Introduction
Chronic kidney disease (CKD) shows sex differences in prevalence and rate of progression. The incidence or prevalence of CKD is high among women in most countries [
1]; nevertheless, men have a higher risk of CKD progression and are more likely to develop end-stage kidney disease (ESKD) [
2]. As for kidney transplantation (KT), women are less likely to be kidney recipients but are more likely to become living kidney donors [
3,
4]. Various causes have been mentioned for this sex disparity in KT. Women are more likely to be excluded from being KT recipients due to a higher level of preexisting lymphocytotoxic antibodies. Men may also be excluded as donors because of preexisting comorbidities such as diabetes or coronary artery disease.
Recently, the Asian Society of Transplantation in partnership with Women in Transplantation highlighted the disparity between male and female KT donors and recipients in the Asia Pacific region [
5]. Overall, there was a female predominance of living donors across most countries; however, there were large differences in the female proportions of donors and recipients worldwide. Social factors such as attitude, financial considerations, patriarchy, and coercion have been suggested to be key contributors to disparity [
5]. Since the success of the first kidney transplant in 1969, Korea has made remarkable progress in terms of both quantity and quality of transplants, based on number and survival rate. Furthermore, the socioeconomic status of women in Korea is generally improving. According to the Organisation for Economic Cooperation and Development (OECD), Korean women took a larger role in economic activities and achieved great strides in educational attainment [
6]. However, there has not been much research on sex disparity in the field of CKD and transplantation in Korea. Thus, this study aimed to describe the perspectives of nephrologists on sex disparity in dialysis, waiting list registration, and KT.
Discussion
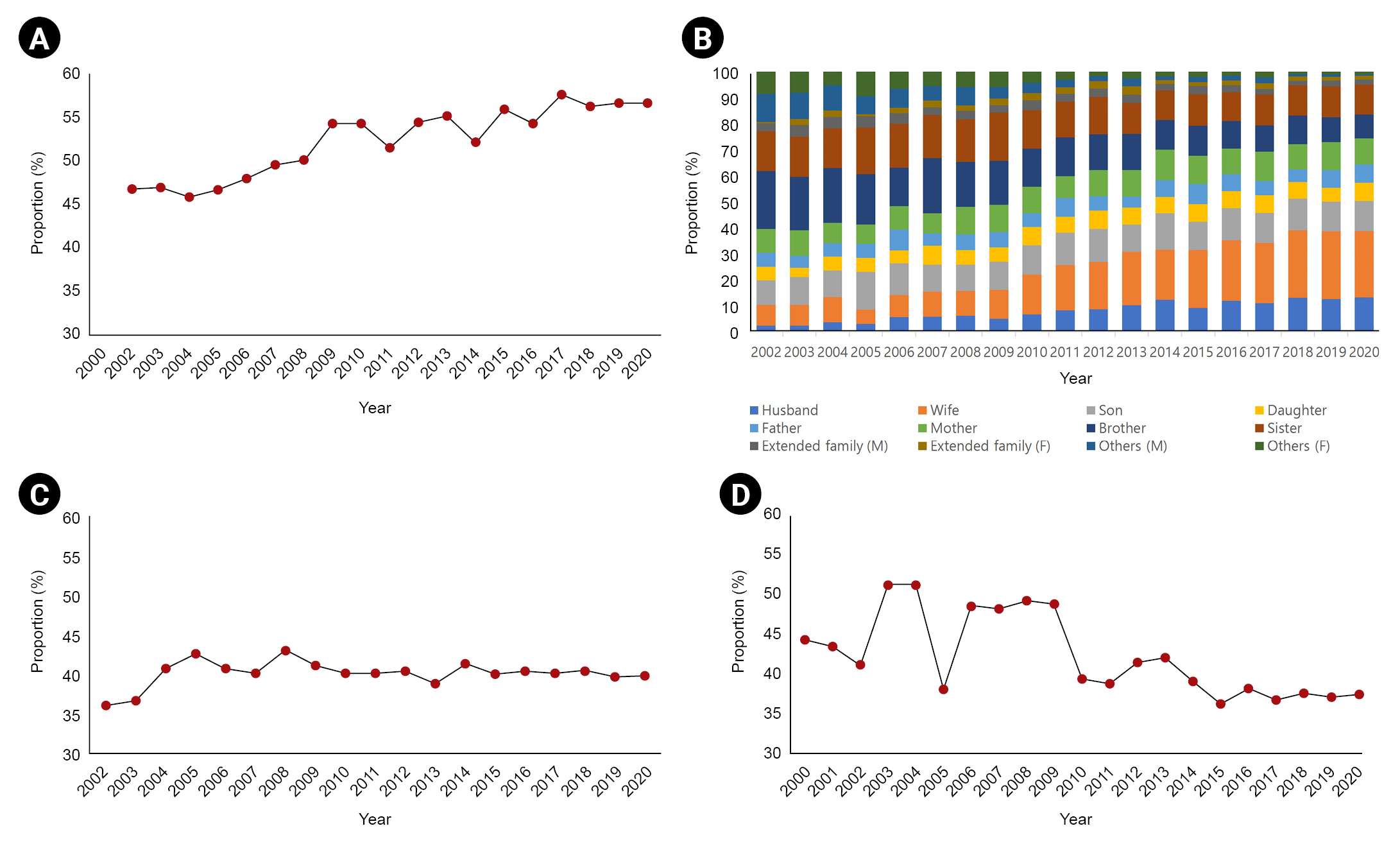
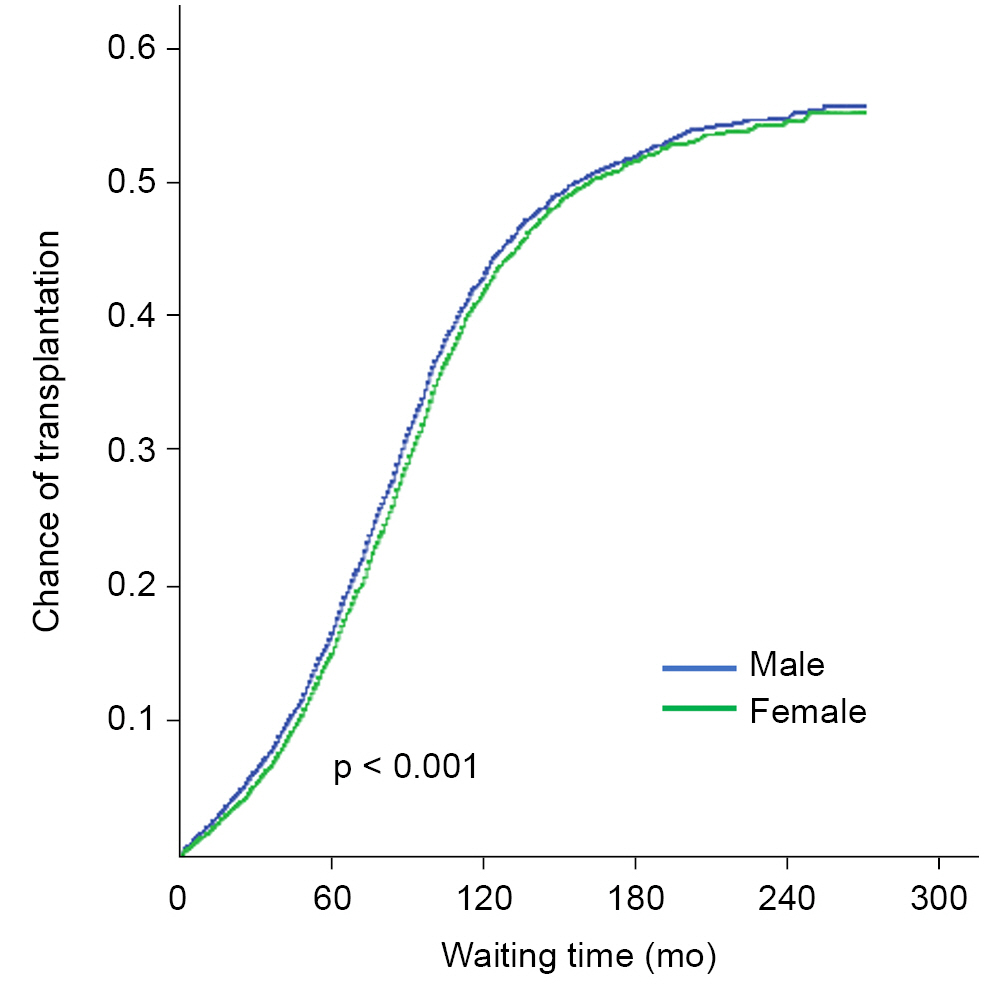
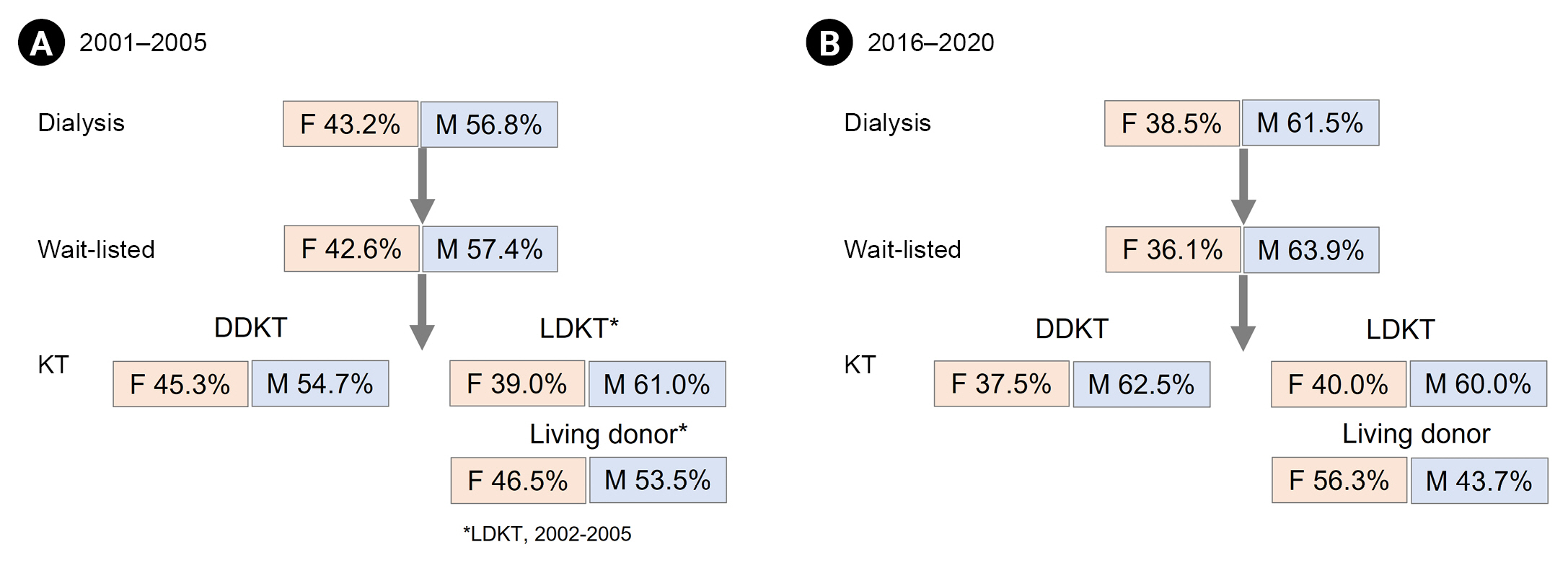
In this study, we described trends in the proportion of females on dialysis, on the waiting list, and who were KT donors and recipients over 20 years. We found a decreasing trend in the proportion of females in incident dialysis, on the waiting list, and who received DDKT sequentially. In contrast, the proportion of female living donors showed an increasing trend; in particular, there was a significant increase in the number of donations from wives.
In this study, we have not mentioned the female proportion of CKD in Korea. Because it is impossible to conduct a full investigation of the proportion of females with CKD, there is inevitably a sampling bias, and the prevalence of CKD among females and males differs from study to study [
7]. The proportion of males vs. females with CKD was 59% vs. 41% in the Korean National Health Insurance Service-National Sample Cohort from 2003 to 2007 [
8]. Likewise, CKD prevalence in men was 3.5% and in women was 2.4% in Korean National Health and Nutrition Examination Survey VI [
7]. In the case of dialysis, there are statistical data from the KSN registry project, which might not be accurate because of the self-reporting system of each dialysis center. Based on KSN registry data, the male proportion of new dialysis continued to increase over the past 20 years.
The ratio of men on the waiting list is also increasing. This could be because the ratio of men receiving dialysis has increased; furthermore, this may be because the proportion of women over 70 years of age is higher than that of men. Older dialysis patients might be reluctant to register for transplantation, which may explain why the waiting list registration rate for women is lower than for men. A similar trend was seen in the United States [
9]; national data from the United States showed that access to transplantation for women declined with increasing age and comorbidities.
Living donation from females is increasing steadily. Analysis of the donor-recipient relationship among family members showed marked increase in interspousal donation. Donations from husbands to wives and
vice versa are increasing; however, donation from wives is over twice that from husbands on average. The development of ABO-incompatible KT (ABOi KT) could have affected the increase in donations from wives. Since ABOi KT was introduced in Korea in 2007, ABOi KT has accounted for over 20% of all LDKT [
10]. Because ABOi KT from spousal donors can be considered for ESKD patients whose only potential donor is an ABO-mismatched spouse, ABOi KT increased spousal donation by up to 31.5% in LDKT in Korea [
11]. There were more donations from sons than daughters before; however, currently donations from sons are on the decline and those from daughters are increasing. Meanwhile, donations from sisters are higher than those from brothers.
To donate a kidney, one must be in good physical and mental health. Individuals with uncontrolled hypertension, diabetes, malignancy, or acute infections are excluded from donation. The unbalanced ratio between men and women could be attributed to the higher rate of comorbidities among men than among women. Another reason is the higher level of presensitization in women than in men. However, sex discrepancies appear to be multifactorial in nature, and vary depending on both sociocultural and biological determinants. The main reasons for sex disparities could be the higher incidence of kidney disease in men and fear of losing earnings among men [
12]. Sociocultural factors such as patriarchy and socioeconomic dependency of women on men within the family may be key contributors to increasing the number of female living donors in developing countries [
13]. In the case of Korea, nuclear families and fewer children could also be a factor. It can be hypothesized that in the early 2000s, more men acted as donors; however, recently, owing to reduced number of male donors in the family, females such as daughters and sisters have opted to become donors.
There are several limitations to this study. We obtained dialysis data from the KSN ESKD registry which is collected through an internet program and self-reported by the dialysis center. In 2020, 51.9% of dialysis centers in Korea participated in this registry [
14], which means not all dialysis patients were included in the study. In addition, socioeconomic factors or underlying diseases could not be considered in the analysis of sex disparities because these data were not available in the KONOS database. Also, sex disparities in the transition from CKD to end-stage renal disease (ESRD) or ESRD to the waiting list could not be analyzed owing to absence of a relevant national registry. However, this study is meaningful in that it shows patterns in sex disparities over 20 years.
We use the term ‘sex disparity’ rather than ‘sex inequity.’ Disparity implies a difference of some kind, whereas inequity implies unfairness and injustice. It is obvious that there is a disparity with regard to sex for women in transplantation; however, we could not establish whether there is sex inequity in transplantation because we could not consider socioeconomic factors in this analysis.
In summary, although there was a decreasing trend in the proportion of females on dialysis, on the waiting list, and receiving DDKT over the past 20 years, the proportion of females among LDKT donors is increasing. The underlying influencing factors, especially socioeconomic and biological factors in Korea, should be elucidated to ensure equal access to KT for both sexes.











 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















