PKD2 mutation in an Iranian autosomal dominant polycystic kidney disease family with misleading linkage analysis data☆
Article information
Abstract
Background
Autosomal dominant polycystic kidney disease (ADPKD) is the most common genetic renal disorder caused by mutation in 2 genes PKD1 and PKD2. Thus far, no mutation is identified in approximately 10% of ADPKD families, which can suggest further locus heterogeneity. Owing to the complexity of direct mutation detection, linkage analysis can initially identify the responsible gene in appropriate affected families. Here, we evaluated an Iranian ADPKD family apparently unlinked to both PKD1 and PKD2 genes. This is one of the pioneer studies in genetic analysis of ADPKD in Iranian population.
Methods
Linkage reanalysis was performed by regenotyping of flanking microsatellite markers in 8 individuals of the ADPKD family. Direct mutation analysis was performed by Sanger sequencing.
Results
Mutation analysis revealed a pathogenic mutation (c.1094+1G>A) in the PKD2 gene in the proband. Analyzing 2 healthy and 4 clinically affected members confirmed the correct segregation of the mutation within the family and also ruled out the disease in 1 suspected individual. Misinterpretation of the linkage data was due to the occurrence of 1 crossing over between the PKD2 intragenic and the nearest downstream marker (D4S2929). Homozygosity of upstream markers caused the recombination indistinguishable.
Conclusion
Although analysis of additive informative polymorphic markers can overcome the misleading haplotype data, it is limited because of the lack of other highly polymorphic microsatellite markers closer to the gene. Direct mutation screening can identify the causative mutation in the apparently unlinked pedigree; moreover, it is the only approach to achieve the confirmed diagnosis in individuals with equivocal imaging results.
Introduction
Autosomal dominant polycystic kidney disease (ADPKD [OMIM# 173900]) is the most common genetic renal disorder, affecting approximately 1 in 400 to 1,000, in different populations [1], [2]. It is characterized by renal and extrarenal manifestations including bilateral renal cysts; hypertension; cysts in the liver, seminal vesicles, pancreas, and arachnoid membrane; intracranial aneurysms; dilatation of the aortic root; and mitral valve prolapse.
ADPKD is a genetically heterogeneous disorder with 2 known causative genes, PKD1 (MIM# 601313) on chromosome 16p13.3 [3] and PKD2 (MIM# 173910) on chromosome 4q21-23 [4], both discovered through linkage analysis. However, some reported families unlinked to either of these genes, suggesting the existence of a third locus [5], [6], [7], [8]; likewise, no mutation is identified in approximately 10% of ADPKD families [9]. More investigations revealed cosegregation of both PKD1 and PKD2 mutations in 1 previously unlinked family [10]. Besides, a recent comprehensive study identified pathogenic mutations in 4 of 5 such families [11]. Although these findings reduce the possibility of the third PKD3 locus, they highlight the importance of considering the linkage and haplotype segregation analysis confounders.
Linkage or haplotype analysis has been used widely in a variety of molecular genetics investigations, including genetic diagnosis, population genetics, forensics, complex kinship analysis, and also transplantation medicine [12], [13], [14]. Furthermore, it is an efficient approach to determine the pattern of inheritance among generations using highly polymorphic markers, mainly in the case of heterogeneous and multigenic disorders.
Although the new emerging next-generation sequencing method is the best and comprehensive method, it may not be available or cost benefit for research all over the world.
DNA testing is the definite ADPKD diagnostic method, especially in patients with equivocal imaging findings, or very early-onset cases, as well as potential related kidney donors from affected families. Also it helps at-risk couples to prevent disease transmission using preimplantation genetic diagnosis (PGD). In regard to emerging new therapeutic drugs, genetic testing might help to predict the best time and person to receive the intervention [15].
This study is one of the pioneer studies in genetic analysis of ADPKD in Iranian population, which investigates 1 Iranian ADPKD family with excluded linkage to both PKD1 and PKD2 loci. Furthermore, here we illustrated important sources of error in linkage analysis, a basic method used in clinical laboratories.
Methods
Subjects and DNA extraction
All individuals of 1 ADPKD family (P-13), who showed no linkage to both PKD1 and PKD2 loci in our previous study, were recruited. New blood samples were collected from all available individuals, including 5 patients, 2 healthy individuals, and 1 suspected patient with equivocal clinical diagnosis.
DNA was extracted using Exgene Blood SV mini kit (GeneAll Biotechnology Co, Ltd, Seoul, Korea) according to the manufacturer's instruction. The quality and quantity of DNA were assessed by the NanoDrop spectrophotometer (ND-1000, Thermo Scientific, USA) as well as agarose gel electrophoresis. The study was approved by the research ethics committee of the Tehran University of Medical Sciences. Informed consent was obtained from all the participants.
Analysis of microsatellite markers
Identification of the haplotypes of all individuals was performed manually based on the genotypes of 10 polymorphic microsatellite markers within or around the PKD1 and PKD2 genes. Characteristics of microsatellite markers and amplification details were described previously [16]. Furthermore, an in-house panel of 24 short tandem repeat markers was used to investigate the paternity within the family.
PCR amplification and sequencing
At the first step, coding sequences and exon–intron boundaries of PKD2 were screened by direct Sanger sequencing. New primers were designed to amplify the PKD2 fragments with the average size of 600 bp (Table 1). All PKD2 exons, except exon 1, were amplified in a final reaction volume of 25 μL using polymerase chain reaction (PCR) Master Mix (Ampliqon, Denmark, A140303) and 0.3 μmol/L of each primer, along with 30 ng of DNA. The final concentration of MgCl2 was 1.5 mmol/L. The cycling parameters were as follows: initial denaturation of 95°C for 5 minutes, followed by 30 cycles of 95°C for 30 seconds, 61°C for 30 seconds, 72°C for 40 seconds, and a final extension of 72°C for 5 minutes. Owing to the higher GC content, amplification of exon 1 was performed by the addition of 1X Q-solution (Qiagen group, www.qiagen.com) to the 25 μL reaction mixture as above, with denaturation at 98°C for 5 minutes, followed by 40 cycles of 96°C for 30 seconds, 64°C for 30 seconds, 72°C for 40 seconds, and a final extension of 72°C for 5 minutes.
PCR products were purified using the Expin kit (GeneAll Biotechnology Co, Ltd) to improve the quality of sequencing. Sanger sequencing was carried out using the ABI 3137 automated sequencer from Applied Biosystems (provided by the Pishgam Biotech Company, Tehran, Iran, www.pishgambc.com).
Variant analysis
The quality of sequencing was checked through assessing the obtained chromatogram by Sequence Scanner software, version 1.0 (http://www.appliedbiosystems.com). The data were then analyzed by Mutation Surveyor software, version 3.03 (www.softgenetics.com/mutationSurveyor.html), for variation calling purposes. Pathogenesis potentiality of unclassified variants was investigated by Sift, Provean [17], and PolyPhen-2 [18] software. Segregation analysis was performed by sequencing all the family members for the responsible mutation.
Results
Table 2 illustrates the polymorphic characteristics of each marker. Mean heterozygosity of all markers was higher than 0.5. Pedigree structure of family P-13 is shown in Fig. 1. The proband (IV-1) was first diagnosed with ADPKD at the age of 34 years by regular ultrasound examination because of positive family history. Haplotypes were constructed for all individuals of the family based on repeated microsatellite genotyping results. As illustrated in Fig. 1, the linkage analysis of the PKD1 locus identified that patients did not inherit the same haplotype. In the case of PKD2 locus, all affected individuals share a common haplotype, except IV-2 (diagnosed at age 22 by regular ultrasound examination) and III-3. The ultrasound results and clinical investigations of the III-3 individual was confusing and did not support ADPKD exactly; she was supposed to be affected because of her positive family history, so she was excluded in the linkage analysis. Her ultrasound scan revealed 1 small cyst in her right kidney that measured about 26 mm in the axial plane along with a small calcified region. Although noninformativeness of microsatellite markers made haplotype analysis difficult, according to linkage analysis data, this pedigree can be considered a probable PKD3 family. Forensic testing confirmed the relationship between the family members.
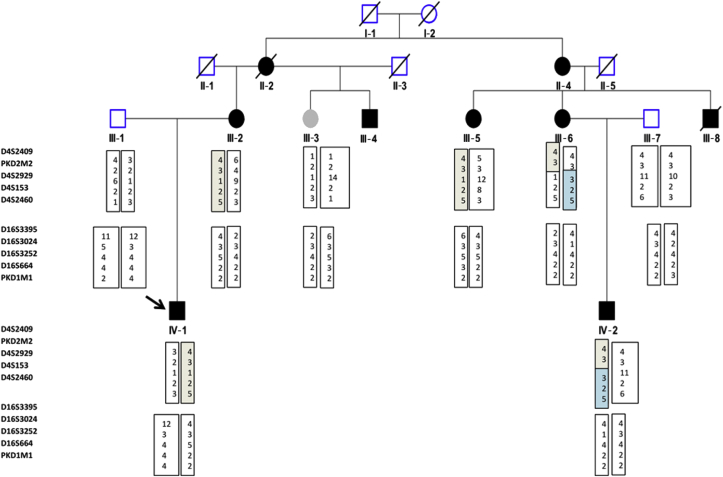
Pedigree and haplotype data of family P-13. Black boxes indicate the common PKD2 haplotype among affected individuals. Individual III-3 was suspected to be affected. Break in haplotype boxes shows the recombination point.
PKD, polycystic kidney disease.
Mutation screening of the entire PKD2 gene was performed for better evaluation of the family. Sequencing of all exons and exon boundaries in the proband revealed a splice site mutation, c.1094+1G>A, Ala365fs, in intron 4, which results in a frameshift change after alanine 365 (Fig. 2A). The mutation possibly produces the truncated protein, which results in a loss-of-function effect. It is classified as definitely pathogenic according to the ADPKD Mutation Database (http://pkdb.mayo.edu/cgi). This mutation was also described in 1 Korean [19] and 1 French family [9] previously. We also identified 1 synonymous variant in exon 1, c.420G>A, p.G140G, along with 2 intronic and 1 3′UTR (untranslated region) variants (Table 3). Designing longer PCR amplicons made it possible to identify deep intronic and untranslated regions' variants.
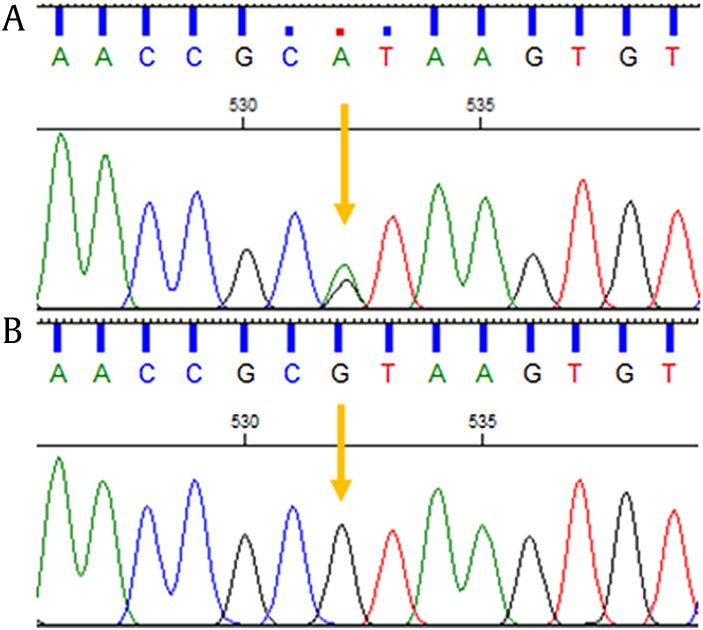
The Sanger sequencing electropherograms. Proband with heterozygous mutation c.1094+1G>A (A). Individual III-3 with normal alleles (B).
Correct segregation of the mutation with the disease was confirmed by analyzing 2 healthy and 4 clinically affected (1 men and 3 women) individuals including the IV-2. The proband semi-aunt (III-3) shows 2 normal alleles (Fig. 2B).
Once more (PND), precise inspection of haplotypes proposed the probability of 1 crossing over between the PKD2 intragenic and the adjacent downstream marker (D4S2929) in the III-6 individual. At first glance, it seems that his affected son inherited the normal maternal haplotype (Fig. 1). Actually, the occurrence of crossing over in the mother could not be distinguished easily because of the homozygosity of the first 2 microsatellite markers, despite their high heterozygosity (Table 1).
Discussion
Herein, we evaluated the ADPKD family that first appeared to be unlinked to both PKD1 and PKD2 genes because of recombination and identified the pathogenic mutation (c.1094+1G>A, Ala365fs) in all affected members. In addition, we showed the worthiness of mutation detection in ADPKD diagnosis, especially in mildly symptomatic individuals of PKD2 families.
Haplotype segregation analysis of polymorphic microsatellite markers is an efficient methodology. Besides various applications, it is used as the indirect genetic diagnosis tool in heterogeneous genetic disorders, before or along with direct mutation detection.
By linkage analysis, the responsible gene can be determined without the need to detect the causative mutations, but this approach needs the cooperation of other affected and unaffected members of the family, and it cannot be used in sporadic cases. In addition, the clinical states of all the participants must be established definitively. In comparison to the challenging procedure of PKD1 and PKD2 mutation screening, linkage analysis will reduce the time and expense of analysis, which is more prominent in PKD2-linked pedigrees. Furthermore, it is recommended in PGD and prenatal genetic diagnosis for detecting maternal contamination and as a second method to confirm the results [20]. Nevertheless, there are different factors that can confuse the analysis. Here, we mentioned the most important ones.
First of all, microsatellite genotyping itself encountered some challenges including sizing precision, allele calling, and the dye shift error [21]. Furthermore, there is another source of error, allelic dropout, which is failure in amplification of 1 or 2 alleles, resulting in mistaken report of homozygous instead of heterozygous or missing data [22]. One solution is repeating the procedure; so here, all homozygous results were confirmed by regenotyping. In regard to linkage analysis, locus heterogeneity, clinical misdiagnosis, mosaicism, de novo mutations, and recombination encompass the most important confounders. There are examples of pedigrees unlinked to both PKD1 and PKD2 loci because of coinheritance of mutation in both genes [10], [23], homozygous hypomorphic PKD1 alleles [24], mosaicism [25], [26], and de novo mutation.
In our pedigree, the noninheritance of the PKD2 common haplotype in the individual IV-2 could be due to the nonpaternity, another reason which can cause discrepancy in the familial segregation analysis. Therefore, the biological relationship within the family was investigated by an in-house panel of 24 short tandem repeat markers.
Precise inspection revealed that occurrence of 1 recombination event between 2 adjacent maternal STR markers could explain the observed haplotype in IV-2. Recombination events could be distinguished easily in the case of heterozygosity of all the STR markers and complete informativeness of the pedigrees. Although the recombination rates vary over the human genome, 1.55 cM/Mb is estimated in females. Selecting closely, STR markers can reduce the chance of recombination. Here, the physical distance of 2 adjacent markers was about 200 Kb, whereas according to the Marshfield map, the genetic distance to telomeric end was 96.2 cM for both markers (http://research.marshfieldclinic.org). As we see, recombination can still be happening in spite of neighboring markers. Therefore, more caution must be taken in interpreting the haplotype data especially in the prenatal genetic diagnosis and PGD cases.
Informativeness of haplotype analysis is a factor of microsatellite marker heterozygosity. Here, selecting additive flanking markers may increase the haplotype informativeness and help distinguishing the recombination event. Meanwhile, there is very little information about the heterozygosity of PKD2 flanking STR markers in Iranian population; in addition, selecting distant markers would increase the chance of recombination itself.
The blood sample of II-4 was not available, although it can reveal the beginning of the recombination event. She was 70 years old and was being dialyzed for 5 years. The late age of end-stage renal disease (ESRD) in the family is consistent with the milder characteristics of PKD2 gene. She was the only person who reached the end-stage renal disease in the family. Her affected son died at the age of 45 years because of stroke. No more clinical data were accessible. There was no history of any liver, bladder, prostate, or ovarian cysts. III-2 had taken medication for hypertension.
Individual III-3 was a 47-year-old woman with equivocal ultrasound renal findings, normal liver (size and density), and intact spleen, pancreas, and gall bladder. Although the sensitivity of imaging techniques in ADPKD diagnosis is about 90%, especially in mild PKD2 families [27], she did not match the ultrasound criteria for inclusion of ADPKD [28]. Here, mutation screening can unambiguously rule out the disease.
Because haplotype analysis obviously excluded linkage to PKD1 gene, PKD2 direct mutation analysis was performed at the first step, which leads to the identification of the pathogenic mutation.
In conclusion, genomic recombination is one of the confounders that lead to misinterpretation of haplotype and linkage data. Selecting closer or more intragenic markers, whenever possible, as well as highly polymorphic markers, could overcome misdiagnosis. In the case of confusing results, direct mutation screening can identify the causative mutation in the pedigree. Here, the splicing mutation c.1094+1G>A in PKD2 was detected as a pathogenic mutation in all affected members of presumably unlinked PKD1 and PKD2 family. Furthermore, genetic diagnosis can exclude the disease in 1 member with equivocal imaging results.
Conflicts of interest
All authors have no conflicts of interest to declare.
References
Acknowledgments
The authors are very thankful to the participants for their kindness and collaboration.
Notes
The work is attributed to Department of Medical Genetics, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran.


