1. Ruiz-Ortega M, Rup├®rez M, Esteban V, et al. Angiotensin II: a key factor in the inflammatory and fibrotic response in kidney diseases.
Nephrol Dial Transplant 2006;21:16ŌĆō20.


3. Forrester SJ, Booz GW, Sigmund CD, et al. Angiotensin II signal transduction: an update on mechanisms of physiology and pathophysiology.
Physiol Rev 2018;98:1627ŌĆō1738.



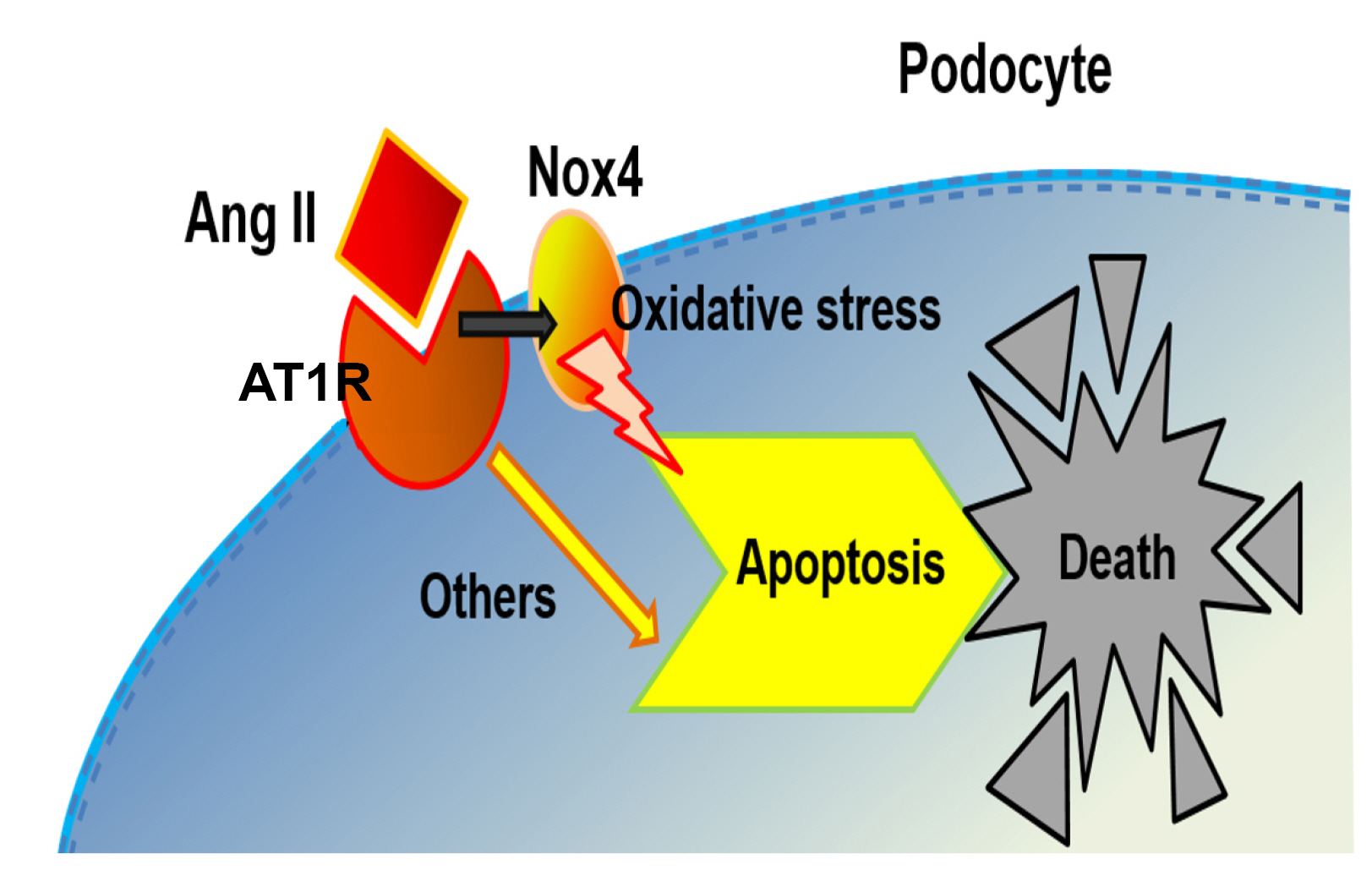
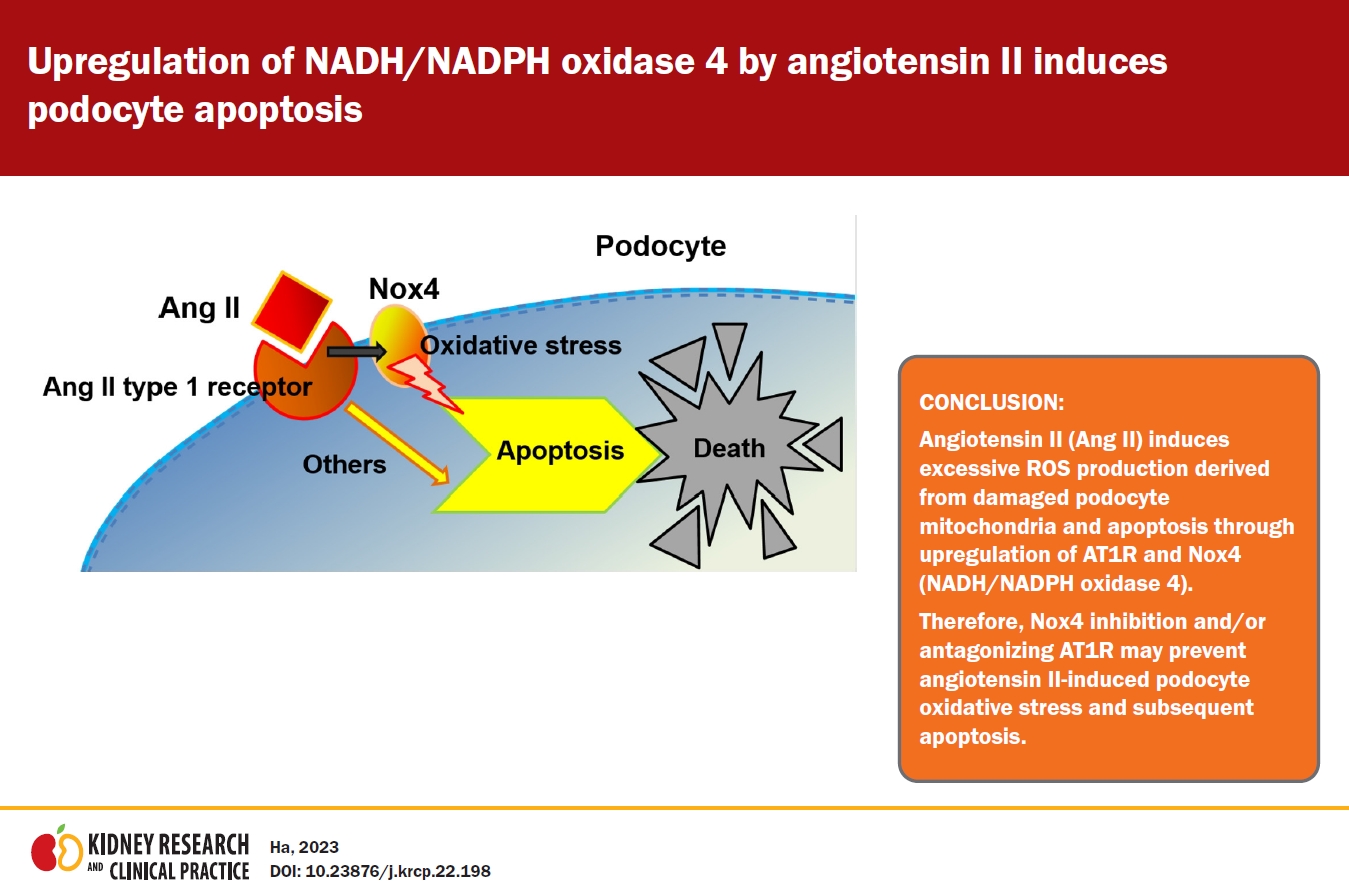
4. Ding G, Reddy K, Kapasi AA, et al. Angiotensin II induces apoptosis in rat glomerular epithelial cells.
Am J Physiol Renal Physiol 2002;283:F173ŌĆōF180.


5. Park HY, Seong SB, Min SY, Ha TS. CD2-associated protein/phosphoinositide 3-kinase signaling has a preventive role in angiotensin II-induced podocyte apoptosis.
Int J Biochem Cell Biol 2016;79:370ŌĆō381.


6. Griendling KK, Minieri CA, Ollerenshaw JD, Alexander RW. Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells.
Circ Res 1994;74:1141ŌĆō1148.


7. Rajagopalan S, Kurz S, M├╝nzel T, et al. Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation: contribution to alterations of vasomotor tone.
J Clin Invest 1996;97:1916ŌĆō1923.



8. Jones SA, OŌĆÖDonnell VB, Wood JD, Broughton JP, Hughes EJ, Jones OT. Expression of phagocyte NADPH oxidase components in human endothelial cells.
Am J Physiol 1996;271:H1626ŌĆōH1634.


9. Radeke HH, Cross AR, Hancock JT, et al. Functional expression of NADPH oxidase components (alpha- and beta-subunits of cytochrome b558 and 45-kDa flavoprotein) by intrinsic human glomerular mesangial cells.
J Biol Chem 1991;266:21025ŌĆō21029.


10. Greiber S, M├╝nzel T, K├żstner S, M├╝ller B, Schollmeyer P, Pavenst├żdt H. NAD(P)H oxidase activity in cultured human podocytes: effects of adenosine triphosphate.
Kidney Int 1998;53:654ŌĆō663.


11. Che G, Gao H, Hu Q, Xie H, Zhang Y. Angiotensin II promotes podocyte injury by activating Arf6-Erk1/2-Nox4 signaling pathway.
PLoS One 2020;15:e0229747.



12. Cui XL, Douglas JG. Arachidonic acid activates c-jun N-terminal kinase through NADPH oxidase in rabbit proximal tubular epithelial cells.
Proc Natl Acad Sci U S A 1997;94:3771ŌĆō3776.



13. Sedeek M, Callera G, Montezano A, et al. Critical role of Nox4-based NADPH oxidase in glucose-induced oxidative stress in the kidney: implications in type 2 diabetic nephropathy.
Am J Physiol Renal Physiol 2010;299:F1348ŌĆōF1358.


14. Circu ML, Aw TY. Reactive oxygen species, cellular redox systems, and apoptosis.
Free Radic Biol Med 2010;48:749ŌĆō762.



15. Ha TS. Roles of adaptor proteins in podocyte biology.
World J Nephrol 2013;2:1ŌĆō10.



16. Scott RP, Quaggin SE. Review series: the cell biology of renal filtration.
J Cell Biol 2015;209:199ŌĆō210.


17. Nath KA, Fischereder M, Hostetter TH. The role of oxidants in progressive renal injury.
Kidney Int Suppl 1994;45:S111ŌĆōS115.

18. Johnson RJ, Lovett D, Lehrer RI, Couser WG, Klebanoff SJ. Role of oxidants and proteases in glomerular injury.
Kidney Int 1994;45:352ŌĆō359.


19. Mundel P, Reiser J, Z├║├▒iga Mej├Ła Borja A, et al. Rearrangements of the cytoskeleton and cell contacts induce process formation during differentiation of conditionally immortalized mouse podocyte cell lines.
Exp Cell Res 1997;236:248ŌĆō258.


20. Forman HJ, Williams JJ, Nelson J, Daniele RP, Fisher AB. Hyperoxia inhibits stimulated superoxide release by rat alveolar macrophages.
J Appl Physiol Respir Environ Exerc Physiol 1982;53:685ŌĆō689.


21. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent.
J Biol Chem 1951;193:265ŌĆō275.


25. Wennmann DO, Hsu HH, Pavenst├żdt H. The renin-angiotensin-aldosterone system in podocytes.
Semin Nephrol 2012;32:377ŌĆō384.


27. Gill PS, Wilcox CS. NADPH oxidases in the kidney.
Antioxid Redox Signal 2006;8:1597ŌĆō1607.


28. Anderson M, Roshanravan H, Khine J, Dryer SE. Angiotensin II activation of TRPC6 channels in rat podocytes requires generation of reactive oxygen species.
J Cell Physiol 2014;229:434ŌĆō442.


29. Halliwell B, Gutteridge JM. Role of free radicals and catalytic metal ions in human disease: an overview. Methods Enzymol 1990;186:1ŌĆō85.
30. Gao N, Wang H, Zhang X, Yang Z. The inhibitory effect of angiotensin II on BKCa channels in podocytes via oxidative stress.
Mol Cell Biochem 2015;398:217ŌĆō222.



31. Rajaram RD, Dissard R, Jaquet V, de Seigneux S. Potential benefits and harms of NADPH oxidase type 4 in the kidneys and cardiovascular system.
Nephrol Dial Transplant 2019;34:567ŌĆō576.


32. Sedeek M, Nasrallah R, Touyz RM, H├®bert RL. NADPH oxidases, reactive oxygen species, and the kidney: friend and foe.
J Am Soc Nephrol 2013;24:1512ŌĆō1518.


33. Yuzefovych LV, LeDoux SP, Wilson GL, Rachek LI. Mitochondrial DNA damage via augmented oxidative stress regulates endoplasmic reticulum stress and autophagy: crosstalk, links and signaling.
PLoS One 2013;8:e83349.



34. Yuan Y, Xu X, Zhao C, et al. The roles of oxidative stress, endoplasmic reticulum stress, and autophagy in aldosterone/mineralocorticoid receptor-induced podocyte injury.
Lab Invest 2015;95:1374ŌĆō1386.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















