1. Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities.
Clin J Am Soc Nephrol 2017;12:2032–2045.


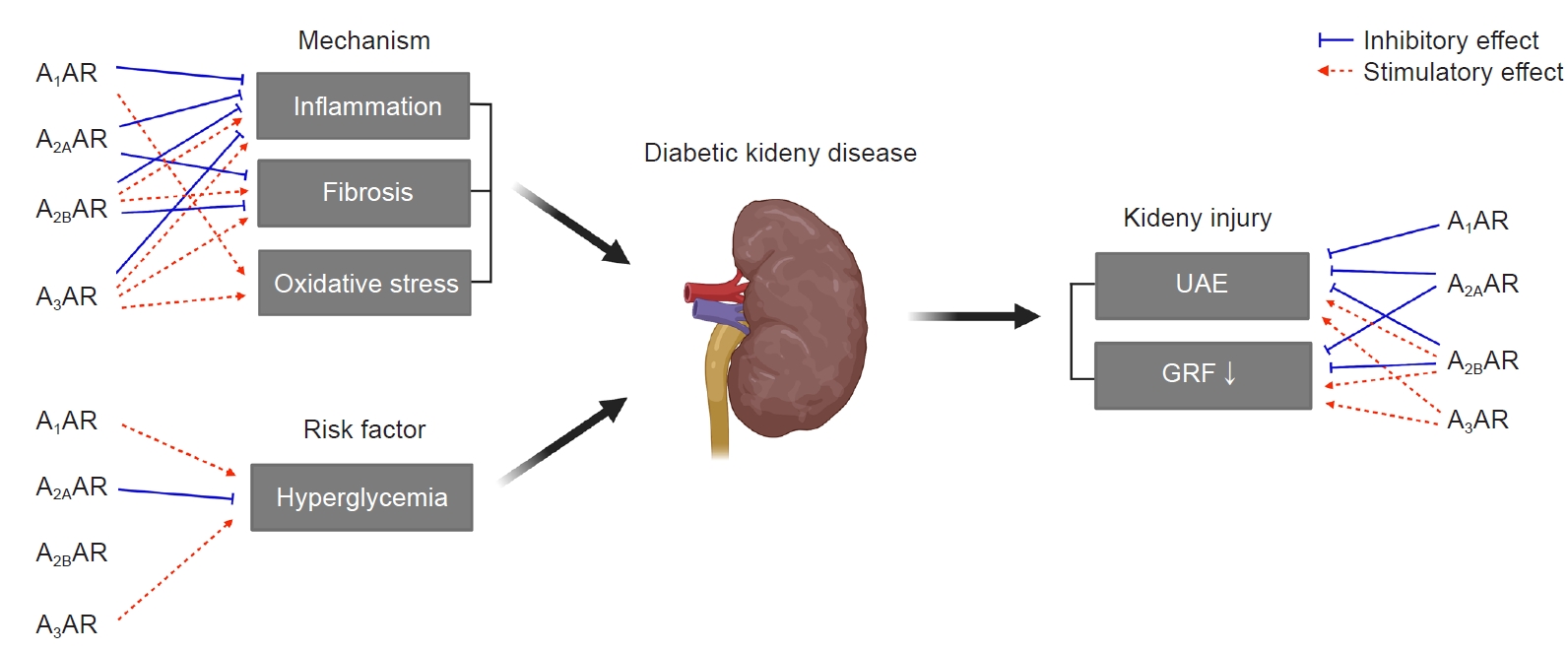
3. Antonioli L, Blandizzi C, Csóka B, Pacher P, Haskó G. Adenosine signalling in diabetes mellitus--pathophysiology and therapeutic considerations.
Nat Rev Endocrinol 2015;11:228–241.



4. Fredholm BB, IJzerman AP, Jacobson KA, Klotz KN, Linden J. International Union of Pharmacology. XXV. Nomenclature and classification of adenosine receptors.
Pharmacol Rev 2001;53:527–552.

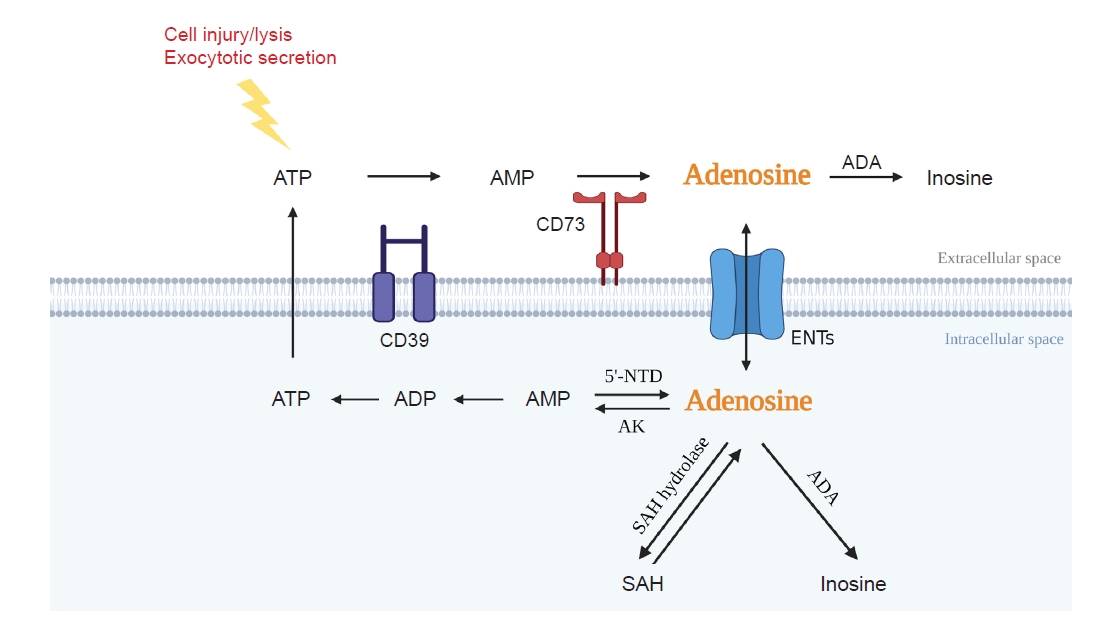
5. Dwyer KM, Kishore BK, Robson SC. Conversion of extracellular ATP into adenosine: a master switch in renal health and disease.
Nat Rev Nephrol 2020;16:509–524.



6. Menzies RI, Tam FW, Unwin RJ, Bailey MA. Purinergic signaling in kidney disease.
Kidney Int 2017;91:315–323.


7. Osswald H, Mühlbauer B, Vallon V. Adenosine and tubuloglomerular feedback.
Blood Purif 1997;15:243–252.



9. Modi AA, Feld JJ, Park Y, et al. Increased caffeine consumption is associated with reduced hepatic fibrosis.
Hepatology 2010;51:201–209.


10. Kim BH, Park YS, Noh HM, Sung JS, Lee JK. Association between coffee consumption and renal impairment in Korean women with and without diabetes: analysis of the fourth Korea National Health and Nutrition Examination Survey in 2008.
Korean J Fam Med 2013;34:265–271.



11. Cronstein BN. Adenosine receptors and fibrosis: a translational review.
F1000 Biol Rep 2011;3:21.



12. Cárdenas A, Toledo C, Oyarzún C, et al. Adenosine A(2B) receptor-mediated VEGF induction promotes diabetic glomerulopathy.
Lab Invest 2013;93:135–144.



13. Awad AS, Huang L, Ye H, et al. Adenosine A2A receptor activation attenuates inflammation and injury in diabetic nephropathy.
Am J Physiol Renal Physiol 2006;290:F828–F837.


14. Persson P, Hansell P, Palm F. Reduced adenosine A2a receptor-mediated efferent arteriolar vasodilation contributes to diabetes-induced glomerular hyperfiltration.
Kidney Int 2015;87:109–115.


15. Persson P, Friederich-Persson M, Fasching A, Hansell P, Inagi R, Palm F. Adenosine A2 a receptor stimulation prevents proteinuria in diabetic rats by promoting an anti-inflammatory phenotype without affecting oxidative stress.
Acta Physiol (Oxf) 2015;214:311–318.


16. Tak E, Ridyard D, Kim JH, et al. CD73-dependent generation of adenosine and endothelial Adora2b signaling attenuate diabetic nephropathy.
J Am Soc Nephrol 2014;25:547–563.


17. Patel L, Thaker A. The effects of adenosine A2B receptor inhibition on VEGF and nitric oxide axis-mediated renal function in diabetic nephropathy.
Ren Fail 2014;36:916–924.

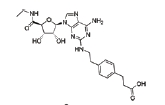
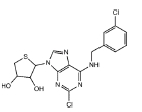
18. Dorotea D, Cho A, Lee G, et al. Orally active, species-independent novel A3 adenosine receptor antagonist protects against kidney injury in db/db mice.
Exp Mol Med 2018;50:1–14.


19. Kretschmar C, Oyarzún C, Villablanca C, et al. Reduced adenosine uptake and its contribution to signaling that mediates profibrotic activation in renal tubular epithelial cells: implication in diabetic nephropathy.
PLoS One 2016;11:e0147430.



20. Garrido W, Jara C, Torres A, et al. Blockade of the adenosine A3 receptor attenuates caspase 1 activation in renal tubule epithelial cells and decreases interleukins IL-1β and IL-18 in diabetic rats.
Int J Mol Sci 2019;20:4531.



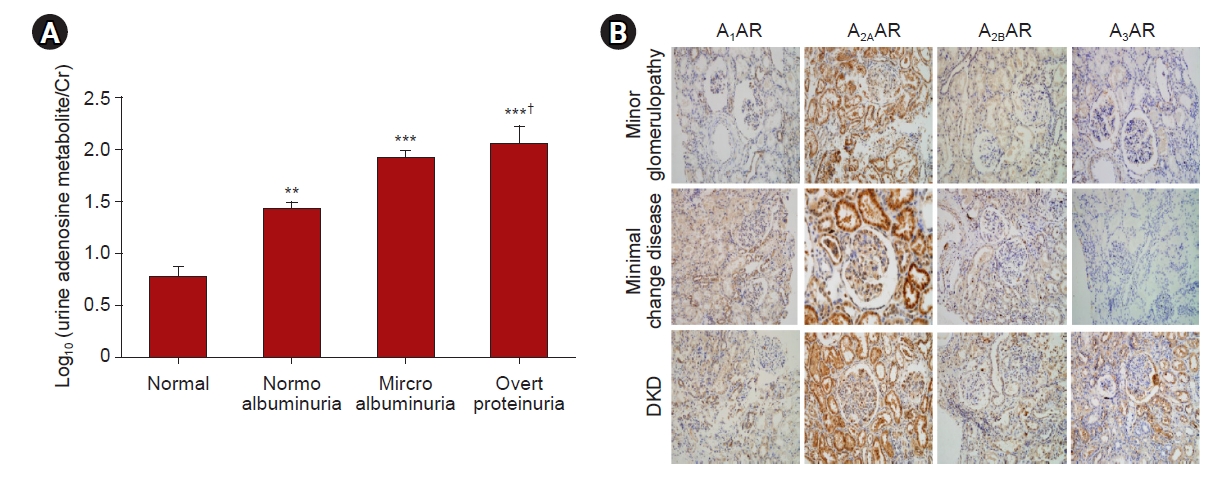
21. Xia JF, Liang QL, Liang XP, et al. Ultraviolet and tandem mass spectrometry for simultaneous quantification of 21 pivotal metabolites in plasma from patients with diabetic nephropathy.
J Chromatogr B Analyt Technol Biomed Life Sci 2009;877:1930–1936.


22. Huang M, Liang Q, Li P, et al. Biomarkers for early diagnosis of type 2 diabetic nephropathy: a study based on an integrated biomarker system.
Mol Biosyst 2013;9:2134–2141.


23. Angielski S, Jakubowski Z, Pawelczyk T, Piec G, Redlak M. Renal handling and metabolism of adenosine in diabetic rats.
Contrib Nephrol 1989;73:52–58.

24. Jacobson KA, Reitman ML. Adenosine-related mechanisms in non-adenosine receptor drugs.
Cells 2020;9:956.



25. Borea PA, Gessi S, Merighi S, Vincenzi F, Varani K. Pharmacology of adenosine receptors: the state of the art.
Physiol Rev 2018;98:1591–1625.


26. Yegutkin GG. Nucleotide- and nucleoside-converting ectoenzymes: important modulators of purinergic signalling cascade.
Biochim Biophys Acta 2008;1783:673–694.


27. Dai Y, Zhang W, Wen J, Zhang Y, Kellems RE, Xia Y. A2B adenosine receptor-mediated induction of IL-6 promotes CKD.
J Am Soc Nephrol 2011;22:890–901.



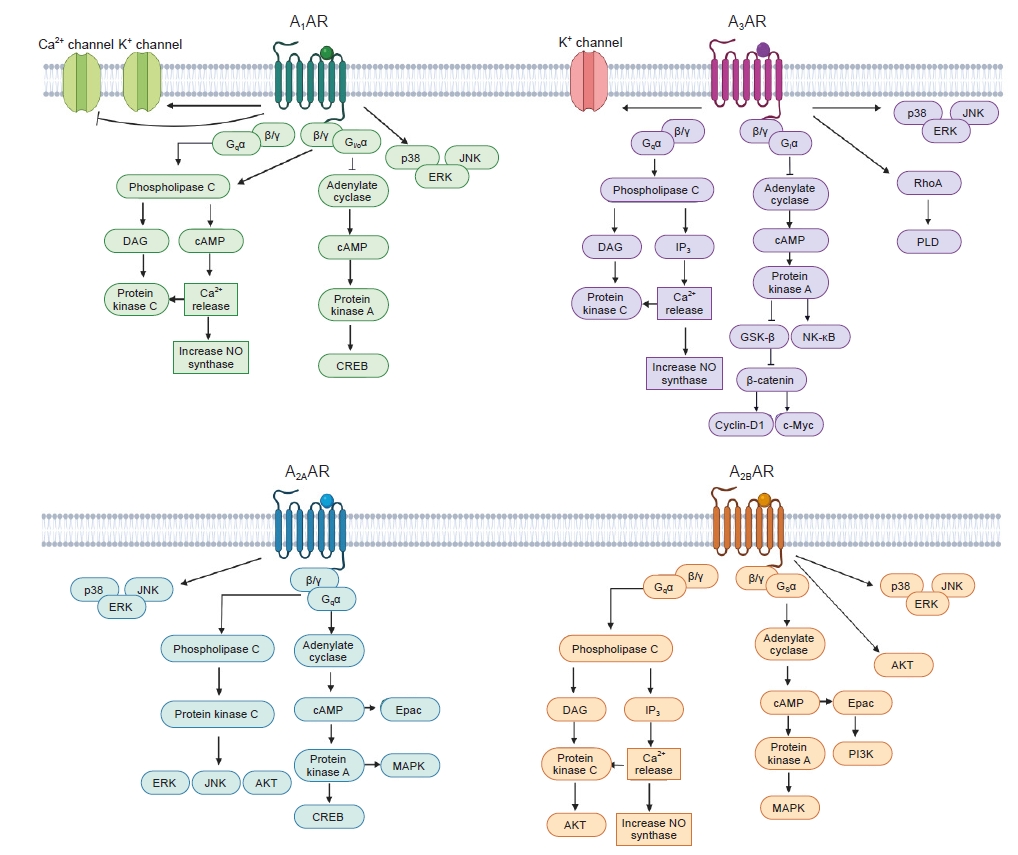
30. Schulte G, Fredholm BB. Signalling from adenosine receptors to mitogen-activated protein kinases.
Cell Signal 2003;15:813–827.


31. Gessi S, Bencivenni S, Battistello E, et al. Inhibition of A2A adenosine receptor signaling in cancer cells proliferation by the novel antagonist TP455.
Front Pharmacol 2017;8:888.



32. Fang Y, Olah ME. Cyclic AMP-dependent, protein kinase A-independent activation of extracellular signal-regulated kinase 1/2 following adenosine receptor stimulation in human umbilical vein endothelial cells: role of exchange protein activated by cAMP 1 (Epac1).
J Pharmacol Exp Ther 2007;322:1189–1200.


33. Ochaion A, Bar-Yehuda S, Cohen S, et al. The A3 adenosine receptor agonist CF502 inhibits the PI3K, PKB/Akt and NF-kappaB signaling pathway in synoviocytes from rheumatoid arthritis patients and in adjuvant-induced arthritis rats.
Biochem Pharmacol 2008;76:482–494.


34. Fishman P, Bar-Yehuda S, Ohana G, et al. An agonist to the A3 adenosine receptor inhibits colon carcinoma growth in mice via modulation of GSK-3 beta and NF-kappa B.
Oncogene 2004;23:2465–2471.



35. Finco DR. Kidney function. In: Kaneko JJ, Harvey JW, Bruss ML, Clinical biochemistry of domestic animals. New York: Academic Press; 1997. p. 441–484.
36. Oyarzún C, Garrido W, Alarcón S, et al. Adenosine contribution to normal renal physiology and chronic kidney disease.
Mol Aspects Med 2017;55:75–89.


37. Vitzthum H, Weiss B, Bachleitner W, Krämer BK, Kurtz A. Gene expression of adenosine receptors along the nephron.
Kidney Int 2004;65:1180–1190.


38. Pawelczyk T, Grden M, Rzepko R, Sakowicz M, Szutowicz A. Region-specific alterations of adenosine receptors expression level in kidney of diabetic rat.
Am J Pathol 2005;167:315–325.



39. Valladares D, Quezada C, Montecinos P, et al. Adenosine A(2B) receptor mediates an increase on VEGF-A production in rat kidney glomeruli.
Biochem Biophys Res Commun 2008;366:180–185.


40. Tang Y, Zhou L. Characterization of adenosine A1 receptors in human proximal tubule epithelial (HK-2) cells.
Recept Channels 2003;9:67–75.


41. Al-Mashhadi RH, Skøtt O, Vanhoutte PM, Hansen PB. Activation of A(2) adenosine receptors dilates cortical efferent arterioles in mouse.
Kidney Int 2009;75:793–799.


42. Park J, Shrestha R, Qiu C, et al. Single-cell transcriptomics of the mouse kidney reveals potential cellular targets of kidney disease.
Science 2018;360:758–763.



43. Wilson RF, Wyche K, Christensen BV, Zimmer S, Laxson DD. Effects of adenosine on human coronary arterial circulation.
Circulation 1990;82:1595–1606.


44. Marraccini P, Fedele S, Marzilli M, et al. Adenosine-induced renal vasoconstriction in man.
Cardiovasc Res 1996;32:949–953.


45. Osswald H. Renal effects of adenosine and their inhibition by theophylline in dogs.
Naunyn Schmiedebergs Arch Pharmacol 1975;288:79–86.



46. Jackson EK, Zhu C, Tofovic SP. Expression of adenosine receptors in the preglomerular microcirculation.
Am J Physiol Renal Physiol 2002;283:F41–F51.


47. Lu Y, Zhang R, Ge Y, et al. Identification and function of adenosine A3 receptor in afferent arterioles.
Am J Physiol Renal Physiol 2015;308:F1020–F1025.



48. Vallon V, Mühlbauer B, Osswald H. Adenosine and kidney function.
Physiol Rev 2006;86:901–940.


49. Vallon V, Osswald H. Adenosine receptors and the kidney.
Handb Exp Pharmacol 2009;2009:443–470.

50. Spielman WS, Osswald H. Characterization of the postocclusive response of renal blood flow in the cat.
Am J Physiol 1978;235:F286–F290.


51. Osswald H, Spielman WS, Knox FG. Mechanism of adenosine-mediated decreases in glomerular filtration rate in dogs.
Circ Res 1978;43:465–469.


52. Aki Y, Tomohiro A, Nishiyama A, Kiyomoto K, Kimura S, Abe Y. Effects of KW-3902, a selective and potent adenosine A1 receptor antagonist, on renal hemodynamics and urine formation in anesthetized dogs.
Pharmacology 1997;55:193–201.


53. Hansen PB, Hashimoto S, Oppermann M, Huang Y, Briggs JP, Schnermann J. Vasoconstrictor and vasodilator effects of adenosine in the mouse kidney due to preferential activation of A1 or A2 adenosine receptors.
J Pharmacol Exp Ther 2005;315:1150–1157.


54. Cook CB, Churchill PC. Effects of renal denervation on the renal responses of anesthetized rats to cyclohexyladenosine.
Can J Physiol Pharmacol 1984;62:934–938.


55. Weihprecht H, Lorenz JN, Briggs JP, Schnermann J. Vasomotor effects of purinergic agonists in isolated rabbit afferent arterioles.
Am J Physiol 1992;263:F1026–F1033.


56. Levens N, Beil M, Schulz R. Intrarenal actions of the new adenosine agonist CGS 21680A, selective for the A2 receptor.
J Pharmacol Exp Ther 1991;257:1013–1019.

57. Zou AP, Nithipatikom K, Li PL, Cowley AW Jr. Role of renal medullary adenosine in the control of blood flow and sodium excretion.
Am J Physiol 1999;276:R790–R798.


58. Agmon Y, Dinour D, Brezis M. Disparate effects of adenosine A1- and A2-receptor agonists on intrarenal blood flow.
Am J Physiol 1993;265:F802–F806.


59. Hansen PB, Castrop H, Briggs J, Schnermann J. Adenosine induces vasoconstriction through Gi-dependent activation of phospholipase C in isolated perfused afferent arterioles of mice.
J Am Soc Nephrol 2003;14:2457–2465.


60. Hansen PB, Friis UG, Uhrenholt TR, Briggs J, Schnermann J. Intracellular signalling pathways in the vasoconstrictor response of mouse afferent arterioles to adenosine.
Acta Physiol (Oxf) 2007;191:89–97.


61. Okumura M, Miura K, Yamashita Y, Yukimura T, Yamamoto K. Role of endothelium-derived relaxing factor in the in vivo renal vascular action of adenosine in dogs.
J Pharmacol Exp Ther 1992;260:1262–1267.

62. Arulkumaran N, Turner CM, Sixma ML, Singer M, Unwin R, Tam FW. Purinergic signaling in inflammatory renal disease.
Front Physiol 2013;4:194.



63. Thomson S, Bao D, Deng A, Vallon V. Adenosine formed by 5’-nucleotidase mediates tubuloglomerular feedback.
J Clin Invest 2000;106:289–298.



64. Sällström J, Carlsson PO, Fredholm BB, Larsson E, Persson AE, Palm F. Diabetes-induced hyperfiltration in adenosine A(1)-receptor deficient mice lacking the tubuloglomerular feedback mechanism.
Acta Physiol (Oxf) 2007;190:253–259.


65. Vallon V, Richter K, Huang DY, Rieg T, Schnermann J. Functional consequences at the single-nephron level of the lack of adenosine A1 receptors and tubuloglomerular feedback in mice.
Pflugers Arch 2004;448:214–221.



66. Ren Y, Garvin JL, Carretero OA. Efferent arteriole tubuloglomerular feedback in the renal nephron.
Kidney Int 2001;59:222–229.


67. Tagawa H, Vander AJ. Effects of adenosine compounds on renal function and renin secretion in dogs.
Circ Res 1970;26:327–338.


68. Jackson EK. Adenosine: a physiological brake on renin release.
Annu Rev Pharmacol Toxicol 1991;31:1–35.


69. Schweda F, Wagner C, Krämer BK, Schnermann J, Kurtz A. Preserved macula densa-dependent renin secretion in A1 adenosine receptor knockout mice.
Am J Physiol Renal Physiol 2003;284:F770–F777.


70. Churchill PC, Bidani A. Renal effects of selective adenosine receptor agonists in anesthetized rats.
Am J Physiol 1987;252:F299–F303.


71. Oyarzún C, Salinas C, Gómez D, et al. Increased levels of adenosine and ecto 5'-nucleotidase (CD73) activity precede renal alterations in experimental diabetic rats.
Biochem Biophys Res Commun 2015;468:354–359.


72. San Martín R, Valladares D, Roa H, Troncoso E, Sobrevia L. Do adenosine receptors offer new therapeutic options for diabetic nephropathy?
Curr Vasc Pharmacol 2009;7:450–459.


73. Pawelczyk T, Sakowicz M, Szczepanska-Konkel M, Angielski S. Decreased expression of adenosine kinase in streptozotocin-induced diabetes mellitus rats.
Arch Biochem Biophys 2000;375:1–6.


74. Sakowicz M, Pawelczyk T. Insulin restores expression of adenosine kinase in streptozotocin-induced diabetes mellitus rats.
Mol Cell Biochem 2002;236:163–171.

75. Pye C, Elsherbiny NM, Ibrahim AS, et al. Adenosine kinase inhibition protects the kidney against streptozotocin-induced diabetes through anti-inflammatory and anti-oxidant mechanisms.
Pharmacol Res 2014;85:45–54.



76. Elsherbiny NM, Al-Gayyar MM, Abd El Galil KH. Nephroprotective role of dipyridamole in diabetic nephropathy: effect on inflammation and apoptosis.
Life Sci 2015;143:8–17.


77. Taşkıran E, Erbaş O, Yiğittürk G, Meral A, Akar H, Taşkıran D. Exogenously administered adenosine attenuates renal damage in streptozotocin-induced diabetic rats.
Ren Fail 2016;38:1276–1282.


78. Faulhaber-Walter R, Chen L, Oppermann M, et al. Lack of A1 adenosine receptors augments diabetic hyperfiltration and glomerular injury.
J Am Soc Nephrol 2008;19:722–730.



79. Lee HT, Ota-Setlik A, Xu H, D’Agati VD, Jacobson MA, Emala CW. A3 adenosine receptor knockout mice are protected against ischemia- and myoglobinuria-induced renal failure.
Am J Physiol Renal Physiol 2003;284:F267–F273.


80. Pareek A, Chandurkar N, Naidu K. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 2016;375:1800.
81. Morita M, Kanasaki K. Sodium-glucose cotransporter-2 inhibitors for diabetic kidney disease: targeting Warburg effects in proximal tubular cells.
Diabetes Metab 2020;46:353–361.


82. Thomson SC, Rieg T, Miracle C, et al. Acute and chronic effects of SGLT2 blockade on glomerular and tubular function in the early diabetic rat.
Am J Physiol Regul Integr Comp Physiol 2012;302:R75–R83.


83. Rajasekeran H, Lytvyn Y, Bozovic A, et al. Urinary adenosine excretion in type 1 diabetes.
Am J Physiol Renal Physiol 2017;313:F184–F191.


84. Vallon V, Osswald H. Dipyridamole prevents diabetes-induced alterations of kidney function in rats.
Naunyn Schmiedebergs Arch Pharmacol 1994;349:217–222.



85. Bigotte Vieira M, Magriço R, Viegas Dias C, Leitão L, Neves JS. Caffeine consumption and mortality in chronic kidney disease: a nationally representative analysis.
Nephrol Dial Transplant 2019;34:974–980.



86. Tang J, Jiang X, Zhou Y, Xia B, Dai Y. Increased adenosine levels contribute to ischemic kidney fibrosis in the unilateral ureteral obstruction model.
Exp Ther Med 2015;9:737–743.



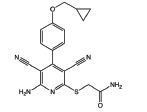
87. Lee J, Hwang I, Lee JH, Lee HW, Jeong LS, Ha H. The selective A3AR antagonist LJ-1888 ameliorates UUO-induced tubulointerstitial fibrosis.
Am J Pathol 2013;183:1488–1497.


88. Lee HT, Kim M, Joo JD, Gallos G, Chen JF, Emala CW. A3 adenosine receptor activation decreases mortality and renal and hepatic injury in murine septic peritonitis.
Am J Physiol Regul Integr Comp Physiol 2006;291:R959–R969.


89. Haskó G, Pacher P. A2A receptors in inflammation and injury: lessons learned from transgenic animals.
J Leukoc Biol 2008;83:447–455.



90. Day YJ, Huang L, McDuffie MJ, et al. Renal protection from ischemia mediated by A2A adenosine receptors on bone marrow-derived cells.
J Clin Invest 2003;112:883–891.



91. Day YJ, Huang L, Ye H, Linden J, Okusa MD. Renal ischemia-reperfusion injury and adenosine 2A receptor-mediated tissue protection: role of macrophages.
Am J Physiol Renal Physiol 2005;288:F722–F731.


92. Garcia GE, Truong LD, Chen JF, Johnson RJ, Feng L. Adenosine A(2A) receptor activation prevents progressive kidney fibrosis in a model of immune-associated chronic inflammation.
Kidney Int 2011;80:378–388.


93. Xiao H, Shen HY, Liu W, et al. Adenosine A2A receptor: a target for regulating renal interstitial fibrosis in obstructive nephropathy.
PLoS One 2013;8:e60173.



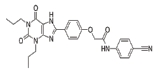
94. Pak ES, Jeong LS, Hou X, Tripathi SK, Lee J, Ha H. Dual actions of A2A and A3 adenosine receptor ligand prevents obstruction-induced kidney fibrosis in mice.
Int J Mol Sci 2021;22:5667.



95. Wilkinson PF, Farrell FX, Morel D, Law W, Murphy S. Adenosine signaling increases proinflammatory and profibrotic mediators through activation of a functional adenosine 2B receptor in renal fibroblasts.
Ann Clin Lab Sci 2016;46:339–345.

96. Lee HT, Gallos G, Nasr SH, Emala CW. A1 adenosine receptor activation inhibits inflammation, necrosis, and apoptosis after renal ischemia-reperfusion injury in mice.
J Am Soc Nephrol 2004;15:102–111.


97. Lee HT, Xu H, Nasr SH, Schnermann J, Emala CW. A1 adenosine receptor knockout mice exhibit increased renal injury following ischemia and reperfusion.
Am J Physiol Renal Physiol 2004;286:F298–F306.


98. Kim JY, Kim M, Ham A, et al. IL-11 is required for A1 adenosine receptor-mediated protection against ischemic AKI.
J Am Soc Nephrol 2013;24:1558–1570.



99. Ha H, Hwang IA, Park JH, Lee HB. Role of reactive oxygen species in the pathogenesis of diabetic nephropathy.
Diabetes Res Clin Pract 2008;82 Suppl 1:S42–S45.


100. Bae YS, Choi MK, Lee WJ. Dual oxidase in mucosal immunity and host-microbe homeostasis.
Trends Immunol 2010;31:278–287.


102. Yang T, Gao X, Sandberg M, et al. Abrogation of adenosine A1 receptor signalling improves metabolic regulation in mice by modulating oxidative stress and inflammatory responses.
Diabetologia 2015;58:1610–1620.



103. Yang T, Zollbrecht C, Winerdal ME, et al. Genetic abrogation of adenosine A3 receptor prevents uninephrectomy and high salt-induced hypertension.
J Am Heart Assoc 2016;5:e003868.



104. Kagami K, Morita H, Onda K, Hirano T, Oka K. Protective effect of caffeine on streptozotocin-induced beta-cell damage in rats.
J Pharm Pharmacol 2008;60:1161–1165.



105. Zywert A, Szkudelska K, Szkudelski T. Effects of adenosine A(1) receptor antagonism on insulin secretion from rat pancreatic islets.
Physiol Res 2011;60:905–911.


106. Johansson SM, Salehi A, Sandström ME, et al. A1 receptor deficiency causes increased insulin and glucagon secretion in mice.
Biochem Pharmacol 2007;74:1628–1635.


107. Ohtani M, Oka T, Ohura K. Possible involvement of A₂A and A₃ receptors in modulation of insulin secretion and β-cell survival in mouse pancreatic islets.
Gen Comp Endocrinol 2013;187:86–94.

108. Chhabra P, Wang K, Zeng Q, et al. Adenosine A(2A) agonist administration improves islet transplant outcome: evidence for the role of innate immunity in islet graft rejection.
Cell Transplant 2010;19:597–612.
















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















