1. Cho MH. Renal fibrosis.
Korean J Pediatr 2010;53:735–740.



2. Shu DY, Lovicu FJ. Myofibroblast transdifferentiation: the dark force in ocular wound healing and fibrosis.
Prog Retin Eye Res 2017;60:44–65.



3. Jang HS, Kim JI, Han SJ, Park KM. Recruitment and subsequent proliferation of bone marrow-derived cells in the postischemic kidney are important to the progression of fibrosis.
Am J Physiol Renal Physiol 2014;306:F1451–F1461.


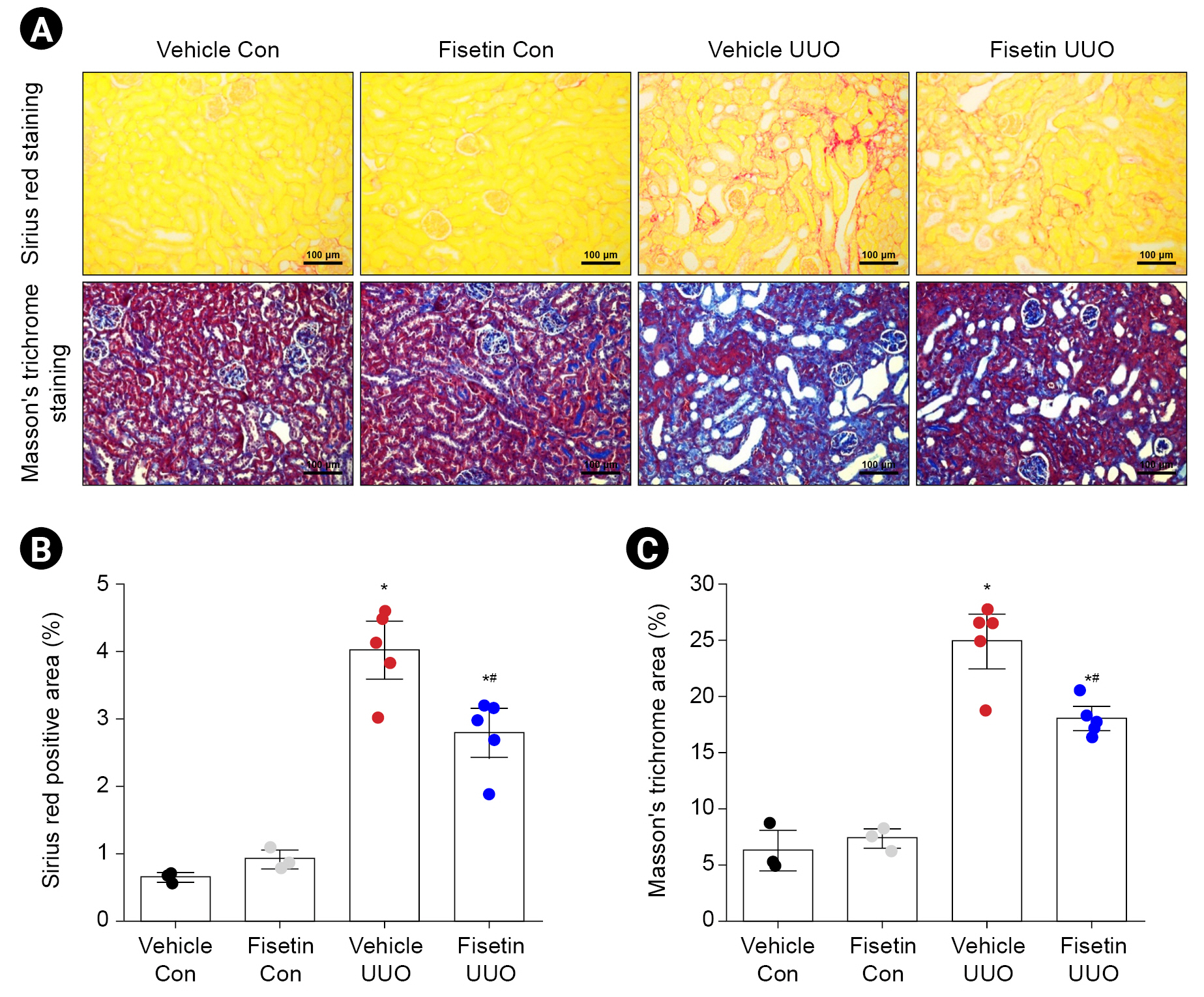
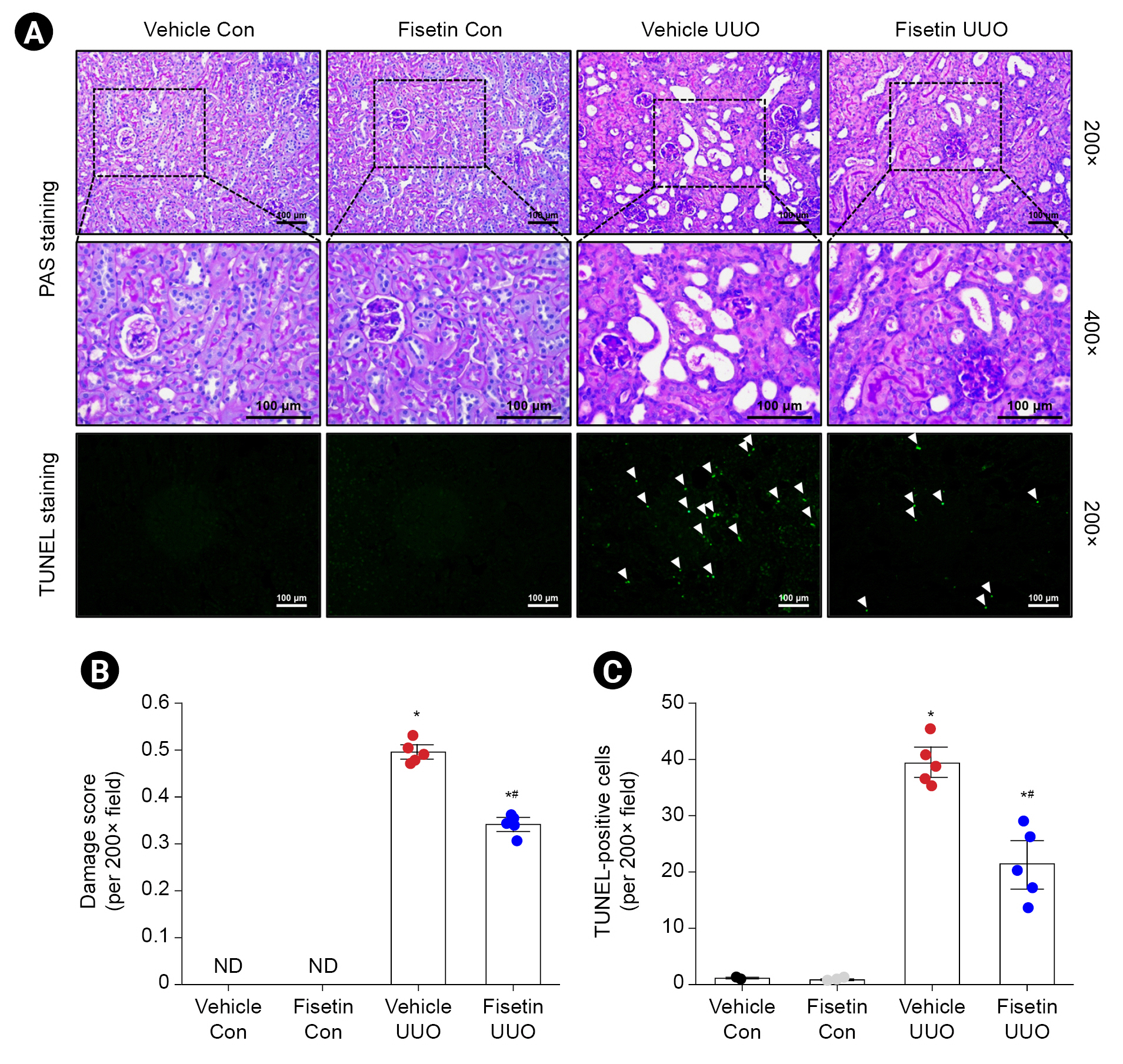
4. Chevalier RL, Forbes MS, Thornhill BA. Ureteral obstruction as a model of renal interstitial fibrosis and obstructive nephropathy.
Kidney Int 2009;75:1145–1152.


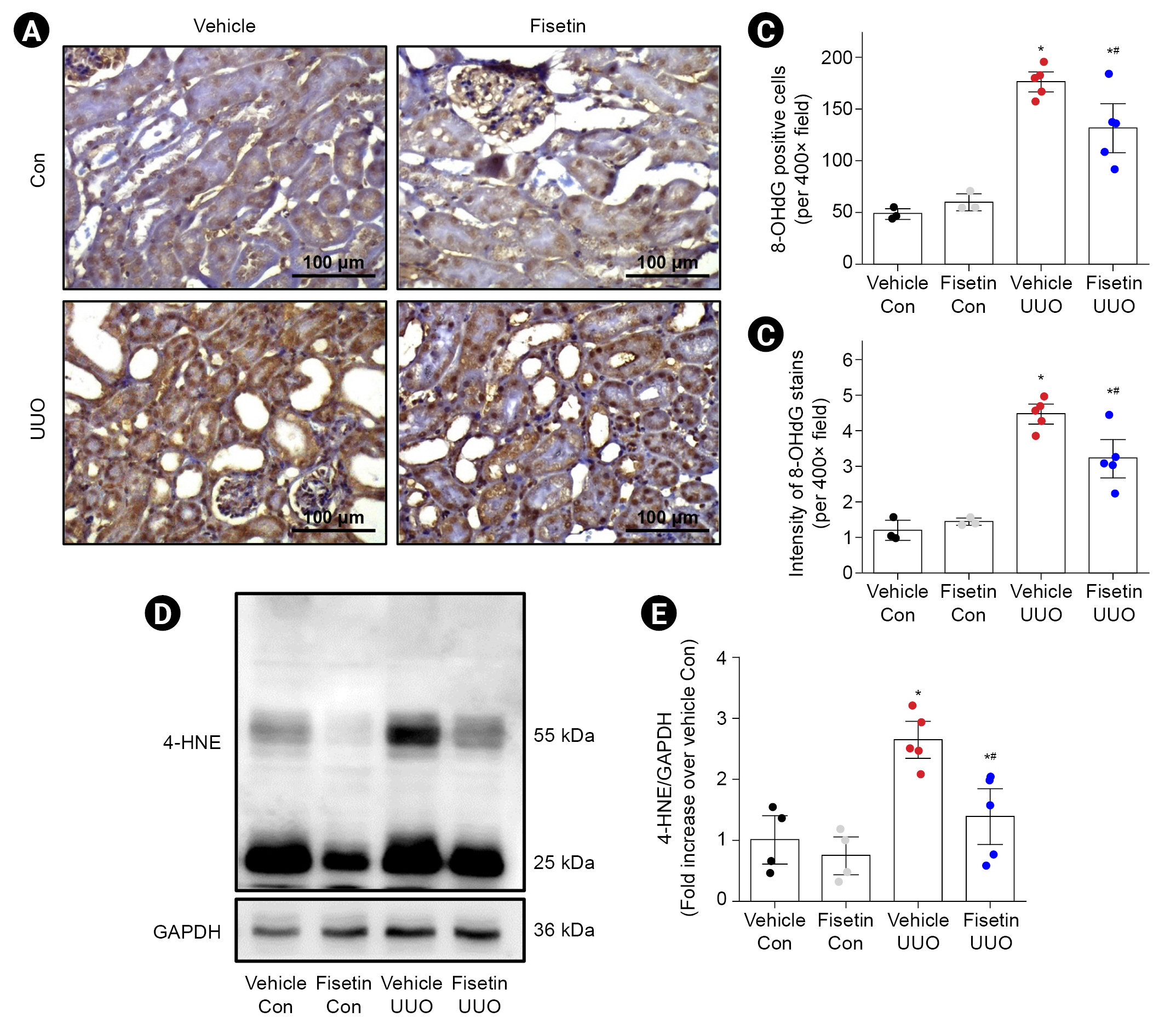
5. Dendooven A, Ishola DA, Nguyen TQ, et al. Oxidative stress in obstructive nephropathy.
Int J Exp Pathol 2011;92:202–210.



6. Pal HC, Pearlman RL, Afaq F. Fisetin and its role in chronic diseases.
Adv Exp Med Biol 2016;928:213–244.


7. Zhang H, Zheng W, Feng X, et al. Nrf2⁻ARE signaling acts as master pathway for the cellular antioxidant activity of fisetin.
Molecules 2019;24:708.



8. Park HH, Lee S, Oh JM, et al. Anti-inflammatory activity of fisetin in human mast cells (HMC-1).
Pharmacol Res 2007;55:31–37.


9. Sun X, Ma X, Li Q, et al. Anti‑cancer effects of fisetin on mammary carcinoma cells via regulation of the PI3K/Akt/mTOR pathway: in vitro and in vivo studies.
Int J Mol Med 2018;42:811–820.



10. Sahu BD, Kalvala AK, Koneru M, et al. Ameliorative effect of fisetin on cisplatin-induced nephrotoxicity in rats via modulation of NF-κB activation and antioxidant defence.
PLoS One 2014;9:e105070.



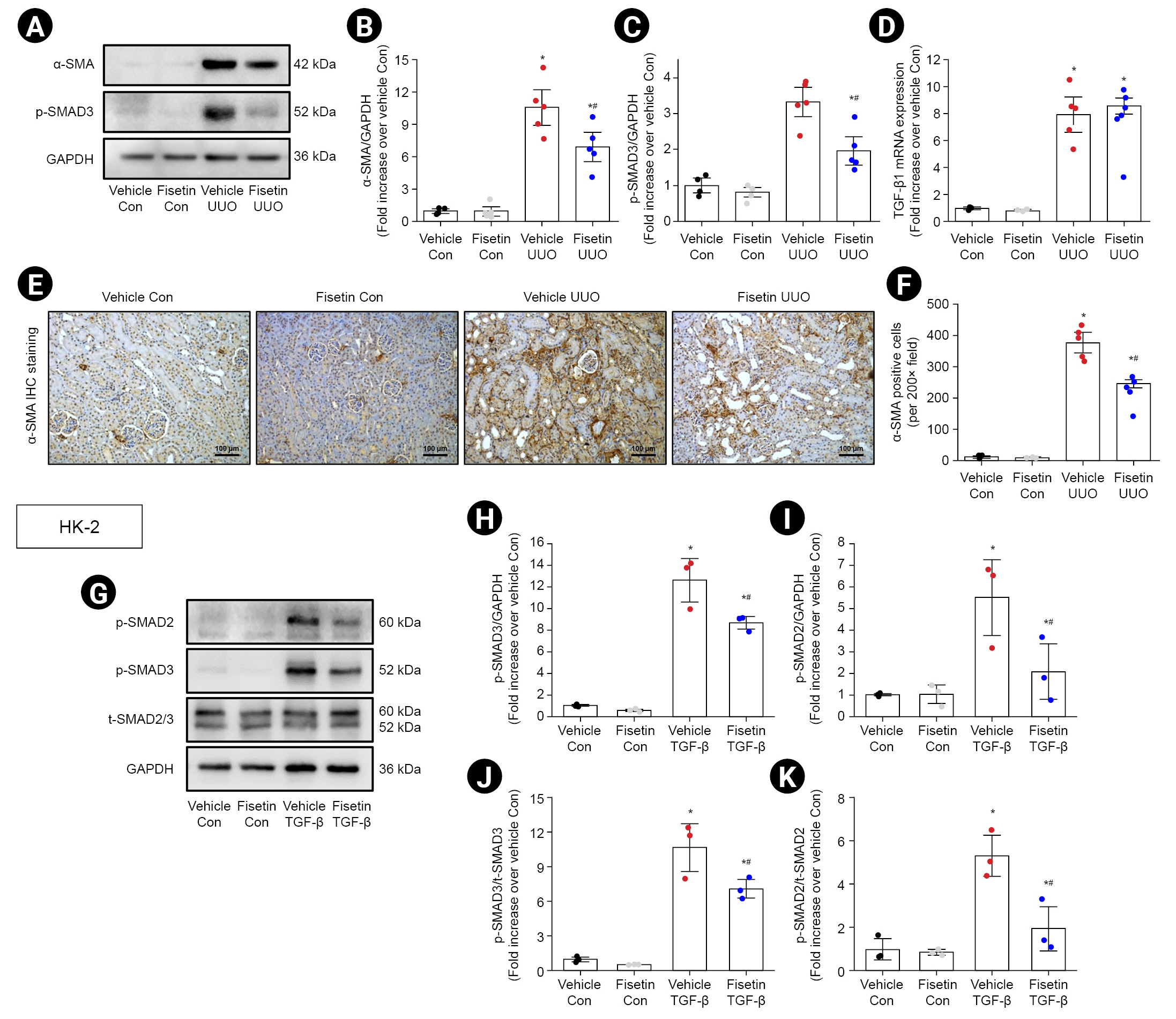
11. Ren Q, Tao S, Guo F, et al. Natural flavonol fisetin attenuated hyperuricemic nephropathy via inhibiting IL-6/JAK2/STAT3 and TGF-β/SMAD3 signaling.
Phytomedicine 2021;87:153552.


12. Han SJ, Noh MR, Jung JM, et al. Hydrogen sulfide-producing cystathionine γ-lyase is critical in the progression of kidney fibrosis.
Free Radic Biol Med 2017;112:423–432.


13. Li Z, Wang Y, Zhang Y, et al. Protective effects of fisetin on hepatic ischemia-reperfusion injury through alleviation of apoptosis and oxidative stress.
Arch Med Res 2021;52:163–173.


14. Ren Q, Guo F, Tao S, Huang R, Ma L, Fu P. Flavonoid fisetin alleviates kidney inflammation and apoptosis via inhibiting Src-mediated NF-κB p65 and MAPK signaling pathways in septic AKI mice.
Biomed Pharmacother 2020;122:109772.


15. Zhang L, Tong X, Huang J, et al. Fisetin alleviated bleomycin-induced pulmonary fibrosis partly by rescuing alveolar epithelial cells from senescence.
Front Pharmacol 2020;11:553690.



16. Meng XM, Tang PM, Li J, Lan HY. TGF-β/Smad signaling in renal fibrosis.
Front Physiol 2015;6:82.



18. Martínez-Klimova E, Aparicio-Trejo OE, Tapia E, Pedraza-Chaverri J. Unilateral ureteral obstruction as a model to investigate fibrosis-attenuating treatments.
Biomolecules 2019;9:141.



19. Heldin CH, Miyazono K, ten Dijke P. TGF-beta signalling from cell membrane to nucleus through SMAD proteins.
Nature 1997;390:465–471.



20. Walton KL, Johnson KE, Harrison CA. Targeting TGF-β mediated SMAD signaling for the prevention of fibrosis.
Front Pharmacol 2017;8:461.



21. Inazaki K, Kanamaru Y, Kojima Y, et al. Smad3 deficiency attenuates renal fibrosis, inflammation, and apoptosis after unilateral ureteral obstruction.
Kidney Int 2004;66:597–604.


22. Ai J, Nie J, He J, et al. GQ5 hinders renal fibrosis in obstructive nephropathy by selectively inhibiting TGF-β-induced Smad3 phosphorylation.
J Am Soc Nephrol 2015;26:1827–1838.


23. Chen H, Yang T, Wang MC, Chen DQ, Yang Y, Zhao YY. Novel RAS inhibitor 25-O-methylalisol F attenuates epithelial-to-mesenchymal transition and tubulo-interstitial fibrosis by selectively inhibiting TGF-β-mediated Smad3 phosphorylation.
Phytomedicine 2018;42:207–218.


24. Liu L, Gan S, Li B, Ge X, Yu H, Zhou H. Fisetin alleviates atrial inflammation, remodeling, and vulnerability to atrial fibrillation after myocardial infarction.
Int Heart J 2019;60:1398–1406.


25. Aranda-Rivera AK, Cruz-Gregorio A, Aparicio-Trejo OE, Ortega-Lozano AJ, Pedraza-Chaverri J. Redox signaling pathways in unilateral ureteral obstruction (UUO)-induced renal fibrosis.
Free Radic Biol Med 2021;172:65–81.


26. Mittal M, Siddiqui MR, Tran K, Reddy SP, Malik AB. Reactive oxygen species in inflammation and tissue injury.
Antioxid Redox Signal 2014;20:1126–1167.



27. Moriyama T, Kawada N, Nagatoya K, Horio M, Imai E, Hori M. Oxidative stress in tubulointerstitial injury: therapeutic potential of antioxidants towards interstitial fibrosis.
Nephrol Dial Transplant 2000;15 Suppl 6:47–49.


29. Milkovic L, Cipak Gasparovic A, Zarkovic N. Overview on major lipid peroxidation bioactive factor 4-hydroxynonenal as pluripotent growth-regulating factor.
Free Radic Res 2015;49:850–860.


30. Tamura M, Aizawa R, Hori M, Ozaki H. Progressive renal dysfunction and macrophage infiltration in interstitial fibrosis in an adenine-induced tubulointerstitial nephritis mouse model.
Histochem Cell Biol 2009;131:483–490.



31. Shen B, Liu X, Fan Y, Qiu J. Macrophages regulate renal fibrosis through modulating TGFβ superfamily signaling.
Inflammation 2014;37:2076–2084.



32. Fortini F, Vieceli Dalla Sega F, Marracino L, et al. Well-known and novel players in endothelial dysfunction: updates on a Notch(ed) landscape.
Biomedicines 2021;9:997.



33. Qin CC, Liu YN, Hu Y, Yang Y, Chen Z. Macrophage inflammatory protein-2 as mediator of inflammation in acute liver injury.
World J Gastroenterol 2017;23:3043–3052.



35. Ashcroft GS, Yang X, Glick AB, et al. Mice lacking Smad3 show accelerated wound healing and an impaired local inflammatory response.
Nat Cell Biol 1999;1:260–266.



36. Pan B, Liu G, Jiang Z, Zheng D. Regulation of renal fibrosis by macrophage polarization.
Cell Physiol Biochem 2015;35:1062–1069.



37. Tang WB, Ling GH, Sun L, Liu FY. Smad anchor for receptor activation (SARA) in TGF-beta signaling.
Front Biosci (Elite Ed) 2010;2:857–860.











 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















