hyperparathyroidism. In this study, PD was not substituted for, or combined with, hemodialysis. Treatment of tumoral calcinosis, comprising administration of low-calcium dialysate with a non-calcium-containing phosphate binder, resulted in near-complete resolution of pathology.
Uremic tumoral calcinosis is a rare complication in uremic patients. Its etiology is incompletely understood, although increased deposition of calcium-phosphate product secondary to hyperparathyroidism, dialysis vintage, and vitamin D intoxication have been implicated in its pathogenesis [2]. In the patient described here, iPTH level increased to 417.6 pg/mL without an increase in the calcium-phosphate product level beyond 36.6 mg2/dL2, contrary to previous reports by Chu et al [1], in which all of seven cases of uremic tumoral calcinosis were associated high calcium-phosphate product levels. In this instance, however, the dialysis vintage of >9 years was longer than that previously reported.
Uremic tumoral calcinosis can be unifocal or multifocal, and patients may present with localized swelling, pain, pruritus, ulceration, and infection [3]. Lesions are typically observed around the weight-bearing joints particularly susceptible to excessive wear, such as the shoulders, elbows, and hips. In this case, the predominant manifestation was painful multifocal masses on both hip joints, although a bone scan revealed additional lesions in the patient’s shoulders. Upon physical examination, signs of infection were observed around the masses. Hamada et al [3] previously reported that 25% of patients with uremic tumoral calcinosis present with infection.
Several medical and surgical strategies have been considered for the treatment of uremic tumoral calcinosis. Medical treatment consists of a non-calcium phosphate binder, low-calcium dialysate, or increased dose of dialysis. A thorough literature review identified 16 published cases of PD patients with uremic tumoral calcinosis. In all cases, medical treatment was unsuccessful [1]. Chu et al [1] reported that two of seven patients received only medical therapy including a phosphate-restricted diet, a calcium or non-calcium phosphate binder, and intensive dialysis with low-calcium dialysate (2 mEq/L). However, medical therapy was ineffective in all cases. In cases of hemodialysis patients with uremic tumoral calcinosis, daily hemodialysis with a low-calcium dialysate or daily nocturnal dialysis has been found to effectively decrease and resolve massive tumoral calcinosis [4], [5].
Kuriyama et al [6] suggested that combining hemodialysis with PD using a low-calcium dialysate can be effective in patients undergoing PD with tumoral calcinosis. Surgical treatment, including excision of calcific masses or parathyroidectomy in case of severe secondary hyperparathyroidism, is indicated in patients resistant to medical treatment. It is interesting that in the case presented here, near-complete resolution of uremic tumoral calcinosis was observed after 36 months of medical intervention with low-calcium dialysis and sevelamer, a non-calcium phosphate binder.
In conclusion, medical management with low-calcium dialysate and a non-calcium phosphate binder over a prolonged interval can resolve massive uremic tumoral calcinosis in patients with PD.





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















