Zebra bodies in lupus nephritis after hydroxychloroquine therapy
Article information
A 79-year-old woman with a 25-year history of systemic lupus erythematosus, on regular treatment with hydroxychloroquine (HCQ), presented with increasing proteinuria for the past 8 months. Serum creatinine, C3 and C4 were 2.1 mg/dL (reference range, 0.5–1.6 mg/dL), 73 mg/dL (reference range, 60–120 mg/dL), and 20.3 mg/dL (reference range, 15–25 mg/dL), respectively. Antinuclear antibody was positive and anti-double stranded DNA was elevated (65.6 IU/mL). Hematological investigations showed mild anemia and thrombocytopenia (hemoglobin, 10.5 g/dL; platelet count, 132 × 109/L). Twenty-four hour urine protein was in the nephrotic range and a renal biopsy was performed.
Renal biopsy revealed glomeruli displaying mesangial and segmental endocapillary hypercellularity, with glomerular basement membrane thickening (Fig. 1B) and epimembranous argyrophilic spikes on silver staining. Immunofluorescence showed granular capillary wall and mesangial deposits of immunoglobulin G (IgG) (2+), IgM (2+), IgA (1+), C3 (2+), C1q (2+), kappa (1+), and lambda (1+). Renal biopsy revealed lupus nephritis (International Society of Nephrology-Renal Pathology Society [ISN/RPS] classification, III + V). Electron microscopy confirmed the immunohistological diagnosis, with the presence of subepithelial, subendothelial, and mesangial electron-dense deposits, along with numerous zebra bodies (ZBs) in podocyte cytoplasm (Fig. 1A).
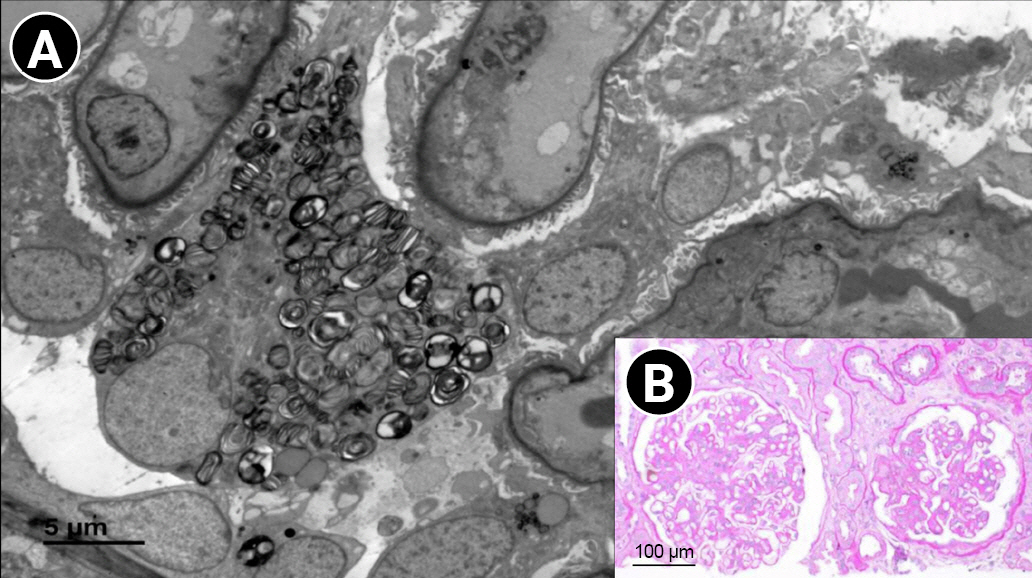
Case of lupus nephritis (ISN/RPS classification, III+V) with zebra bodies on electron microscopy.
(A) Electron microscopy reveals numerous zebra bodies in the podocyte cytoplasm. (B) Periodic acid Schiff staining (×200) displays mesangial hypercellularity and segmental endocapillary hypercellularity, along with thickening of the glomerular basement membrane.
ISN/RPS, International Society of Nephrology-Renal Pathology Society.
ZBs, which are a common characteristic of Fabry disease (FD), also occur in drug-induced phospholipidosis (DIP), usually after chloroquine and HCQ treatment. Electron microscopy is required to diagnose DIP. DIP has fewer ZBs that are smaller in size as compared to FD, and are usually seen in the podocytes alone, rather than in other glomerular and tubular epithelial cells. Recognition of DIP is important for the discontinuation of the implicated drug to prevent further DIP-induced organ damage. Furthermore, differentiation of DIP from FD is essential to avoid expensive life-long enzyme-replacement therapy.
Notes
Conflict of interest
All authors have no conflicts of interest to declare.
Authors’ contributions
Data curation: AS
Conceptualization, Formal analysis, Supervision: VA
Writing–original draft: AS
Writing–review & editing: VA
All authors read and approved the final manuscript.
