Kidney transplantation in highly sensitized recipients
Article information
Abstract
In kidney transplantation (KT), overcoming donor shortage is particularly challenging in patients with preexisting donor-specific antibodies (DSAs) against human leukocyte antigen (HLA), called HLA-incompatible KT (HLAi KT), carrying the risk of rejection and allograft loss. Thus, it is necessary to accurately evaluate the degree of sensitization before HLAi KT, and undertake appropriate pretreatment strategies. To determine the degree of sensitization, complement-dependent cytotoxicity has been the only method employed; the development of a method using flow cytometry further improved the test sensitivity. However, these tests present disadvantages, including the need for living cells, with a solid-phase assay developed to resolve this problem. Currently, the method using Luminex (Luminex Corp.) is widely used in clinical practice. As this method measures DSAs using single antigen beads, it is possible to classify immunological risks by measuring the type and amount of DSAs. Furthermore, there have been major advances in methods that involve DSA removal before HLAi KT. In the early stages of desensitization, plasmapheresis and intravenous immunoglobulins were the main treatment methods employed; however, the introduction of CD20 monoclonal antibody and proteasome inhibitors further increased the success rate of desensitization. Currently, HLAi KT has been established as an important transplant method, but an understanding of DSAs and a novel desensitization treatment are warranted.
Introduction
Kidney transplantation (KT) is a well-known treatment strategy that best improves the quality of life and survival outcomes in patients with end-stage kidney disease (ESKD) [1]. However, although the number of patients with ESKD is markedly increasing worldwide, the number of living donors is limited, resulting in a growing number of patients on waiting lists for transplantation [2,3]. To overcome this donor shortage, KT in ABO-incompatible (ABOi) or sensitized patients has been attempted to increase the potential living donor pool. In the Republic of Korea, ABOi KT was initiated in 2007 and has been rapidly increasing [4]. Furthermore, a case of successful KT was reported in the Republic of Korea in 2002 after plasmapheresis was performed in a patient who had a positive crossmatch test with a living donor [5], and KT in highly sensitized recipients is currently being actively implemented across several centers.
KT in recipients with alloantibodies to donor human leukocyte antigens (HLAs) is termed HLA-incompatible (HLAi) KT. The presence of alloantibodies against HLAs of potential donors was previously considered a major barrier to KT [6]. However, as new technologies for measuring the characteristics and strength of these donor-specific antibodies (DSAs) have emerged since the early 2000s, immunologic risk stratification has been possible in highly sensitized recipients [7] along with advances in desensitization treatment. Accordingly, a highly sensitized status as a barrier to KT is being surpassed by these developments, which are being actively implemented to overcome donor shortage [8].
In this review, we describe the pretransplant alloantibody detection, desensitization treatment, allograft and patient outcomes, and our center’s experiences and outcomes in HLAi KT.
Alloantibody detection
To evaluate highly sensitized recipients and to implement appropriate treatment regimens, it is crucial to first understand the various tests for immunologic risk stratification. Successful KT can be achieved by identifying preformed DSAs through complement-dependent cytotoxicity (CDC) crossmatch, flow cytometry crossmatch (FCXM), and solid-phase binding assay (SPA), and reaching the appropriate target antibody range before transplantation [9]. As large differences in sensitivity and specificity exist between these tests, individualized immunologic risk stratification is generally performed by employing a combination of test results [10].
Complement-dependent cytotoxicity crossmatch
CDC crossmatch is a traditional test that was first employed as a pretransplant immunological test and remains a routinely performed test until now [6]. This test can detect whether complement-fixing immunoglobulin (Ig) M and IgG antibodies targeting donor lymphocytes are present in the recipient’s serum [11]. Typically, the test result is positive only when there are sufficient antibodies that can bind to the donor antigen and activate the complement cascade; hence, the sensitivity of CDC crossmatch is relatively inferior when compared with other tests [12].
The CDC crossmatch has several limitations. This test can only detect complement-fixing antibodies, requires viable donor lymphocytes for testing, and the sensitivity may vary depending on the rabbit complement batch. To overcome these limitations, various techniques have been employed [12]. Prolonging the incubation time to 120 minutes after adding the complement can increase the test sensitivity. The Amos wash technique is used to increase test sensitivity and detect only clinically meaningful IgG antibodies by removing anticomplementary factors and low-affinity IgM antibodies by washing the unbound antibodies from the cell suspension before adding complement [13]. The anti-human globulin (AHG) augmentation method is widely used to increase test sensitivity by adding an anti-kappa light chain. AHG enhances complement activation via the proximity of the Fc portion of the antibody. Therefore, detection of low-titer anti-HLA antibodies and non-complement-fixing antibodies is feasible [14]. Pretreatment of patient serum with dithiothreitol or dithioerythritol removes disulfide bonds from the IgM pentamer, but IgG remains relatively intact; hence, IgG and IgM antibodies can be distinguished [15].
Despite these efforts, CDC crossmatch is a reaction between a patient’s serum and donor lymphocytes; hence, the specific profile of the antibody cannot be identified, and false positives may be demonstrated by non-HLA antibodies that are not pathogenic [16]. Furthermore, this test may be affected by drugs or the patient’s underlying disease, with false positives detected owing to the patient’s autoantibodies [17]. Moreover, rituximab can be detected in a patient’s serum for more than 3 months; hence, the B-cell CDC crossmatch can produce false positives during this period [18]. Nevertheless, the CDC crossmatch test remains meaningful as it can stratify high immunologic risks and can be used to reevaluate pretransplant immunologic risks after appropriate desensitization treatment.
Flow cytometry crossmatch
Although CDC crossmatch is effective in avoiding hyperacute rejection, several transplant patients have revealed poor clinical outcomes such as primary non-function and delayed graft function. This could be attributed to low-titer DSA, which is lower than the detection threshold of conventional CDC crossmatch in sensitized patients. Garovoy et al. [19] identified low-titer IgG DSAs by the FCXM method, which was not observed in CDC crossmatch. FCXM is a more sensitive test than CDC crossmatch, and it was reported that the incidence of delayed graft function, acute rejection, and graft failure was higher in the case of FCXM-positive with CDC crossmatch-negative than that of both negatives before transplantation, suggesting that weak and sublytic DSAs play a pathogenic role [20].
FCXM is a cell-based method in which donor lymphocytes react with the recipient serum, similar to CDC crossmatch. However, unlike CDC crossmatch, in this method, the flow cytometer signal is read by adding fluorochrome-conjugated antibodies rather than by employing a cytotoxic response [21]. In some laboratories, donor lymphocytes are pretreated with pronase to remove Fc receptors and CD20 from the B-cell surface. By removing the Fc receptor on the B-cell surface, background noise that may occur due to binding of non-HLA antibodies can be removed; removal of CD20 can reduce the effect of rituximab on B-cell FCXM [22].
As a significant proportion of patients reportedly presented an uneventful clinical course, although they were FCXM-positive, FCXM is considered a test with high sensitivity and low specificity in early graft dysfunction and antibody-mediated rejection (ABMR) [23]. Furthermore, FCXM can be impacted by several variable factors, including flow cytometers, fluorochrome reagents, cell-to-serum ratio, and incubation conditions, rendering standardization difficult. It is necessary to establish individual cutoff values for each laboratory [24]. Moreover, the problem of false positives induced by non-HLA antibodies, autoantibodies, and rituximab tends to persist, which are disadvantages associated with traditional CDC crossmatch [23].
FCXM results must be interpreted together with the CDC crossmatch results (Table 1). For example, when only T-cell CDC and T-cell FCXM results are positive, this may indicate T cell-specific antibody but probably not IgG HLA class I antibody; T-cell FCXM-negative and only B-cell FCXM-positive may indicate the presence of class II DSAs, low-titer class I DSAs, autoantibodies, or antibodies against major histocompatibility complex class I-related chain A [25]. Therefore, CDC and FCXM test results must be interpreted in combination with the SPA test described later to obtain accurate information regarding immunologic risks in sensitized patients.
Solid-phase binding assays
Advances in the SPA method have greatly contributed to the increased sensitivity and specificity of HLA antibody detection [7]. The first SPA techniques were enzyme-linked immunosorbent assay and flow cytometry, but recently, these have been largely superseded by "Luminex" technology (Luminex Corp., Austin, TX, USA), which uses polystyrene microbeads with attached purified HLA proteins. The panel reactive antibody (PRA) test is a method to screen anti-HLA antibodies present in the recipient’s serum using a pooled antigen panel composed of microbeads of HLA class I or class II antigens, obtained from multiple donors. A single antigen bead (SAB) panel is the most sensitive test method because each bead is coated with only one HLA allelic antigen, presenting the advantage of being able to detect specific DSAs [26]. Therefore, it is recommended that highly sensitized recipients perform at least one SAB assay before transplantation [24].
Antigen-coated microbeads are incubated with the recipient’s serum, followed by addition of fluorescent-labeled anti-human IgG. If anti-HLA antibodies are present in the recipient’s serum, they bind to the microbeads, and as fluorescent-labeled anti-human IgG binds sequentially to anti-HLA antibodies, it can be detected using a dual-laser instrument [24]. Luminex SAB provides semiquantitative information regarding the anti-HLA antibody titer through median fluorescence intensity (MFI) values, which are used as important information in pretransplant immunologic risk assessment [27]. Luminex SAB may present false-positive or false-negative results owing to IgM or various inhibitory factors present in the recipient’s serum. However, these limitations can be overcome through hypotonic dialysis, heat inactivation, or pretreatment with dithiothreitol or ethylenediaminetetraacetic acid [28].
However, as Luminex SAB is a semiquantitative test, results should be interpreted by utilizing professional knowledge rather than absolute values. In particular, as the coefficient of variance of the MFI values exceeds 25%, a change of less than 1,000 or less than 25% of the MFI values should not be interpreted as clinically significant [27]. Additionally, the prozone phenomenon may occur at markedly high antibody titers. The high titer of antibodies interferes with the formation of the antibody-antigen complex, resulting in a false-negative result. This is clinically indicated by a strong positive CDC crossmatch result, with a negative SAB assay result. In this case, when the recipient’s serum is diluted, the SAB assay results in an increase in the MFI values, allowing antibody detection [29]. The presence of antibodies against the shared epitope in the recipient’s serum may result in false-positive results for multiple microbeads representing HLA antigens [30]. Furthermore, the SAB assay is an extremely sensitive test and does not show ABMR or poor allograft survival in all patients with detected DSAs [31,32]. Therefore, to detect cytotoxic DSAs, a modified test method (C1q binding assay, C3d binding assay) that detects antibodies capable of complement activation is currently being implemented [33].
As the SAB assay can detect specific antibodies, calculated PRA (cPRA) can be derived. cPRA is an index that evaluates the actual degree of sensitization by reflecting the HLA antigen frequencies of the population and can be extremely important in counseling the waiting time of highly sensitized recipients waiting for deceased donors [34]. Furthermore, virtual crossmatching is possible by comparing the recipient’s specific anti-HLA antibodies and donor HLA typing results. The deceased donor allocation time can be reduced by allowing the compatible donor-recipient combination to be checked in advance before the actual crossmatch test [35]. In addition, the SAB assay can be used for monitoring de novo DSA, allowing proper patient management after transplantation [36].
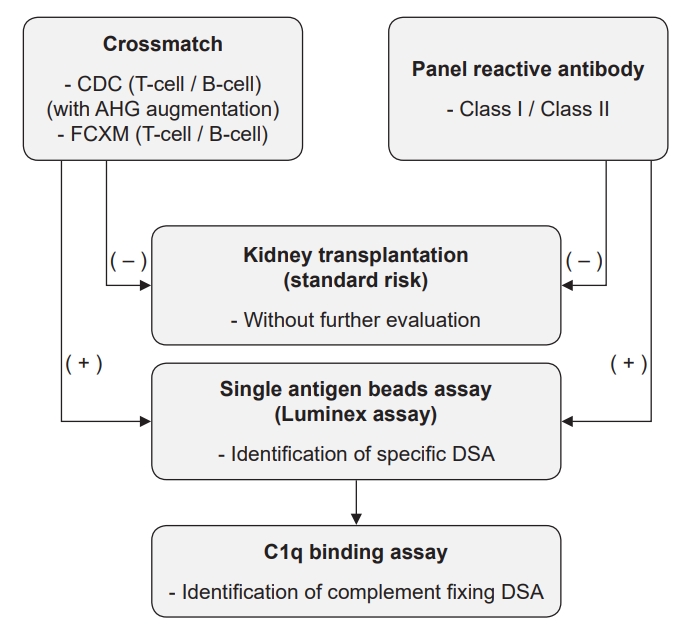
Individualized pretransplant immunologic risk assessment is possible by using the results of previously described CDC crossmatch, FCXM, and SAB assays collectively. By interpreting these test results together, the immunologic risk of sensitized patients can be stratified into the high-risk group (the probability of hyperacute rejection is high if antibody reduction therapy is not performed owing to high-titer DSAs), the intermediate-risk group (the probability of hyperacute rejection is low, with a higher probability of ABMR and poor allograft outcome), and the low-risk group (the incidence of rejection may be high owing to low-titer DSAs, but the evidence for poor allograft outcome is insufficient) [10] (Table 2). At our center, as immunologic risk evaluation, crossmatch and PRA are used as screening tests to identify the presence of anti-HLA antibodies; if the screening test is positive, the SAB assay is performed to identify specific DSAs (Fig. 1).
Future direction
As the development of the SAB assay allows the identification of specific DSAs, there has been great progress in evaluating the degree of sensitization. However, some challenges need to be further addressed [37].
Complement-binding assays determine whether DSA can activate the complement cascade. This has been reported as a valuable test for pretransplant immunologic risk stratification, predicting ABMR and graft loss occurrence [38,39]. Several studies have reported that complement-binding DSA has a strong correlation with high antibody titers (high MFI levels) [40,41]. However, since the antibody titer can change dynamically, the complement-binding assay can show inconsistent results [40]. In addition, in a previous study, ABMR with DSA did not show complement fixation in vitro, but 40% of them showed C4d-positive histology in vivo [42]; thus, further research is needed on this.
It is thought that the mechanism of alloimmune response is different depending on the IgG subclass. IgG1 and IgG3 subclasses are known to have stronger complement-fixing properties than IgG2 and IgG4 subclasses [43]. Furthermore, previous studies have reported that IgG1 and IgG3 subclasses are strongly related to acute rejection and graft loss [44,45]. However, there is a technical limitation that the currently used IgG subclass-specific reagents cannot classify subclasses in 10% to 20% of total IgG-positive HLA antibodies [44]. In addition, IgG2 and IgG4 are also known to have some correlation with rejection [46]; therefore, further research is warranted.
Progress is being made in uncovering the outside-in signal transduction pathway by DSA. As the mechanistic target of rapamycin signaling axis is revealed as a pathway for activation of endothelial cells by HLA class II molecules [47], research on the development of diagnostic tools and drugs using this is expected. In addition, the relationship between the Fc receptor genotype and HLA subclass in leukocyte recruitment and microcirculation inflammation has been reported [48], and the pathological mechanisms for this are expected to be uncovered in the future.
DSA is not observed, but the presence of previously sensitized memory B/T cells may induce a rapid alloimmune response after transplantation [49]. Therefore, attempts are being made to discover these memory B/T cells before transplantation. Test methods such as flow cytometric HLA-binding memory B-cell assay, in vitro differentiation of memory B-cell assay, donor-specific interferon-γ secreting T-cell assay, follicular helper T-cell assay, immunophenotypic bulk memory T-cell assay have been attempted, but there are no tests showing clinically useful predictable power to date [50–54].
HLA allorecognition by B/T cells is more likely to occur as recipient HLA and donor HLA molecules are more different [55]. Currently, computational algorithms can be used to quantify the HLA molecule mismatch (mMM) between the recipient and donor. Commonly used methods are HLA Matchmaker, Electrostatic Mismatch Score, Predicted Indirectly ReCognizable HLA Epitopes Matching, and simple counting of amino acid mismatches [56–58]. In previous studies, the HLA-DR or -DQ mMM score was an independent risk factor for de novo DSA, and it has been reported that both simple HLA type mismatch and mMM are important for pretransplant immunologic risk stratification [59]. However, since various mMM calculation systems currently exist, standardization is required. Moreover, some mMMs have been reported to have stronger immunogenicity than other mMMs, necessitating further research on this [57,60].
Desensitization treatment
Currently, desensitization is performed by removing preexisting antibodies and inhibiting the production of antibodies (Fig. 2). Plasmapheresis, immunoadsorption, high-dose intravenous immunoglobulin (IVIG), and plasmapheresis with low-dose IVIG methods are available to remove existing antibodies [61]. With the introduction of drugs that inhibit the production of antibodies, the success rate of desensitization treatment has increased. As such, CD20 monoclonal antibody that removes B cells or a proteasome inhibitor, which induces apoptosis of plasma cells, can be employed. The most widely used method for desensitization treatment worldwide is plasmapheresis with low-dose IVIG [62] in conjunction with rituximab [8]. Our center also uses a desensitization protocol based on plasmapheresis with low-dose IVIG with rituximab (Fig. 3A) [63]. If T-CDC-AHG is positive or if there is no appropriate DSA MFI titer reduction even after three or more plasmapheresis sessions, a bortezomib-added protocol is performed (Fig. 3B) [64]. In the case of PRA ≥ 50% alone (with crossmatch-negative and DSA MFI titer < 3,000), only rituximab is administered 7 days before transplantation without plasmapheresis [65].
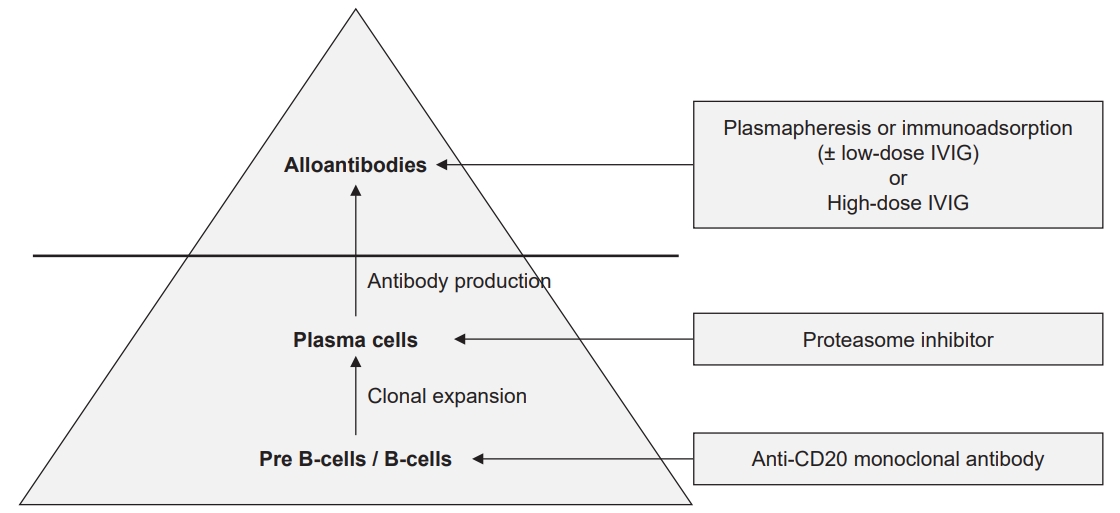
Basic concept of desensitization treatment in highly sensitized recipients.
IVIG, intravenous immunoglobulin.

The desensitization protocol of Seoul St. Mary’s Hospital.
(A) Standard desensitization protocol. The target goals were T-CDC and T-FCXM-negative conversion, DSA MFI titer less than 3,000, and C1q binding assay negative conversion. (B) Bortezomib-based desensitization protocol. If T-CDC or T-AHG is positive, or if there is no adequate DSA reduction after three or more PP/IVIG sessions, bortezomib-based protocol is performed. The target goals were T-CDC and T-FCXM-negative conversion, DSA MFI titer less than 3,000, and C1q binding assay negative conversion.
AHG, anti-human globulin; ATG, antithymocyte globulin; CDC, complement-dependent cytotoxicity; D, day; DSA, donor-specific antibody; FCXM, flow cytometry crossmatch; KT, kidney transplantation; MFI, median fluorescence intensity; IVIG, intravenous immunoglobulin; PP, plasmapheresis; XM, crossmatch.
aBasiliximab is administered at 20 mg/day on days 0 and 4. ATG is administered at a dose of 1.5 mg/kg/day from day 0 to day 4 for 5 days.Plasmapheresis or immunoadsorption
Plasmapheresis or immunoadsorption is a method that physically removes immunoglobulins from the recipient’s serum. As a desensitization method, plasmapheresis is mainly performed in the United States, and immunoadsorption is mainly performed in Europe. As in the United States, plasmapheresis is currently the main method undertaken in the Republic of Korea. Plasmapheresis is not specific to the removal of alloantibodies, and hence, all plasma proteins, including albumin and blood coagulation factors, are lost, which need to be replaced with albumin or fresh frozen plasma. Immunoadsorption utilizes columns that selectively remove the immunoglobulin, preventing excessive loss of coagulation factors [66]. Reportedly, one treatment session with plasmapheresis or immunoadsorption can result in an alloantibody reduction between 15% and 20%, and alloantibody levels are reduced by more than 90% with 3 to 6 treatment sessions. However, rebound anti-HLA antibody titers can be detected within 4 weeks after the completion of plasmapheresis or immunoadsorption [67].
Intravenous immunoglobulin
IVIG is a preparation that is produced by separating the gamma globulin fraction of pooled human plasma and is employed to treat various autoimmune diseases or hypogammaglobulinemia. The mechanism of action of IVIG in desensitization treatment remains unclear, but it is considered that IVIG modulates the immune response through various pathways [68]. These complex mechanisms could involve the neutralization of cytokines and antibodies, inhibition of B/T cells through the saturation of Fc receptors, increased regulatory T cells, inhibition of immune complex formation, and inhibition of dendritic cell activity [69]. In a retrospective study that directly compared high-dose IVIG (2 g/kg) and plasmapheresis with low-dose IVIG (100 mg/kg) as desensitization treatment in T-CDC crossmatch-positive recipients, the proportion of patients who achieved crossmatch negativity was 38% in the high-dose IVIG group and 84% in the plasmapheresis with low-dose IVIG group [70]. The incidence of ABMR was 80% in the high-dose IVIG group and 37% in the plasmapheresis with low-dose IVIG group; hence, plasmapheresis with low-dose IVIG was reported to be a better desensitization treatment method [70]. However, in another large-scale study, the comparable success rate of high-dose IVIG and rituximab combination therapy has also been reported [8], and high-dose IVIG can have an advantage over plasmapheresis, as there is no concern regarding the loss of other plasma proteins. Currently, at our center, highly sensitized patients waiting for deceased donors are undergoing high-dose IVIG therapy (1 g/kg/day for 4 days [at day 1, day 2, day 30, day 31] for the removal of anti-HLA antibodies.
Anti-CD20 monoclonal antibody
Rituximab is a monoclonal antibody against CD20 expressed on the surface of B cells and their progenitor cells. It removes B cells present in the peripheral blood and spleen and inhibits their differentiation into plasma cells, thereby suppressing antibody production. In highly sensitized patients, administration of rituximab significantly reduced re-elevation of anti-HLA antibody titers after KT [71]. However, as plasma cells do not express CD20, they cannot be removed with rituximab, and hence, the effect of rituximab may be insufficient in plasma cells that continuously generate antibodies [71]. Nevertheless, to date, rituximab is the most widely used agent to inhibit antibody production during desensitization treatment.
Proteasome inhibitor
Bortezomib is a reversible 26S proteasome inhibitor that inhibits the migration of nuclear factor-kappa B to the cell nucleus, thereby inducing apoptosis of plasma cells [72]. The bone marrow niche resident long-lived plasma cells are known to continuously produce anti-HLA antibodies, which do not express CD20 and are not removed by rituximab [73]. Therefore, desensitization treatment via additional administration of bortezomib targeting plasma cells has been attempted when conventional desensitization treatment does not respond sufficiently, or the antibody titer is markedly high [74]. Carfilzomib is a second-generation irreversible proteasome inhibitor. In a recent study, it was reported that the carfilzomib monotherapy-based desensitization protocol showed acceptable safety and toxicity with significant bone marrow plasma cell depletion and DSA reduction [75]. In highly sensitized patients awaiting a deceased donor, it has been reported that the chance of deceased donor KT was increased by lowering the DSA titer through desensitization using high-dose IVIG, rituximab, and bortezomib [76]. Our center has also been performing this desensitization protocol since 2019, and to date, three deceased donor KTs have been successfully performed.
Novel agents
Eculizumab is a monoclonal antibody against complement C5 that prevents the separation of C5a and C5b, and finally inhibits the formation of the membrane attack complex C5b–C9. Therefore, it could prevent allograft damage by inhibiting the complement cascade. In a study comparing an eculizumab treatment group and the historical control group in crossmatch-positive recipients, the incidence of acute ABMR after KT was significantly lower in the eculizumab treatment group than in the historical control group [77]. However, a large-scale study is still lacking, and further studies are needed.
C1-esterase inhibitor (C1-INH), another complement inhibitor, inhibits the classical and lectin complement pathways by inhibiting C1r and C1s. A randomized phase I/II study compared C1-INH with placebo to prevent acute ABMR in HLAi KT. Twenty recipients who underwent IVIG, rituximab, with or without plasmapheresis before KT, were compared by dividing them into C1-INH and placebo groups. There was no ABMR in the C1-INH group, but one ABMR was reported in the placebo group [78]. It is thought that C1-INH, to some extent, contributes to the prevention of ABMR in highly sensitized patients, but further studies are needed.
Interleukin-6 is a cytokine that induces inflammation through various mechanisms, including the differentiation of B cells into plasma cells. In a previous study using an anti-interleukin-6 receptor blocker (tocilizumab) as desensitization treatment, it was revealed that successful desensitization was possible when tocilizumab was administered to patients who failed to be desensitized following high-dose IVIG and rituximab [79]. Additionally, in KT recipients with chronic ABMR, a significant decrease in the DSA titer was observed when tocilizumab was administered in patients whose DSA titer did not decrease following standard therapy (IVIG + rituximab with or without plasmapheresis). Tocilizumab is expected to contribute not only to desensitization but also to chronic ABMR treatment [80].
Belatacept is a fusion protein that inhibits costimulatory signals in T-cell activation by binding to CD80/CD86 molecules of antigen-presenting cells. It is attracting attention as a new maintenance immunosuppressant [81]. In a recent human in vitro study, it was reported that belatacept inhibits plasmablast differentiation and immunoglobulin production by acting independently on B cells [82]. In a recent retrospective cohort study of highly sensitized recipients (cPRA ≥ 98%), the belatacept group showed a significant decrease in HLA class I antibodies, suggesting that belatacept may be an option for desensitization.
The IgG-degrading enzyme of Streptococcus pyogenes (IdeS) is a cysteine endopeptidase that divides IgG into F(ab’)2 and Fc to neutralize antibodies. It reportedly acts rapidly and neutralizes most of the IgG within 4 hours of administration [83]. In the United States and Sweden, 24 out of 25 highly sensitized recipients reported successful deceased donor KT after IdeS administration. One patient presented with hyperacute rejection, but it was presumed to be caused by unrecognized IgM, IgA, or non-HLA antibodies as no detectable IgG DSAs were observed after IdeS administration [84]. IdeS is currently being investigated in a clinical trial and is expected to play an important role as a desensitization tool in highly sensitized recipients in the future.
Alternative to desensitization (kidney paired donation)
Kidney paired donation (KPD) is a method of performing KT without desensitization in highly sensitized recipients through compatible recipient-donor pair matching in recipient and donor pool [85]. The KPD program has been developed in many countries over the past 30 years, and recent data from KPD registries in Australia and Canada reported that the KT match rates of recipients with cPRA between 50% and 96% and recipients with cPRA < 50% were similar [86]. In a recent study comparing the KPD network program (National Kidney Registry) and all national transplants registry (United Network for Organ Sharing) in the United States, KT performed through the KPD network program showed a higher proportion of retransplantation and highly sensitized recipients (cPRA > 80%) [87]. In a study that analyzed how highly sensitized recipients received KT in the United States from 2009 to 2017, it was observed that living donor KT through KPD gradually increased, which is thought to be due to the development of the KPD program [88].
Allograft and patient outcomes
Table 3 summarizes the studies on HLAi KT to date. As highly sensitized recipients present preexisting alloantibodies before KT, the ABMR incidence was higher than in those without alloantibodies [89]. Consequently, HLAi KT has a significantly lower allograft survival rate than HLA-compatible KT (HLAc KT), which has been reported to be significantly reduced from 1 year of transplantation (89.9% in HLAi KT vs. 97.6% in HLAc KT) [90].
HLAi KT poses concerns regarding increased rejection and worse allograft outcomes, as well as increased infection and malignancy risks due to desensitization treatment. Until now, most studies on the risk of desensitization treatment have been short-term studies; hence, the impact of the long-term risk of desensitization treatment remains unclear. Inconsistent results have been reported on the effect of desensitization treatment on infection risk [91–94]. Kahwaji et al. [93] reported that there were no differences in bacterial, viral, and fungal infection rates between the rituximab with high-dose IVIG group and the non-administered group over 18 months after transplantation. Conversely, Ko et al. [92] reported that desensitization treatment was an independent risk factor for infection-related mortality (adjusted hazard ratio, 3.40; p = 0.002) in a nationwide cohort study in the Republic of Korea. In a recent phase 2 randomized controlled trial comparing the eculizumab-added group and the standard desensitization (plasmapheresis + IVIG or plasmapheresis alone) group in HLAi KT, it was reported that the overall infection rate was numerically higher in the eculizumab-added group (62.7% in the eculizumab group vs. 49.0% in the standard desensitization group) [95]. Few studies have highlighted the malignancy risk associated with desensitization treatment in HLAi KT. In previous studies, nonmelanoma skin cancer and lymphoproliferative disorder were common in the desensitization treatment group [96], with urothelial carcinoma particularly common in the Asian population [97].
DSA titers at the time of transplantation and allograft survival were found to be correlated [63,98]. In an observational study of living donor KT patients at 22 centers of United States, the overall graft survival rates at 1 year and 5 years of transplantation were highest in HLAc KT, the second in the positive SAB (Luminex) assay with negative FCXM (PLNF) group, the third in the positive FCXM with negative CDC crossmatch (PFNC) group, and the lowest in the positive CDC crossmatch (PCC) group. The authors reported that the higher the intensity of sensitization before transplantation, the higher the overall allograft loss rate (Fig. 4) [98]. It is postulated that in addition to the DSA titer, DSA characteristics can affect the allograft outcome. In a patient in whom the C1q binding DSA was converted to negative, but CDC crossmatch remained positive at the time of transplantation, a favorable outcome was observed without evidence of antibody-mediated injury after transplantation [74]. In the future, additional studies on allograft outcomes according to the characteristics of DSA (C1q binding, C3d binding, or IgG subclass) are necessary.

Overall allograft survival rate by crossmatch and SAB assay results at the time of transplantation.
Modified from the article of Orandi et al. (Am J Transplant 2014;14:1573-1580).
PCC, positive complement cytotoxicity; PFNC, positive flow cytometry/negative complement cytotoxicity; PLNF, positive SAB (Luminex, Luminex Corp., Austin, TX, USA) assay/negative flow cytometry; SAB, single antigen bead.
Although HLAi KT has a higher ABMR incidence and lower allograft survival rate than HLAc KT, HLAi KT has advantages over continuing dialysis while waiting for deceased donor KT. Montgomery et al. [62] reported that the HLAi KT group showed more than twice the survival benefit when compared with the dialysis-only group and the dialysis-or-deceased donor KT group in a single-center study. Similarly, Orandi et al. [98] reanalyzed this through the national cohort and reported that HLAi KT demonstrated a better long-term survival rate when compared with dialysis only and dialysis-or-deceased donor KT groups. Although HLAi KT costs approximately $30,000 more than HLAc KT in terms of economics [99], compared to continuing dialysis, HLAi KT increases the quality of life and patient survival and reduces the need for dialysis, making it more cost-effective than continuing dialysis [100].
Our center’s experiences and outcomes
At our center, a total of 137 HLAi KTs were performed from 2010 to 2020. Based on immunologic stratification, 41 patients (29.9%) were PCC, 46 (33.6%) were PFNC, and 50 (36.5%) were PLNF. Among these patients, 41 patients (29.9%) had concomitant ABO incompatibility. Desensitization treatment was performed with rituximab and plasmapheresis with low-dose IVIG according to our center protocol (Fig. 3A). In five patients, the bortezomib-based protocol was performed (Fig. 3B). Antithymocyte globulin was used in 62.0% (85 of 137) and basiliximab in 38.0% (52 of 137) as induction therapy before transplantation. In the posttransplant allograft outcome, de novo DSAs occurred in 10.2% (14 of 137) of patients, and preexisting DSA rebound occurred in 21.9% (30 of 137) of patients. On analyzing biopsy-proven rejection, the acute rejection rate was 30.7% (42 of 137) and the chronic rejection rate was 11.7% (16 of 137). In sub-analysis, the acute T cell-mediated rejection (TCMR) rate was 14.6% (20 of 137), acute ABMR rate was 20.4% (28 of 137), chronic active TCMR rate was 0.7% (1 of 137), and the chronic active ABMR rate was 10.9% (15 of 137). The median follow-up duration was 44.8 months, death censored graft loss rate was 9.5% (13 of 137), overall graft loss rate was 13.9% (19 of 137), and the patient death rate was 8.0% (11 of 137). Following analysis according to the immunological risk group, the overall graft loss rate was 19.5% (8 of 41) in the PCC group, 15.2% (7 of 46) in the PFNC group, and 8.0% (4 of 50) in the PLNF group. It should be considered that the median follow-up duration was 44.8 months, but the overall graft survival of HLAi KT in crossmatch-positive patients at our center was marginally improved compared to previous studies (Table 3).
Conclusion
Highly sensitized recipients are less likely to have deceased donor KT opportunities than non-sensitized recipients. Moreover, in these patients, living donor KT after desensitization treatment reportedly presents a better patient survival rate than that observed with continuing dialysis while waiting for deceased donor KT. Therefore, if a potential donor is available, it is necessary to actively perform HLAi KT. Furthermore, owing to great advances in SAB assays and desensitization treatment in the field of transplantation, it is expected that patient prognosis can be improved through appropriate immunologic risk stratification and desensitization treatment. Moreover, many researches are ongoing in the field of transplant immunity and new agents of desensitization treatment. Based on these findings, in the future, we anticipate that safe KT will be performed even in highly sensitized recipients, thereby actively improving their prognosis.
Notes
Conflict of interest
All authors have no conflicts of interest to declare.
Authors’ contributions
Investigation, Data curation: EJK, BHC
Writing–original draft: YP, CWY
Writing–review & editing: YP, CWY
All authors read and approved the final manuscript.