| Kidney Res Clin Pract > Volume 41(5); 2022 > Article |
|
Abstract
Background
Methods
Results
Notes
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2020R1F1A1049799).
Authors’ contributions
Conceptualization: TK, YK, ME
Data curation: YK, JYL, HS
Formal analysis: TK, JYL, HS, ME
Funding acquisition, Methodology, Project administration, Resources, Supervision: ME
Validation: ME, JSK, JWY
Writing–original draft: TK, JYL
Writing–review & editing: all authors
All authors read and approved the final manuscript.
Figure 1.
Microscopic findings of representative pathological prognostic factors of diabetic nephropathy.
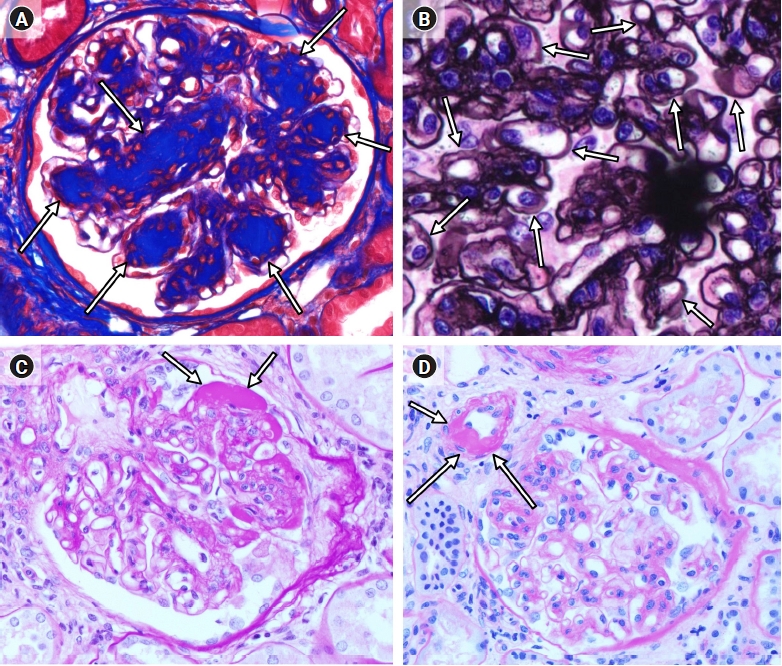
Figure 2.
Microscopic findings of a laminated nodule and capillary microaneurysm.

Figure 3.
Receiver operating characteristic curve for the prediction of renal injury requiring renal replacement therapy.

Table 1.
| Characteristics | RRT+ | RRT– | p-value |
|---|---|---|---|
| No. of patients | 56 | 37 | |
| Age (yr) | 48.29 ± 11.86 | 54.97 ± 10.80 | 0.007* |
| Sex | 0.33 | ||
| Male | 43 (76.8) | 25 (67.6) | |
| Female | 13 (23.2) | 12 (32.4) | |
| Type of diabetes | 0.50 | ||
| I | 5 (8.9) | 2 (5.4) | |
| II | 46 (82.1) | 33 (89.2) | |
| Unknown | 5 (8.9) | 2 (5.4) | |
| Diabetes duration (yr) | 9.94 ± 5.89 | 10.94 ± 7.77 | 0.51 |
| RPS glomerular class | 0.01* | ||
| I | 1 (1.8) | 4 (10.8) | |
| IIa + IIb | 9 (16.1) | 14 (37.8) | |
| III | 27 (48.2) | 10 (27.0) | |
| IV | 19 (33.9) | 9 (24.3) | |
| RPS glomerular class | 3.14 ± 0.75 | 2.65 ± 0.98 | 0.01* |
| JRPS classification grade | 0.06 | ||
| 1 | 1 (1.8) | 3 (8.1) | |
| 2 | 2 (3.6) | 6 (16.2) | |
| 3 | 27 (48.2) | 13 (35.1) | |
| 4 | 26 (46.4) | 15 (40.5) | |
| JRPS classification grade | 3.39 ± 0.65 | 3.08 ± 0.95 | 0.09 |
| J-score | 14.23 ± 2.84 | 12.57 ± 4.66 | 0.06 |
| Baseline eGFR (mL/min/1.73 m2) | 31.61 ± 30.53 | 58.42 ± 39.00 | <0.001* |
Data are expressed as number only, mean ± standard deviation, or number (%).
JRPS classification grade: 1, J-score of 0–5; 2, J-score of 6–10; 3, J-score of 11–15; 4, J-score of 16–19.
JRPS, Japanese Renal Pathology Society; J-score, JRPS score; RPS, Renal Pathology Society; RRT+, received renal replacement therapy; RRT, did not receive renal replacement therapy.
Table 2.
| Parameter |
Pearson correlation coefficient (r) |
|||||
|---|---|---|---|---|---|---|
| Creatinine | eGFR | HbA1c | 24-hr TP | 24-hr Malb | CKD stage | |
| JPRS score (1–19) | –0.090 | –0.472*** | 0.067 | –0.057 | –0.134 | 0.284** |
| Diffuse lesion (0–3) | 0.153 | –0.243* | 0.276* | 0.132 | –0.201 | 0.115 |
| Nodular lesion (0, 1) | 0.203 | –0.298** | 0.16 | 0.074 | 0.039 | 0.210* |
| GBM doubling (0–3) | 0.207* | –0.301** | –0.161 | –0.164 | –0.212* | 0.190 |
| Mesangiolysis (0, 1) | 0.219* | –0.273** | 0.028 | –0.035 | –0.085 | 0.089 |
| Exudative lesion (0, 1) | 0.284** | –0.385*** | 0.003 | 0.103 | 0.056 | 0.402*** |
| Polar vasculosis (0, 1) | 0.078 | –0.247* | 0.026 | –0.054 | –0.098 | 0.109 |
| Global glomerulosclerosis (%) | 0.314** | –0.393*** | –0.130 | 0.056 | 0.043 | 0.425*** |
| Glomerulomegaly (0, 1) | –0.136 | 0.091 | 0.002 | 0.08 | 0.074 | –0.137 |
| IFTA (0–3) | 0.494*** | –0.587*** | –0.187 | 0.002 | –0.090 | 0.432*** |
| Interstitial inflammation (0–3) | 0.355*** | –0.508*** | –0.151 | 0.130 | –0.050 | 0.424*** |
| Arteriolar hyalinosis (0–3) | 0.053 | –0.093 | 0.169 | 0.024 | –0.019 | –0.056 |
| Intimal thickening (0–2) | 0.171 | –0.225* | –0.152 | –0.116 | –0.166 | 0.070 |
Table 3.
| Parameter | Creatinine (mg/dL) | eGFR (mL/min/1.73m2) | HbA1c (%) | 24-hr TP (mg/day) | 24-hr Malb (mg/day) | CKD stage |
|---|---|---|---|---|---|---|
| Microaneurysm | ||||||
| – | 3.46 ± 0.34 | 42.98 ± 37.60 | 8.23 ± 2.65 | 4,266.88 ± 460.11 | 4,563.75 ± 2,971.81 | 2.65 ± 0.60 |
| + | 2.50 ± 1.09 | 33.67 ± 14.71 | 8.20 ± 1.96 | 4,079.73 ± 1,541.99 | 5,393.23 ± 2,876.17 | 2.57 ± 0.79 |
| Laminated nodule | ||||||
| – | 3.30 ± 3.08 | 45.64 ± 38.69** | 8.21 ± 2.69 | 6,351.27 ± 4,307.26 | 4,469.40 ± 3,018.43 | 2.62 ± 0.59 |
| + | 3.84 ± 2.93 | 26.10 ± 14.72** | 8.29 ± 2.16 | 7,763.85 ± 3,886.59 | 5,380.74 ± 2,599.26 | 2.75 ± 0.68 |
Table 4.
| Parameter | Grade or score (n) | Odds ratio (95% CI) | p-value |
|---|---|---|---|
| JRPS grade | Grade 1, 2 (12) vs. 3, 4 (81) | 0.14 (0.03–0.68) | 0.02* |
| RPS glomerular class | Grade 1, 2 (27) vs. 3, 4 (66) | 0.83 (0.34–2.07) | 0.69 |
| Diffuse lesion | Score 0–2 (22) vs. 3 (71) | 0.15 (0.02–1.35) | 0.09 |
| Nodular lesion | Score 0 (43) vs. 1 (50) | 0.79 (0.35–1.79) | 0.57 |
| GBM doubling | Score 0–2 (85) vs. 3 (8) | 1.25 (0.26–6.03) | 0.78 |
| Mesangiolysis | Score 0–2 (52) vs. 3 (41) | 1.98 (0.86–4.56) | 0.11 |
| Exudative lesion | Score 0 (31) vs. 1 (62) | 0.82 (0.34–1.97) | 0.66 |
| Polar vasculosis | Score 0 (16) vs. 1 (77) | 0.85 (0.29–2.51) | 0.77 |
| Glomerulomegaly | Score 0 (75) vs. 1 (18) | 1.55 (0.55–4.38) | 0.41 |
| Arteriolar hyalinosis | Score 0–2 (64) vs. 3 (29) | 0.43 (0.07–2.76) | 0.38 |
| Intimal thickness | Score 0-1 (41) vs. 2 (52) | 1.88 (0.54–6.54) | 0.32 |
| Microaneurysm | Score 0 (86) vs. 1 (7) | 0.84 (0.18–4.00) | 0.83 |
| Laminated nodule | Score 0 (77) vs. 1 (16) | 0.86 (0.29–2.56) | 0.79 |
Table 5.
| Parameter | Grade or score (n) | Odds ratio (95% CI) | p-value |
|---|---|---|---|
| JRPS grade | Grade 1, 2 (12) vs. 3, 4 (81) | 5.68 (1.42–22.68) | 0.01* |
| RPS glomerular class | Grade 1, 2 (27) vs. 3, 4 (66) | 4.60 (1.56–13.54) | 0.006** |
| Diffuse lesion | Score 0–2 (22) vs. 3 (71) | 9.43 (0.91–98.05) | 0.06 |
| Nodular lesion | Score 0 (43) vs. 1 (50) | 4.77 (1.60–14.24) | 0.005** |
| GBM doubling | Score 0–2 (85) vs. 3 (8) | 1.04 (0.17–6.29) | 0.97 |
| Mesangiolysis | Score 0–2 (52) vs. 3 (41) | 1.77 (0.62–5.06) | 0.28 |
| Exudative lesion | Score 0 (31) vs. 1 (62) | 3.08 (1.08–8.74) | 0.04* |
| Polar vasculosis | Score 0 (16) vs. 1 (77) | 1.93 (0.54–6.92) | 0.31 |
| Glomerulomegaly | Score 0 (75) vs. 1 (18) | 0.92 (0.25–3.38) | 0.90 |
| Arteriolar hyalinosis | Score 0–2 (64) vs. 3 (29) | 3.80 (0.42–34.08) | 0.23 |
| Intimal thickness | Score 0-1 (41) vs. 2 (52) | 0.44 (0.08–2.36) | 0.34 |
| Microaneurysm | Score 0 (86) vs. 1 (7) | 0.87 (0.18–4.14) | 0.86 |
| Laminated nodule | Score 0 (77) vs. 1 (16) | 3.43 (0.90–13.00) | 0.07 |
Table 6.
| Parameter | Grade or score (n) | Odds ratio (95% CI) | p-value |
|---|---|---|---|
| JRPS grade | Grade 1, 2 (12) vs. 3, 4 (81) | 6.25 (2.31–16.95) | <0.001*** |
| RPS glomerular class | Grade 1, 2 (27) vs. 3, 4 (66) | 4.57 (1.30–16.07) | 0.02* |
| Diffuse lesion | Score 0–2 (22) vs. 3 (71) | 12.75 (1.40–116.04) | 0.02* |
| Nodular lesion | Score 0 (43) vs. 1 (50) | 2.98 (1.16–7.67) | 0.02* |
| GBM doubling | Score 0–2 (85) vs. 3 (8) | 4.96 (0.56–44.10) | 0.15 |
| Mesangiolysis | Score 0–2 (52) vs. 3 (41) | 1.73 (0.68–4.42) | 0.25 |
| Exudative lesion | Score 0 (31) vs. 1 (62) | 5.55 (2.09–14.73) | 0.001** |
| Polar vasculosis | Score 0 (16) vs. 1 (77) | 1.71 (0.55–5.31) | 0.35 |
| Glomerulomegaly | Score 0 (75) vs. 1 (18) | 0.53 (0.18–1.57) | 0.25 |
| Arteriolar hyalinosis | Score 0–2 (64) vs. 3 (29) | 0.53 (0.05–5.22) | 0.58 |
| Intimal thickness | Score 0-1 (41) vs. 2 (52) | 2.06 (0.59–7.15) | 0.26 |
| Microaneurysm | Score 0 (86) vs. 1 (7) | 0.97 (0.18–5.33) | 0.97 |
| Laminated nodule | Score 0 (77) vs. 1 (16) | 3.17 (0.67–15.56) | 0.15 |
Table 7.
| Adjustment | Parameter | Odds ratio (95% CI) | p-value |
|---|---|---|---|
| Age, sex, BMI, HbA1c, DM duration, and hypertension | JRPS grade | 20.44(2.82–148.10) | 0.003** |
| Nodular lesion | 4.98(1.40–17.75) | 0.013* | |
| Exudative lesion | 11.26(2.88–44.05) | 0.001** |
References
-
METRICS

- ORCID iDs
-
Taeyeong Kim

https://orcid.org/0000-0002-6140-3669Yooujin Kwak

https://orcid.org/0000-0002-4295-6452Jun Young Lee

https://orcid.org/0000-0001-8047-4190Hanwul Shin

https://orcid.org/0000-0003-3863-5434Jae Seok Kim

https://orcid.org/0000-0002-1350-3526Jae Won Yang

https://orcid.org/0000-0003-3689-5865Minseob Eom

https://orcid.org/0000-0002-8121-8399 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















