Introduction
Coronavirus disease 2019 (COVID-19) is a disease caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has affected nearly 4 billion people to date and caused about 6 million deaths worldwide. Previous reports have determined that old age, comorbidities, and an immunocompromised state can increase the risk of death from COVID-19 [
1–
3]. Moreover, patients with end-stage renal disease exhibit a higher mortality rate compared to the general population. A study by a Belgian group recently reported the incidence, outcome, and mortality burden of SARS-CoV-2 infection in the Flemish region. They documented higher incidence (5.3% vs. 0.6%) and mortality (29.6% vs. 15.3%) rates among patients receiving hemodialysis (HD) compared to the general population [
4]. Other recent studies from other countries have determined the mortality rate of HD patients to be around 30% [
5–
7].
Meanwhile, the COVID-19 Task Force Team, established under the Korean Society of Nephrology at the beginning of the COVID-19 pandemic, has developed COVID-19 prevention guidelines for HD units [
8,
9]. Thanks to the adherence to stringent primary prevention strategies in Korea, the overall fatality rate of COVID-19 in the general population has been lower than that in other countries (0.8% vs. 1.5%) [
10]. However, no study has evaluated the mortality rate using a nationwide cohort database among HD patients in Korea. Therefore, this study evaluated the in-hospital fatality rate among Korean HD patients with a COVID-19 diagnosis and compared it to that of patients without chronic kidney disease (CKD). We also analyzed risk factors associated with in-hospital fatality among COVID-19–positive HD patients.
Methods
This study was approved by the Institutional Review Board of Hallym University Kangnam Sacred Heart Hospital (No. HKS 2021-07-013). The need to gather informed consent was waived due to the retrospective nature of the study.
Data collection
From February 2020 to November 2021, clinical information as well as clinical outcomes of confirmed cases of COVID-19 were collected from each HD unit every 6 months using a nationwide survey. The survey was sent to each nephrologist to fill up the data, then returned to the Korean Society of Nephrology COVID-19 Task Force Team by e-mail. The clinical information of interest included patient age and sex; location and date of diagnosis; presence and type of initial symptoms; duration of hospitalization; admission to the intensive care unit (ICU); and use of mechanical ventilation (MV), continuous renal-replacement therapy, or extracorporeal membrane oxygenation. We also collected data about the type of dialysis unit and the presence of a nephrologist on staff at the dialysis unit.
We used the Korean COVID-19 nationwide database available from Korea Disease Control and Prevention Agency (KDCA) and excluded data of patients with CKD to compare clinical outcomes between the non-CKD population and HD patients. Among 5,628 patients confirmed to have COVID-19 up to April 30, 2020, a total of 5,570 patients were included in the current analysis as control subjects after excluding 58 patients with CKD.
Clinical outcome
First, we analyzed the in-hospital mortality rate and associated risk factors among HD patients confirmed to have COVID-19. Then, we compared the in-hospital fatality rate and composite outcome between HD patients and non-CKD patients. The composite outcome included in-hospital mortality, ICU admission, or MV application.
Statistical analyses
Statistical analyses were performed using IBM SPSS version 20.0 (IBM Corp., Armonk, NY, USA) and R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria;
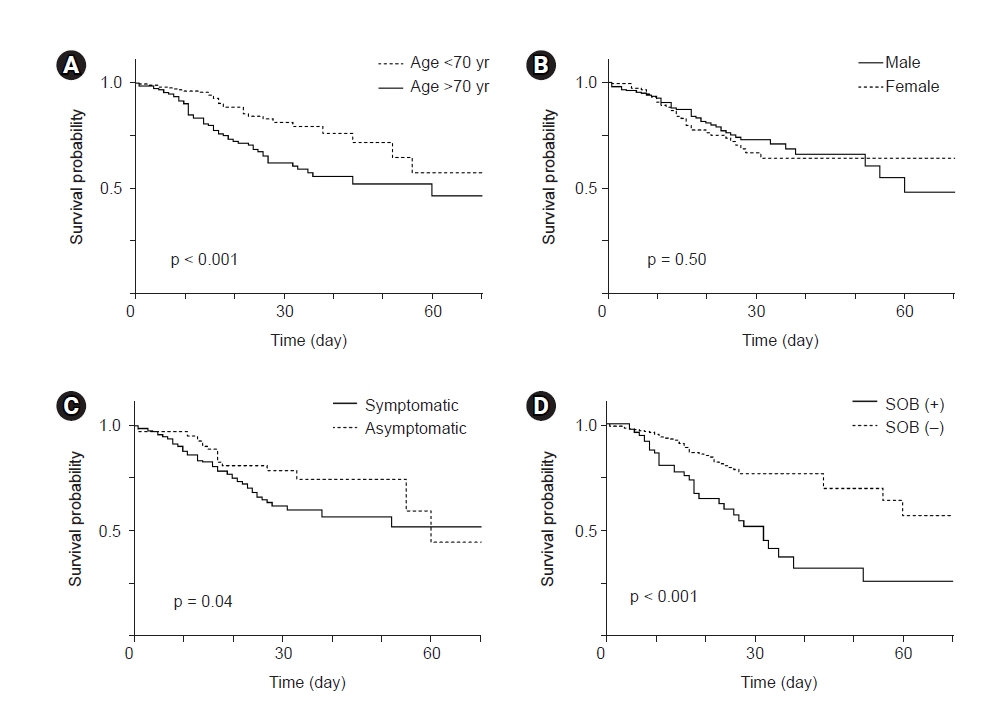
http://www.r-project.org/). The overall in-hospital fatality rate was calculated as the number of fatalities during hospitalization/total number of admitted patients. Clinical factors were compared between survivors and deceased patients using the chi-square test and independent t test. Kaplan-Meier curves were used to show the predicted survival between groups. A Cox proportional hazards model was used to demonstrate independent risk factors for mortality after adjusting other factors. A p-value of <0.05 was considered statistically significant.
To compare the rate of in-hospital fatality and the composite outcome between non-CKD and HD patients, we performed propensity score matching (PSM). Age and sex were used for matching. The HD group was matched with the non-CKD group at a ratio of 1:3. In these matched cohorts, comparisons between groups were conducted with a paired t test, McNemar test, and the Wilcoxon signed-rank test. We conducted a multivariable Cox regression analysis to determine whether HD was an independent risk factor for in-hospital mortality and the composite outcome. Model 1 included only age, sex, and HD, and model 2 included the presence of initial symptoms in addition to the variables included in model 1.
Discussion
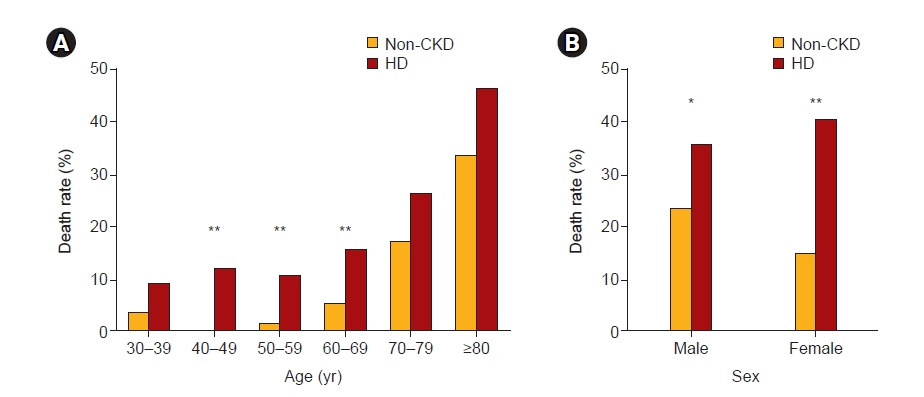
This is the first Korean nationwide cohort study to reveal the mortality risk and associated factors among COVID-19–confirmed HD patients. Our study revealed that the in-hospital fatality rate was higher among HD patients compared to non-CKD patients (22.4% vs. 4.1%). Old age and the presence of shortness of breath at initial presentation were associated with in-hospital fatality among HD patients. After adjusting for patient age and sex, the risk of in-hospital death was 2.1 times higher in HD patients compared to the non-CKD population. HD patients also had a 3.5-fold greater risk of the composite outcome compared to non-CKD patients.
Our study compared the clinical outcomes of HD patients and non-CKD patients hospitalized with COVID-19. Kang et al. [
11] also compared clinical outcomes between CKD and non-CKD patients using Korean national claims data; however, they only included 14 dialysis-dependent CKD patients. Another study by Jung et al. [
12] analyzed outcomes of COVID-19 among patients on in-center HD, but it did not compare outcomes between HD and non-CKD patients. Moreover, these authors also included small numbers of HD patients. Therefore, our study is the first study to report the in-hospital mortality rate and associated factors among a large number of HD patients and to compare their clinical outcome with that of non-CKD patients. A previous investigation from the United States documented a higher in-hospital mortality rate among patients with end-stage renal disease compared to those without it (31.7% vs. 25.4%) [
13]. Another study from China showed that the mortality rate in maintenance HD patients was as high as 39.2% [
14]. Although it is difficult to compare unadjusted mortality rates directly across nations, the lower in-hospital fatality rate among Korean HD patients may be due to strict prevention strategies and pre-symptomatic screening [
1]. In addition, the COVID-19 Task Force Team was established under the Korean Society of Nephrology from the very beginning of the epidemic to prevent secondary transmission of SARS-CoV-2 among HD patients [
9]. The COVID-19 Task Force Team not only published a COVID-19 prevention guideline [
8] but also proposed adequate vaccination and treatment policies to the KDCA, which resulted in lower rates of disease incidence and mortality among HD units [
15].
Previous studies have suggested the proportion of asymptomatic SARS-CoV-2 infection among HD patients is approximately 25% [
16,
17]. Our study demonstrated a higher prevalence of asymptomatic infection (33.9%) compared to previous studies. The reason for the higher prevalence of asymptomatic infection here would be the extensive screening strategy of contact patients or patients under investigation [
8]. Our previous report also demonstrated a higher prevalence of asymptomatic COVID-19 patients in the general population [
18]. Although mortality rates between symptomatic and asymptomatic patients did not differ in the general population (4.5% vs. 3.3%, p = 0.017) [
18], the in-hospital mortality rate was significantly higher for symptomatic patients compared to asymptomatic patients among those receiving HD (HR, 1.727; 95% CI, 1.025–2.912; p = 0.04). As in previous studies, fever (49.5%) and cough (25.7%) were the most common symptoms among HD patients [
5,
19]. Our study revealed that old age and shortness of breath at initial presentation are the primary risk factors for in-hospital mortality among HD patients, while the presence of a sore throat is a protective factor. A recent study by Jang et al. [
20] also demonstrated that dyspnea and altered mental status are high-risk symptoms, while rhinorrhea and headache are low-risk symptoms among patients with COVID-19.
As seen in the general population, old age was the risk factor for patient mortality. Patients aged ≥70 years showed a high mortality rate in both the HD (35.3%) and non-CKD (24.4%) populations (p > 0.05). However, relatively younger patients aged 40 to 69 years showed a higher mortality rate among HD patients compared to the non-CKD population (
Fig. 3A). This may be related to the greater presence of comorbidities, such as diabetes, cerebrovascular disease, or heart failure, among HD patients. Previous studies showed that age and the presence of comorbidities are the two most important risk factors for COVID-19–related mortality [
1,
3]. Unfortunately, we could not adjust comorbidities as the main confounders in our study since we did not collect comorbidity data through the survey.
Previous studies have demonstrated well that male patients experience poorer clinical outcomes compared to female patients [
1,
4,
11]. Unlike in other studies, however, there was no difference in the mortality rate between sexes in our study. The possible explanation for this may be that our female patients were older than our male patients (68.4 ± 13.2 years vs. 64.8 ± 12.8 years, p = 0.009). Therefore, the male and female patients in our cohort may present different baseline characteristics that may diminish the mortality difference between sexes.
Our study has several limitations. First, we collected data using a survey, not via systematic data collection. Therefore, there are much missing data, especially on treatment modality and the presence of symptoms. In addition, we could not calculate the incidence of COVID-19 infection among HD patients since this study was not based on national registry data but instead on results of a self-report survey. Second, we only analyzed the in-hospital mortality rate but not the long-term overall mortality rate. In addition, the period of data collection differed between HD and non-CKD patients (January 2020 to April 2020 for the non-CKD population and February 2020 to November 2021 for HD patients). Since the dominant viral variant changed over time, the overall mortality rate in HD patients may be under-estimated. Third, we did not collect comorbidities or laboratory data, which are known to be major factors affecting patient mortality. Finally, we could not analyze the effect of vaccination since data about individual vaccination history were not collected during the study period.
In conclusion, HD patients have a higher risk of in-hospital mortality and severe COVID-19 outcomes. Older HD patients and those with initial symptoms should be more closely monitored.

















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement 1
Supplement 1 Print
Print















