Dialysis specialist care and patient survival in hemodialysis facilities: a Korean nationwide cohort study
Article information
Abstract
Background
It is important for the dialysis specialist to provide essential and safe care to hemodialysis (HD) patients. However, little is known about the actual effect of dialysis specialist care on the survival of HD patients. We therefore investigated the influence of dialysis specialist care on patient mortality in a nationwide Korean dialysis cohort.
Methods
We used an HD quality assessment and National Health Insurance Service claims data from October to December 2015. A total of 34,408 patients were divided into two groups according to the proportion of dialysis specialists in their HD unit, as follows: 0%, no dialysis specialist care group, and ≥50%, dialysis specialist care group. We analyzed the mortality risk of these groups using the Cox proportional hazards model after matching propensity scores.
Results
After propensity score matching, 18,344 patients were enrolled. The ratio of patients from the groups with and without dialysis specialist care was 86.7% to 13.3%. The dialysis specialist care group showed a shorter dialysis vintage, higher levels of hemoglobin, higher single-pool Kt/V values, lower levels of phosphorus, and lower systolic and diastolic blood pressures than the no dialysis specialist care group. After adjusting demographic and clinical parameters, the absence of dialysis specialist care was a significant independent risk factor for all-cause mortality (hazard ratio, 1.10; 95% confidence interval, 1.03–1.18; p = 0.004).
Conclusion
Dialysis specialist care is an important determinant of overall patient survival among HD patients. Appropriate care given by dialysis specialists may improve clinical outcomes of patients undergoing HD.
Introduction
The survival of hemodialysis (HD) patients has improved significantly over the past few decades with the development of dialysis-related technologies and drugs. However, the mortality rate remains high in patients with HD due to complications, such as cardiovascular disease and infections. Mortality in HD patients is influenced not only by patient factors but also by environmental factors and procedure-related factors (e.g., dialysis dosage, time of dialysis, and compliance with treatment regimen) [1,2]. In addition to patient- and facility-level characteristics, provider-level factors, such as physician caseload (patient-to-physician ratio), have been suggested to affect clinical outcomes [3,4]. Recent studies have similarly suggested that nephrologist caseload influences HD patient outcomes [5].
According to the Kidney Disease: Improving Global Outcomes (KDIGO) 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease in kidney disease, it is recommended that patients with a rapid decline in the glomerular filtration rate (GFR), a GFR of <30 mL/min/1.73 m2 (GFR category grade 4–5), progressive chronic kidney disease, or severe albuminuria or hematuria be referred to specialist kidney care services [6]. There have been many studies showing the effect of early nephrologist referral on patient mortality and clinical outcomes among those with predialysis chronic kidney disease. Earlier and more frequent consultations with a nephrologist improved patient survival within the first year of dialysis [7,8]. Timely referral to a nephrologist also reduced the initial 90-day mortality rate among elderly patients with end-stage renal disease [9]. Even remote distances from the nephrologist’s office affect the mortality rate and clinical outcomes before and after starting HD [10,11]. However, there have been few studies demonstrating the effect of nephrologist care on overall mortality among HD patients.
HD patients are a unique population with a high burden of complex comorbid conditions who are routinely subjected to specialized procedures. In this regard, there may be a differential association between nephrologist care and outcomes in this population. In many countries, including the United States and Germany, only nephrologists can prescribe HD order sheets and medicine for HD patients [12–14]. In Japan, on the other hand, the Japanese Society of Dialysis Therapy operates an independent certification system called the “dialysis specialist accreditation program,” in which physicians must receive training in both internal medicine and nephrology for ≥5 years at authorized renal units and pass an exam to become dialysis specialists [15]. In South Korea, since there are no workforce requirements for HD unit operation, physicians other than dialysis specialists or board-certified nephrologists treat HD patients from place to place. Since the care given by qualified physicians may play an important role in the management of HD patients [5,16,17], we evaluated whether dialysis specialist care may affect patient mortality among Korean patients on maintenance HD.
Methods
Ethics statement
The present study was performed according to the principles of the Declaration of Helsinki. The study protocol was reviewed and approved by the Institutional Review Board of Ewha Womans University Seoul Hospital in Seoul, Republic of Korea (No. SEUMC 2019-11-001), which waived the need for written informed consent because the study participants were deidentified.
Data source and study population
This study enrolled maintenance HD patients already on dialysis for end-stage renal disease. We used HD quality assessment data and Health Insurance Review and Assessment (HIRA) Service claims data collected from October to December 2015 to gather demographic and clinical data of individual HD patients. Adult HD patients aged ≥18 years who received HD treatment of ≥2 times weekly as outpatients were included in this assessment. Patients who were admitted during assessment or lost to follow-up were excluded from the analysis [12].
The HD quality assessment also collected data from each HD facility through a web-based data-collection system [18]. The collected data include 12 measures in three domains (structure, process, and monitoring) (Supplementary Table 1, available online). Structural information on medical staff members (doctors and nurses), number of HD treatments, numbers of HD equipment and emergency equipment, and status in the water quality test were collected. In addition, information in procedural domains (vascular access stenosis monitoring and frequency of regular laboratory tests) and monitoring domains (frequency and satisfaction rate of HD adequacy and satisfaction rates of calcium and phosphorus control) were collected. The data retrieved from the web-based database were compared with those obtained from patient electronic medical records to check the accuracy and reliability. Demographic data, including age, sex, dialysis vintage, and comorbidities, were also collected. Body mass index and systolic and diastolic blood pressures before the HD session were also measured and reported. Laboratory assessments consisted of plasma hemoglobin, serum albumin, serum calcium and phosphorus, iron saturation, and serum ferritin.
The comorbidities of study participants were identified using the International Classification of Diseases-10 codes from the National Health Insurance Service claims database and searched from January to December 2015 [19,20]. Comorbidities included diabetes mellitus, hypertension, congestive heart failure, cerebrovascular disease, ischemic heart disease, and atrial fibrillation (Supplementary Table 2, available online).
In South Korea, there are two qualifications related to nephrology practice, which are nephrologist board-certification by the Korean Association of Internal Medicine and dialysis specialist certification by the Korean Society of Nephrology. Currently, there are 1,103 board-certified nephrologists and 1,407 certified dialysis specialists in South Korea (these groups overlap somewhat). To become a dialysis specialist, a doctor must complete 3 years of training in internal medicine plus 1 year of training in an authorized HD unit at a university hospital accredited by the Korean Society of Nephrology.
Definition of study groups and outcomes
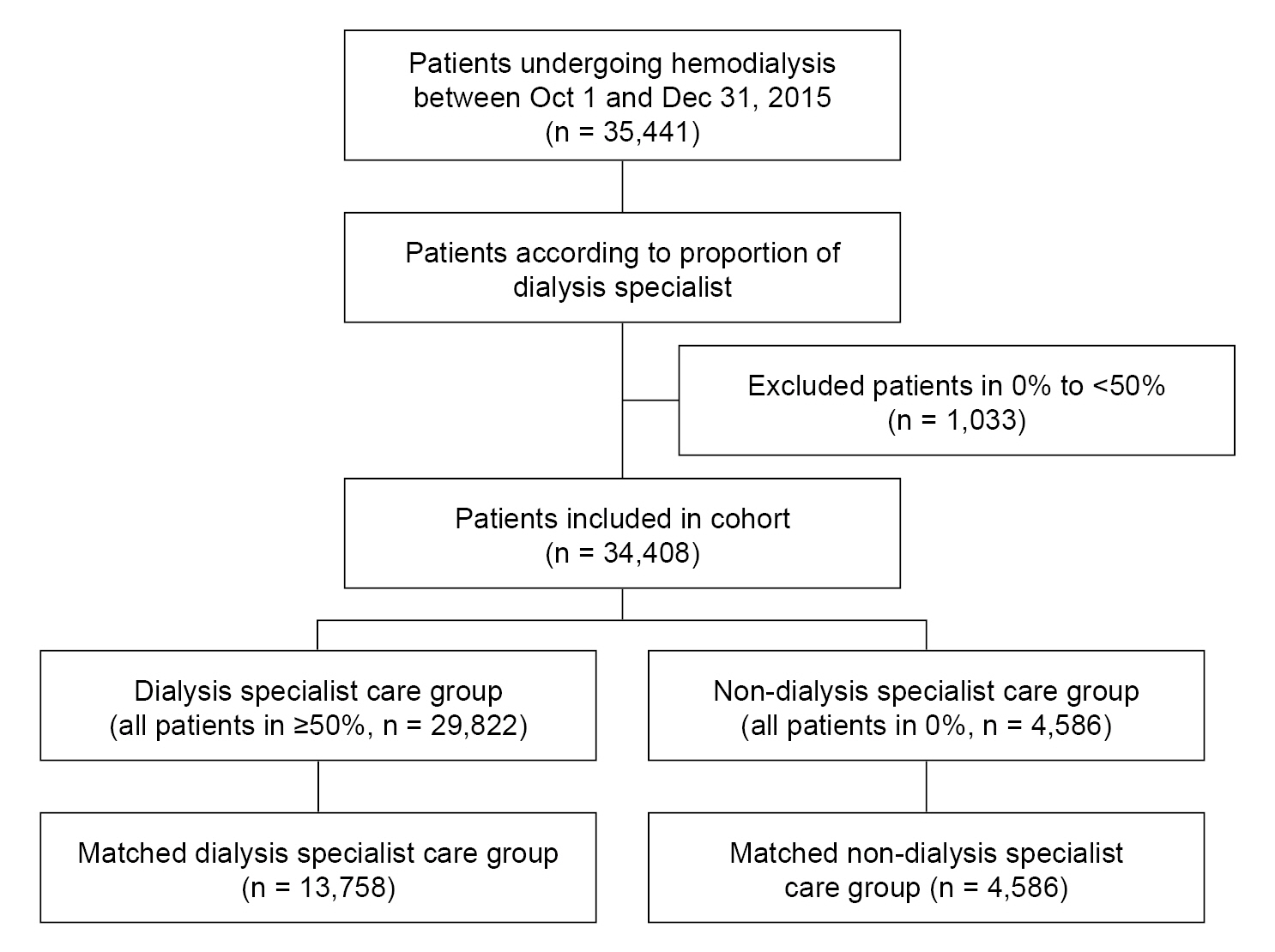
The proportion of dialysis specialists was defined as the percentage of dialysis specialists among all doctors employed in each HD unit. This study included 35,441 patients treated at 799 facilities (Fig. 1). Among them, 30,855 patients (87.1%) were treated by >1 dialysis specialist and 4,586 patients (12.9%) were not treated by any dialysis specialist. Among the HD units with >1 dialysis specialist, there were 20 HD units with dialysis specialist proportions of <50%, and only 1,033 patients (2.9%) received HD in these units. Therefore, for the analysis of patient outcomes according to the proportion of dialysis specialists, we defined two study groups according to the proportion of dialysis specialists, including a no dialysis specialist care group (0%) and a dialysis specialist care group (≥50%).
The primary outcome was all-cause mortality. Mortality data were collected between January 2016 and June 2019. Patients who received a kidney transplant during the follow-up period were censored at the time of their kidney transplantation.
Statistical analyses
Baseline characteristics and outcomes were compared between groups. The groups were matched in a 1:3 ratio using propensity scores to minimize confounding factors that can affect the outcomes. The propensity score matching was performed based on age, sex, and the presence of diabetes mellitus before analysis using the “MatchIt” package of R version 4.0.2. (R Foundation for Statistical Computing). Normally distributed numerical variables were expressed using mean and standard deviation values, while the variables with skewed distributions were expressed with median and interquartile range values. Statistical comparisons between continuous variables were performed using an independent t test. For the data without normal distribution, the Wilcoxon signed-rank test for two groups was performed. The chi-square test and the Fisher exact test were applied to categorical variables, as appropriate.
The Kaplan-Meier method was used to compare death-free survival curves, and differences were assessed using the log-rank test. We used univariate and multivariate Cox proportional hazards models to estimate the risk factors associated with patient mortality. We tested the Schoenfeld residual using the “cox.zph” function of the R package and performed proportional hazards regression modeling by satisfying the proportional hazard ratio (HR) assumption. Model 1 was adjusted for age and sex. Model 2 was adjusted for medical comorbidities in addition to the factors included in model 1. Model 3 was adjusted for all the demographic and clinical parameters. Finally, subgroup analyses were performed to define the relative risk of mortality according to the absence of dialysis specialist care among predefined subgroups (age, <65 years vs. ≥65 years; sex, female vs. male; HD vintage, <5 years vs. ≥5 years; presence vs. absence of diabetes mellitus, ischemic heart disease, congestive heart failure, and cerebrovascular disease; plasma hemoglobin, ≥10 g/dL vs. <10 g/dL; serum albumin, ≥3.5 g/dL vs. <3.5 g/dL; and serum phosphorus, <5.0 mg/dL vs. ≥5.0 mg/dL). All statistical analyses were performed using R version 4.0.2. A p-value of <0.05 was considered statistically significant.
Results
Baseline characteristics according to dialysis specialist care grouping
Among 35,441 patients undergoing total HD in 2015, 1,033 patients with a dialysis specialist proportion of 0% to 50% of the dialysis unit were excluded (Fig. 1). Finally, a total of 34,408 HD patients from 779 HD centers were included in the analysis. The mean age was 60.0 ± 12.9 years, and 58.8% were male. Hypertension (81.4%) and diabetes mellitus (58.4%) were the two most common comorbidities. The ratio of the groups with and without dialysis specialist care was 86.7% (29,822 patients) to 13.3% (4,586 patients). Baseline characteristics according to dialysis specialist care group enrollment are presented in Table 1.
After propensity score matching, the number of patients in the dialysis specialist care group was 13,758 patients (86.7%) and the number of patients in the no dialysis specialist care group was 4,586 patients (13.3%) (Fig. 1), respectively. The patients in the dialysis specialist care group showed a shorter dialysis vintage and a lower proportion of comorbidities other than congestive heart failure compared to the no dialysis specialist care group (Table 1). The dialysis specialist care group also demonstrated higher levels of plasma hemoglobin (10.72 ± 0.83 g/dL vs. 10.61 ± 0.88 g/dL, p < 0.001), and single-pool Kt/V (1.56 ± 0.27 vs. 1.52 ± 0.28, p < 0.001). However, the dialysis specialist care group showed lower systolic (141.03 ± 15.32 mmHg vs. 143.05 ± 15.76 mmHg, p < 0.001) and diastolic (76.75 ± 9.59 mmH vs. 79.69 ± 8.99 mmHg, p < 0.001) blood pressures and lower levels of serum calcium (8.95 ± 0.82 mg/dL vs. 9.08 ± 0.78 mg/dL, p < 0.001) and phosphorus (4.88 ± 1.31 mg/dL vs. 5.04 ± 1.39 mg/dL, p < 0.001) compared to the no dialysis specialist care group.
All-cause mortality according to dialysis specialist care grouping
A total of 7,445 deaths (21.6%) occurred during 36.2 ± 11.2 months. After censoring 2,006 cases (5.8%) who received kidney transplantation, the crude death rate was 71.7 per 1,000 person-years. After propensity score matching, a total of 4,314 patients died, and the crude death rate was 78.3 per 1,000 person-years. The dialysis specialist care group exhibited a lower risk of death than the no dialysis specialist care group, showing a crude death rate ratio of 1.132 (Table 2). In the survival analysis, the mortality rate was also lower in the dialysis specialist care group (log-rank test p < 0.001) (Fig. 2) both before and after propensity score matching.

Kaplan-Meier analysis for survival (A) before PSM and (B) after PSM.
The mortality rate was low in the dialysis specialist care group before and after PSM.
PSM, propensity score matching.
In the univariate analysis for all-cause mortality, the no dialysis specialist care group was associated with a higher mortality risk (HR, 1.13; 95% confidence interval [CI], 1.16–1.21; p < 0.001). When we adjusted for age and sex (model 1), no dialysis specialist care group enrollment remained an independent risk factor for patient mortality (HR, 1.13; 95% CI, 1.16–1.21; p < 0.001). Similarly, in model 2 and model 3, no dialysis specialist care group enrollment remained an independent risk factor for all-cause mortality (HR, 1.12; 95% CI, 1.05–1.20; p < 0.001 in model 2 and HR, 1.10; 95% CI, 1.03–1.18; p = 0.004 in model 3) (Table 3).
Subgroup analysis for all-cause mortality in the no dialysis specialist care group
We performed a subgroup analysis to define the population at high risk for all-cause death in the absence of dialysis specialist care. The no dialysis specialist care group showed higher mortality among patients without ischemic heart disease (HR, 1.18; 95% CI, 1.08–1.28; p < 0.001), congestive heart failure (HR, 1.15; 95% CI, 1.07–1.24; p < 0.001), or cerebrovascular disease (HR, 1.17; 95% CI, 1.08–1.26; p < 0.001) (Fig. 3). In addition, enrollment in this group was an independent risk factor for increased mortality in patients without anemia (HR, 1.15; 95% CI, 1.07–1.24; p < 0.001), hypoalbuminemia (HR, 1.17; 95% CI, 1.09–1.26; p < 0.001), or hypophosphatemia (HR, 1.18; 95% CI, 1.08–1.28; p < 0.001). However, there was no difference according to age, sex, or diabetes subgroup.

Subgroup analysis after propensity score matching.
Dialysis specialist care was associated with a reduction in mortality in patients regardless of age, sex, or the presence of diabetes. However, dialysis specialist care was associated with reduced mortality among patients with a short dialysis vintage; those without ischemic heart disease, congestive heart failure, or cerebrovascular disease; and those without anemia, hypoalbuminemia, or hypophosphatemia.
CI, confidence interval; HR, hazard ratio.
Discussion
In this article, we evaluated the effect of dialysis specialist care on patient mortality using nationwide HD quality assessment data from South Korea. The absence of dialysis specialists in HD facilities was an independent risk factor for all-cause mortality even after adjusting for demographic and clinical parameters. Moreover, patients in the dialysis specialist care group showed higher plasma hemoglobin concentrations, lower blood pressures, and lower serum phosphorus levels than those in the no dialysis specialist care group.
In the United States, there are several types of personnel in HD facilities, such as a medical director, charge nurses and registered nurses, patient care technicians, water treatment system technicians, dietitians, and social workers [21]. Since there are various HD-specific complications and technical problems, the special care given by nephrologists or dialysis specialists may be essential to improve patient outcomes [22]. However, a shortage of both nephrologists and patient care technicians in the American workforce has persisted, which may constitute a barrier to optimal dialysis care [23]. A recent article speculated that the higher mortality among HD patients in America compared to other countries may be due to looser requirements for mandated physicians in HD facilities [24]. On the other hand, Japan has strict rules about medical staffing in HD facilities, with either nephrologists or dialysis specialists required. A previous article by Furumatsu et al. [15] demonstrated that prefectures with higher quintiles of dialysis specialists showed better long-term survival rates among HD patients. However, this result has not been confirmed at either the individual or facility level.
To our knowledge, our study is the first to demonstrate the importance of specialized care by nephrologists in HD units for improving the overall patient mortality rate in South Korea. In a previous study by Slinin et al. [3], 6.9% of HD patients did not receive specialized care from a doctor with a specialty in nephrology. In contrast to the previous study, the number of patients who did not receive specialized care was 12.9% in our study, which was a larger proportion than that from the previous paper. Therefore, the difference in the distribution of patients likely had a significant impact on the prognosis of HD patients in this study. In addition, our results showed that patients treated in HD units with dialysis specialist care demonstrated fewer HD-related complications like anemia, uncontrolled blood pressure, and mineral bone disorders. A previous study also mentioned that more frequent patient–nephrologist contact resulted in the greater achievement of clinical targets for albumin, calcium-phosphate product, dialysis dose, and hemoglobin [25]. Dialysis specialists are the key professionals in the delivery of dialysis therapy and therefore may manage HD-related complications better than non-nephrologists. On the other hand, subgroup analyses demonstrated that dialysis specialist care was more effective among HD patients without cardiovascular morbidities or other complications. This may be due to the high mortality rates among groups with comorbidities and complications that dialysis specialist care may not be able to overcome to improve patient survival.
The strengths of our study include its large sample size, relatively long duration of follow-up, and analysis of well-balanced groups with propensity score matching. However, this study also has several limitations. First, we did not analyze cause-specific mortality among HD patients according to dialysis specialist care since the nationwide database does not include details on the cause of morbidity, such as cardiovascular disease, infection, vascular access problems, or malnutrition. Second, hospitalized patients at the time of HD quality assessment were excluded from this study. Third, we did not include patients in HD units with a proportion of dialysis specialists between 0% and 50%. Although the number of patients in HD units within this bracket is low (1,033 patients [2.9%] in 20 HD units), there could be a graded risk of patient mortality according to the proportion of dialysis specialists. Fourth, we did not include information about vascular access or insurance type among HD patients in this study, and there were also no data on prescription patterns or HD modalities in HD quality assessment. Fifth, an analysis of the other components of HD quality assessment according to the proportion of dialysis specialists could not be performed. Further studies are needed to reveal the mechanisms by which dialysis specialist care influences outcomes and to determine the appropriate proportion of dialysis specialists to improve the quality of care and patient prognosis.
In conclusion, we found that mortality was lower among patients with dialysis specialist care than those without dialysis specialist care. This suggests a link between dialysis specialist care and patient outcomes in HD facilities. Thus, the presence of dialysis specialists at HD facilities may improve outcomes in patients undergoing HD.
Supplementary Materials
Supplementary data are available at Kidney Research and Clinical Practice online (https://doi.org/10.23876/j.krcp.22.103).
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.
Funding
This research was supported by the Hallym University Research Fund, 2022 (HURF-2022-24).
Data sharing statement
The data that support the findings of this study are available from HIRA, but restrictions apply to the availability of these data, so they are not publicly available. Data are, however, available from the authors upon request and with permission from HIRA.
Authors’ contributions
Conceptualization: DHK, YKL
Investigation: YEK, DRR, KHY, JHS, EJS
Data curation: DHK, HCP, AC, YKL
Formal analysis: DHK, JK
Funding acquisition: HCP
Writing–original draft: DHK, HCP
Writing–review & editing: YKL
All authors read and approved the final manuscript.
Acknowledgements
The authors participated in the Joint Project on Quality Assessment Research, and HIRA collected and provided the claims data and quality assessment data to the authors. We really appreciate having the opportunity to participate in the Joint Project on Quality Assessment Research in 2020.