The Korean Organ Transplantation Registry (KOTRY): an overview and summary of the kidney-transplant cohort
Article information
Abstract
Background
As the need for a nationwide organ-transplant registry emerged, a prospective registry, the Korean Organ Transplantation Registry (KOTRY), was initiated in 2014. Here, we present baseline characteristics and outcomes of the kidney-transplant cohort for 2014 through 2019.
Methods
The KOTRY consists of five organ-transplant cohorts (kidney, liver, lung, heart, and pancreas). Data and samples were prospectively collected from transplant recipients and donors at baseline and follow-up visits; and epidemiological trends, allograft outcomes, and patient outcomes, such as posttransplant complications, comorbidities, and mortality, were analyzed.
Results
From 2014 to 2019, there were a total of 6,129 registered kidney transplants (64.8% with living donors and 35.2% with deceased donors) with a mean recipient age of 49.4 ± 11.5 years, and 59.7% were male. ABO-incompatible transplants totaled 17.4% of all transplants, and 15.0% of transplants were preemptive. The overall 1- and 5-year patient survival rates were 98.4% and 95.8%, respectively, and the 1- and 5-year graft survival rates were 97.1% and 90.5%, respectively. During a mean follow-up of 3.8 years, biopsy-proven acute rejection episodes occurred in 17.0% of cases. The mean age of donors was 47.3 ± 12.9 years, and 52.6% were male. Among living donors, the largest category of donors was spouses, while, among deceased donors, 31.2% were expanded-criteria donors. The mean serum creatinine concentrations of living donors were 0.78 ± 0.62 mg/dL and 1.09 ± 0.24 mg/dL at baseline and 1 year after kidney transplantation, respectively.
Conclusion
The KOTRY, a systematic Korean transplant cohort, can serve as a valuable epidemiological database of Korean kidney transplants.
Introduction
Solid-organ transplantation is the best treatment modality for organ failure in terms of quality of life, medical cost, and long-term survival [1–4]. Allograft survival rates have also substantially improved with the development of effective immunosuppressants over the past number of decades. Maximization of patient and allograft survival necessitates proper management of chronic complications, such as cardiovascular disease and malignancy, as well as quality of life. However, the incidence and prognosis of chronic complications as well as organ-transplantation outcomes may differ according to ethnic and regional differences. For instance, while the leading cause of death among Western kidney-transplant recipients is cardiovascular disease, a major cause of death among recipients from certain Asian countries is infectious disease, with a lower-than-expected incidence of cardiovascular disease [5,6]. In Korean organ-transplant patients, further data is required to determine outcomes and prognoses related to ethnic and regional characteristics.
In Korea, since the legislation of organ transplantation in 1999, a centralized organ-procurement organization system and an organ-allocation system as well as a public organ-donation agency have been established. Therefore, deceased-donor organ donation in Korea is a transparent and systematic process. Although most organ transplantations in Korea are from living donors, the number of deceased-donor organ transplantations increased from 233 cases (1.09 per 1 million people) in 2000 to 1,989 cases (9.72 per 1 million people) in 2015 [7,8]. As the number of organ transplantations increased, the need for a nationwide organ-transplant registry became clear, and a prospective registry, the Korean Organ Transplantation Registry (KOTRY), was initiated in 2014 [9]. Previously, the Korean Society of Transplantation managed a retrospective version of the KOTRY, which included approximately 91.9% of all kidney transplants in Korea, from January 2009 to September 2012 [10]. Subsequently, a second retrospective KOTRY was introduced for kidney-transplant patients from October 2012 to March 2014. The current, prospective KOTRY includes five solid-organ-transplantation cohorts (kidney, liver, lung, heart, and pancreas) and 79 transplantation centers, including 40 kidney centers, 24 liver centers, five heart centers, five lung centers, and five pancreas centers, as of December 2019. In this report, we present the baseline characteristics and outcomes of the kidney-transplant cohort in the KOTRY for 2014 through 2019.
Methods
Study population
The organ recipients in both living- and deceased-donor organ transplantations and the organ donors in living-donor organ transplantations were enrolled in this cohort after informed consent was obtained. Recipients who were <19 years old and those undergoing simultaneous multiorgan transplantation, except for simultaneous pancreas and kidney transplantation, were excluded. However, patients in whom sequential multiorgan transplantation was performed were not excluded from the registry, and there was no age limit in liver transplantation. The individual Institutional Review Boards of participating hospitals approved this cohort study (No. H-1312-087-543), and this study was performed in accordance with the Declaration of Helsinki and the Declaration of Istanbul.
Study design and data collection
For each organ-transplant cohort in the KOTRY, medical data of recipients and donors were prospectively collected and entered into the iCReaT, a web-based data-capturing system developed by the Korean National Institute of Health. From these data, epidemiological trends, allograft-related outcomes, and patient outcomes—including posttransplant complications, comorbidities, and mortalities—were analyzed. For instance, data in the kidney-transplant cohort included demographics, comorbid conditions, laboratory data at baseline, discharge data, immunosuppressant use, laboratory data at follow-up, posttransplant complications, event notification, rejection, biopsy, and infections. Kidney-transplant donor data included demographics, comorbid conditions, laboratory data at baseline, discharge data, laboratory data at follow-up, and event notification. Follow-up data collection was performed first at 6 months after kidney transplantation and then subsequently on an annual basis. To analyze the effect of new-onset comorbidities on posttransplant outcomes, data on posttransplant comorbidities were collected at every follow-up visit for consideration of the number and timing of posttransplant comorbidities. Such comorbidities include cardiovascular events, stroke, malignancy, and fractures. Recently, the KOTRY has added case reports of kidney-transplant recipients infected with coronavirus disease 19 (COVID-19), so we collected the treatment and outcomes data related to COVID-19 in kidney-transplant patients.
To enhance the quality of the data, clinical research coordinators in all participating centers received regular training. In addition, an electronic data-validation system was utilized to provide feedback to clinical research coordinators in each center. A central coordination unit moderated the study process, inspected the weekly registration status, and provided feedback to each participating center. To encourage the collection of follow-up data, newsletters that include details on patient enrollment and follow-up were periodically forwarded to the transplant physicians and surgeons of the participating centers. We also adopted a transfer system where, if an enrolled patient in a center was transferred to another center also participating in the KOTRY, the other center could collect the patient’s data. In addition, the importance of the collection of follow-up data of living donors was periodically communicated to all participating centers.
Sample collection
Blood samples for DNA analysis are collected before transplantation from both recipients and donors. Baseline serum samples from organ recipients were collected before transplantation and at 1 and 3 years after all transplantations, except for liver transplantations. In kidney transplantations, additional plasma samples have been collected from recipients at the same time points since 2017. Collection, quality control, and storage of blood samples were performed by an external company (LabGenomics, Seongnam, Republic of Korea).
Study outcomes
The primary outcomes in this study were graft loss and patient mortality. In the kidney-transplant cohort, graft loss was defined as maintenance dialysis performed for >3 months, retransplantation, or death with a functional graft. Causes of graft loss were classified as rejection, recurrent or de novo glomerulonephritis, postoperative complications, calcineurin-inhibitor toxicity, BK-virus nephropathy, noncompliance, primary graft failure, and others. Graft loss was defined as retransplantation or patient death in the liver-, heart-, and lung-transplant cohorts. In the pancreas-transplant cohort, graft loss was defined as insulin dependence or patient death. Causes of patient death were classified as cardiovascular disease, infection, malignancy, liver disease, sudden cardiac death, accident, suicide, and others.
Secondary outcomes included acute rejection, infection requiring hospitalization, malignancy, cardiac events, stroke, tuberculosis, and fractures in the kidney-transplant cohort. Acute rejection included clinical rejection and biopsy-proven rejection, and treatment methods as well as responses were also recorded. The pathogens causing infection were classified into bacteria, viruses (including cytomegalovirus), mycobacteria, fungi, Pneumocystis jirovecii, and others. The type of malignancy was classified according to the International Classification of Diseases, 10th revision. Cardiac events included acute myocardial infarction, angina (requiring therapeutic intervention or objective clinical findings), and congestive heart failure, and others. Stroke events included ischemic and hemorrhagic brain disease.
In the kidney- and liver-transplant cohorts, outcomes of living donors were collected, including death, cause of death, and surgical morbidities. In kidney-transplant donors, new-onset diseases, such as diabetes mellitus, hypertension, end-stage renal disease, stones in the urinary tract, and other comorbid conditions, were also included in the registry.
Statistical analyses
In the KOTRY cohort study, statistical analysis files are generated three times a year after a data-cleaning procedure. The participating center can request their own data at any time, and the latest validated statistical analysis files are released. If investigators were to request all centers’ data for research, the requested variables would be sent as a de-identified dataset after approval of the study proposal by the organ committee of the KOTRY.
Continuous variables were expressed as mean ± standard deviation values or medians with ranges. Categorical variables were described as numbers and percentages. The chi-square test or Fisher exact test was performed to evaluate differences in categorical variables. The Student t-test or analysis of variance was conducted to evaluate differences in continuous variables. Patient and graft survival, rejection-free survival, cardiac events, new-onset diabetes after transplantation (NODAT), malignancy, and infection were estimated using the Kaplan-Meier method and log-rank test. Significant variables in the univariate Cox regression analyses (p < 0.05) and the variables known to be clinically important in previous studies were entered into a multivariate Cox proportional hazards model to determine which factors were independently predicted several outcomes. Statistical significance was defined as p < 0.05.
Results
Baseline characteristics of registered kidney-transplant recipients
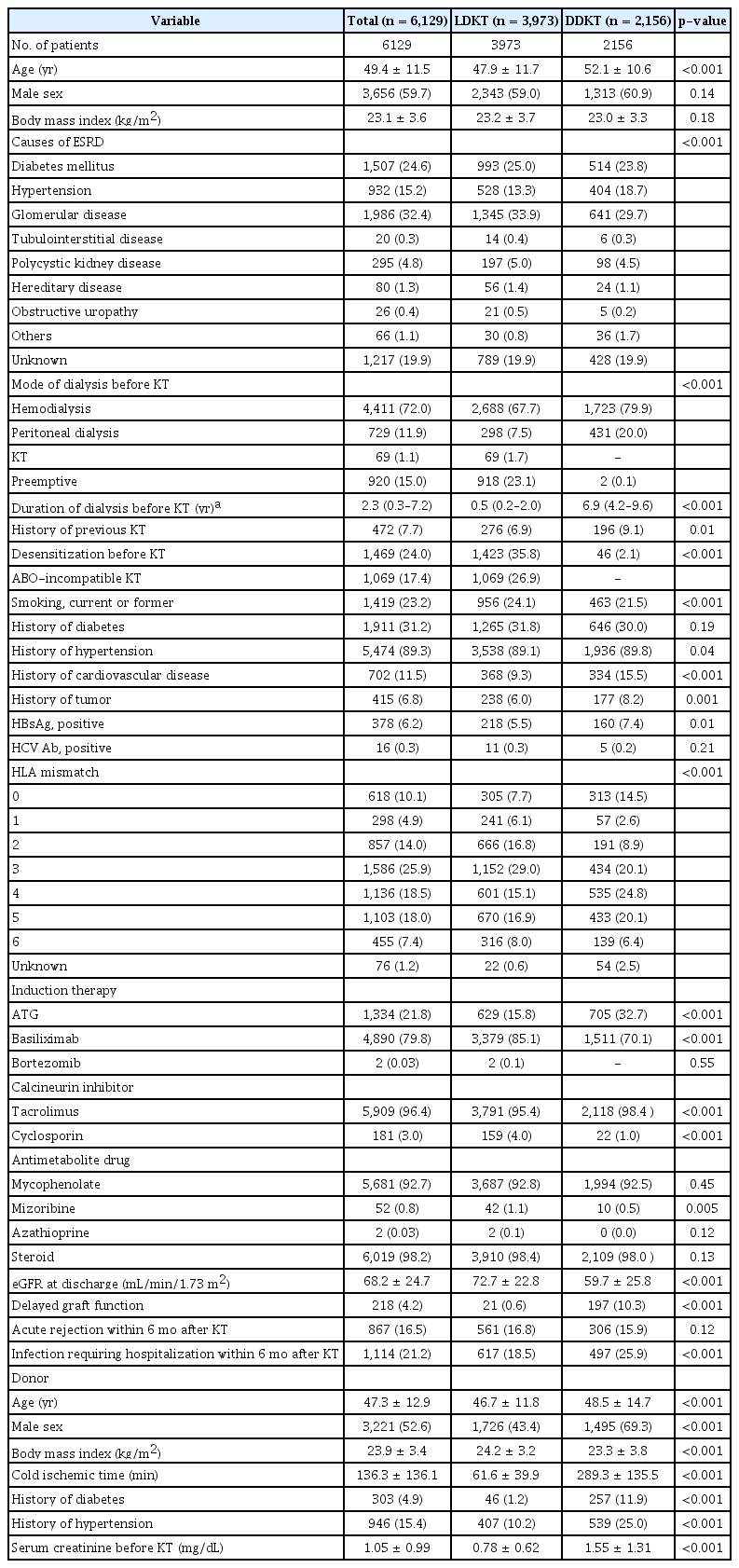
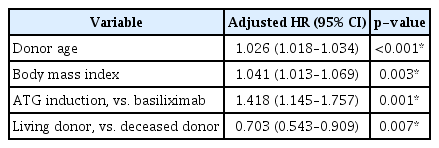
We summarized and analyzed the data of kidney-transplant recipients and donors registered in the KOTRY from 2014 to 2019. There were 6,129 registered kidney transplants, of which 3,973 were living-donor kidney transplants (LDKTs) and 2,156 were deceased-donor kidney transplants (DDKTs) (Fig. 1A). The mean age of the registered recipients was 49.4 ± 11.5 years, with the largest age group being those in their 50s. The mean age of the LDKT group was 47.9 ± 11.7 years, and that of the DDKT group was 52.1 ± 10.6 years. Among all registered recipients, 3,656 (59.7%) were male and 2,473 (40.3%) were female. The proportions of males totaled 59.0% in the LDKT group and 60.9% in the DDKT group, and the distribution was similar year by year. The most common causes of end-stage renal disease were glomerular diseases (1,986 cases, 32.4%), followed by diabetes (1,507 cases, 24.6%) and hypertension (932 cases, 15.2%). Although glomerular diseases were the most common cause of end-stage renal disease, diabetes as a cause exhibited an increasing trend, year by year (Fig. 1B). Among the recipients, 5,140 (83.9%) underwent dialysis before kidney transplantation, including 4,411 (72.0%) who underwent hemodialysis and 729 (11.9%) who underwent peritoneal dialysis. Among 3,973 LDKT recipients, 918 (23.1%) underwent preemptive kidney transplantation (Fig. 1C, D). The median duration of dialysis before kidney transplantation was 0.5 years (interquartile range, 0.2–2.0 years) for LDKTs and 6.9 years (interquartile range, 4.2–9.6 years) for DDKTs. At the time of transplantation, 1,911 recipients (31.2%) had diabetes mellitus (31.8% in the LDKT group and 30.0% in the DDKT group), with an increasing trend, year by year. At the time of transplantation, 702 recipients (11.5%) had cardiovascular disease; the proportion was higher in the DDKT group (334, 15.5%) than in LDKT group (368, 9.3%). The baseline and clinical characteristics of kidney-transplant patients are summarized in Table 1.
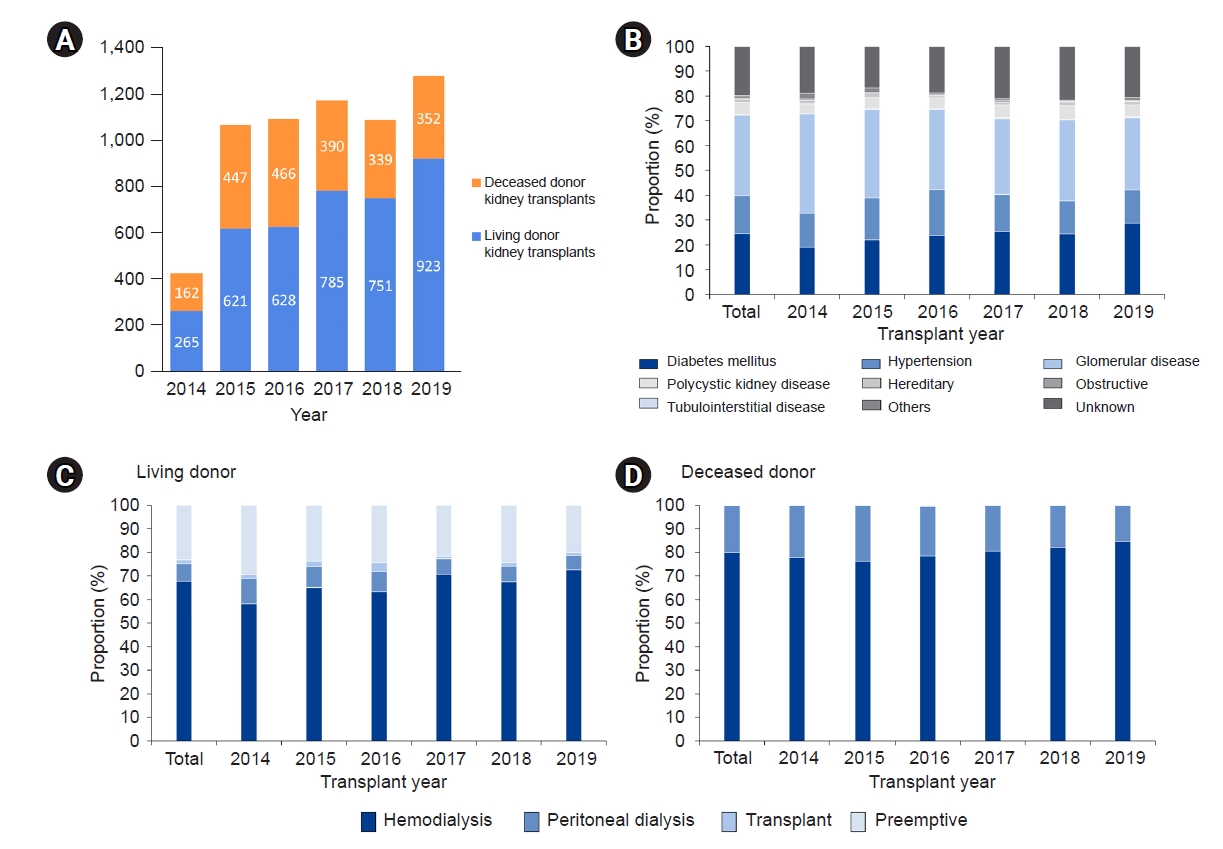
Baseline characteristics of kidney transplants in KOTRY. (A) The numbers of registered living-donor and deceased-donor kidney transplantations in KOTRY from 2014 to 2019. (B) The causes of end-stage renal disease among total kidney recipients. (C, D) Dialysis modality before living-donor and deceased-donor kidney transplantations according to transplantation year.
KOTRY, Korean Organ Transplantation Registry.
Perioperative clinical characteristics of kidney-transplant recipients
A total of 1,469 recipients (24.0%) received desensitization therapy prior to transplantation. The most common reason for desensitization was ABO blood-type incompatibility (1,069 cases, 17.4%), followed by positive human leukocyte antigen (HLA) crossmatch results (434 cases, 7.1%; 129 cases of positive complement–dependent cytotoxicity crossmatch results and 305 cases of positive flow–cytometric crossmatch results) and positive results for donor-specific antibodies (424 cases, 6.9%). Basiliximab was the most commonly used induction agent, and antithymocyte globulin (ATG) induction was used more frequently in the DDKT group than in the LDKT group (p < 0.001). Corticosteroids, tacrolimus, and mycophenolate mofetil were the predominantly used maintenance immunosuppressant. Annual trends in the proportion of ABO- and HLA-incompatible kidney transplantation, complications after kidney transplantation, and usage of maintenance immunosuppressant were represented in Supplementary Fig. 1-3 (available online).
Posttransplant outcomes of registered kidney-transplant recipients
Delayed graft function after kidney transplantation occurred in 10.3% of DDKTs and 0.6% of LDKTs. The mean serum creatinine concentration of the recipients was 1.22 ± 0.55 mg/dL at 1 year after kidney transplantation (1.19 ± 0.52 mg/dL in the LDKT group and 1.27 ± 0.6 mg/dL in the DDKT group, respectively), and the distribution of serum creatinine concentration did not significantly differ year by year. The mean estimated glomerular filtration rate (eGFR) at 1 year after transplantation was 62.9 ± 21.5, 63.4 ± 19.0, and 62.1 ± 25.1 mL/min/1.73 m2 in all kidney transplantations, LDKTs, and DDKTs, respectively.
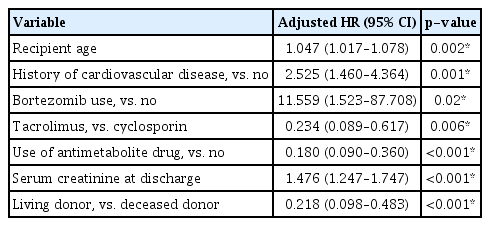
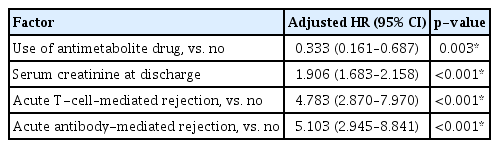
The overall 1-year patient survival rate was 98.4% for all recipients (99.3% in the LDKT group and 97.0% in the DDKT group), and the 3- and 5-year patient survival rates were 97.4% and 95.8% for all recipients (98.7% and 97.8% in the LDKT group and 95.2% and 92.8% in the DDKT group), respectively (Fig. 2A, B). Upon multivariate Cox regression analysis, older recipient age, a history of cardiovascular disease, bortezomib use, cyclosporine rather than tacrolimus use at discharge, no antimetabolite drugs used at discharge, a higher serum creatinine concentration at discharge, and DDKT rather than LDKT were significantly associated with death after kidney transplantation (Table 2). Supplementary Table 1 (available online) presents the causes of patient death, and the most common cause of death was infection, followed by cardiovascular disease and malignancy. The overall 1-year graft survival rate was 97.1% for all recipients (98.4% in the LDKT group and 94.9% in the DDKT group), and the 3- and 5-year graft survival rates were 94.3% and 90.5% for all recipients (96.2% and 93.2% in the LDKT group and 91.3% and 86.1% in the DDKT group), respectively (Fig. 2C, D). No antimetabolite drugs used at discharge, a higher serum creatinine concentration at discharge, and episodes of acute T-cell–mediated or antibody-mediated rejection were significantly associated with graft loss after kidney transplantation upon multivariate Cox regression analysis (Table 3). The 1-year death-censored graft survival rate was 98.5% for all recipients (99.0% in the LDKT group and 97.5% in the DDKT group), and the 3- and 5-year death-censored graft survival rates were 96.5% and 93.6% for all recipients (97.1% and 94.9% in the LDKT group and 95.5% and 91.4% in the DDKT group), respectively.

Patient and graft survival of kidney-transplant recipients in KOTRY. (A, B) Patient survival of kidney recipients. (C, D) Graft survival of kidney recipients.
KOTRY, Korean Organ Transplantation Registry.
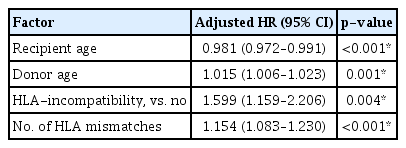
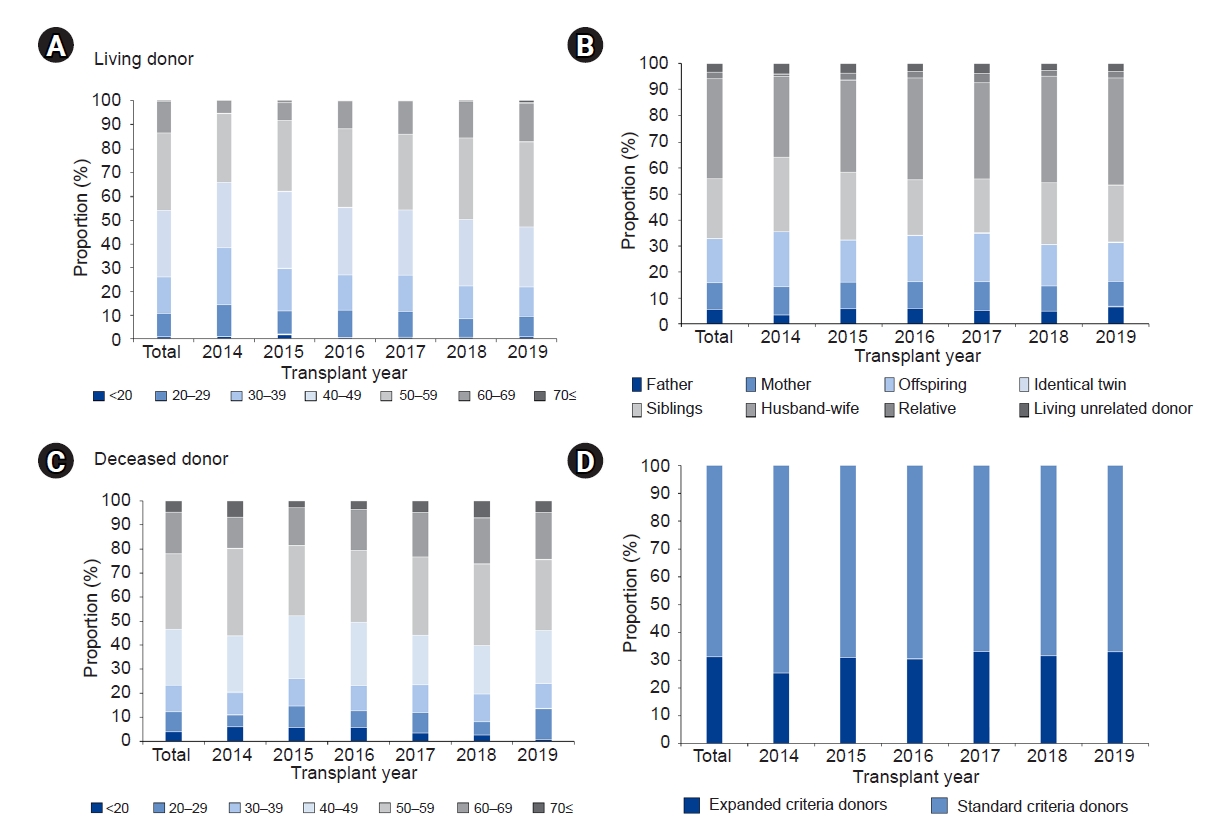
During a mean follow-up period of 3.8 years, biopsy-proven acute rejection episodes were confirmed after kidney transplantation in 17.0% of all recipients (16.1% in the LDKT group and 18.4% in the DDKT group) (Fig. 3A), of which 57 (0.9%) led to graft failures. Upon multivariate Cox regression analysis, younger recipient age, older donor age, HLA-incompatible transplantation, and a higher number of HLA mismatches were significantly associated with rejection after transplantation (Table 4). Cardiac events occurred after transplantation in 4.3% of all recipients (3.2% in the LDKT group and 6.2% in the DDKT group) (Fig. 3B), and NODAT developed in 18.6% of all recipients (19.0% in the LDKT group and 18.1% in the DDKT group) (Fig. 3C). Upon multivariate Cox regression analysis, a history of previous transplantation, diabetes, and a history of cardiovascular disease were significantly associated with cardiac events after transplantation (Table 5), and recipient age and body mass index were significantly associated with NODAT. Malignant tumors were detected after transplantation in 3.8% of all recipients (4.0% in the LDKT group and 3.5% in the DDKT group) (Fig. 3D). A history of tumors and the use of mechanistic target of rapamycin (mTOR) inhibitors, such as sirolimus and everolimus, were significantly associated with malignancy after kidney transplantation upon multivariate Cox regression analysis. The types of malignant tumor and cardiac events are summarized in Supplementary Table 2 (available online); the most common type of malignant tumor was thyroid cancer, followed by kidney cancer, breast cancer, and gastrointestinal cancer. Infection episodes requiring hospitalization were most frequent in the first 6 months after transplantation, and bacterial infection was the most common type of infection, followed by viral infection (Fig. 3E, F). Upon multivariate Cox regression analysis, older donor age, a higher recipient body mass index, ATG rather than basiliximab induction, and transplantation from a deceased donor rather than a living donor were significantly associated with viral infection after transplantation (Table 6), while female recipient sex, HLA- and ABO-incompatible kidney transplantation, a history of cardiovascular disease, and nonuse of antimetabolite drugs were significantly associated with nonviral infection after transplantation (Table 7).
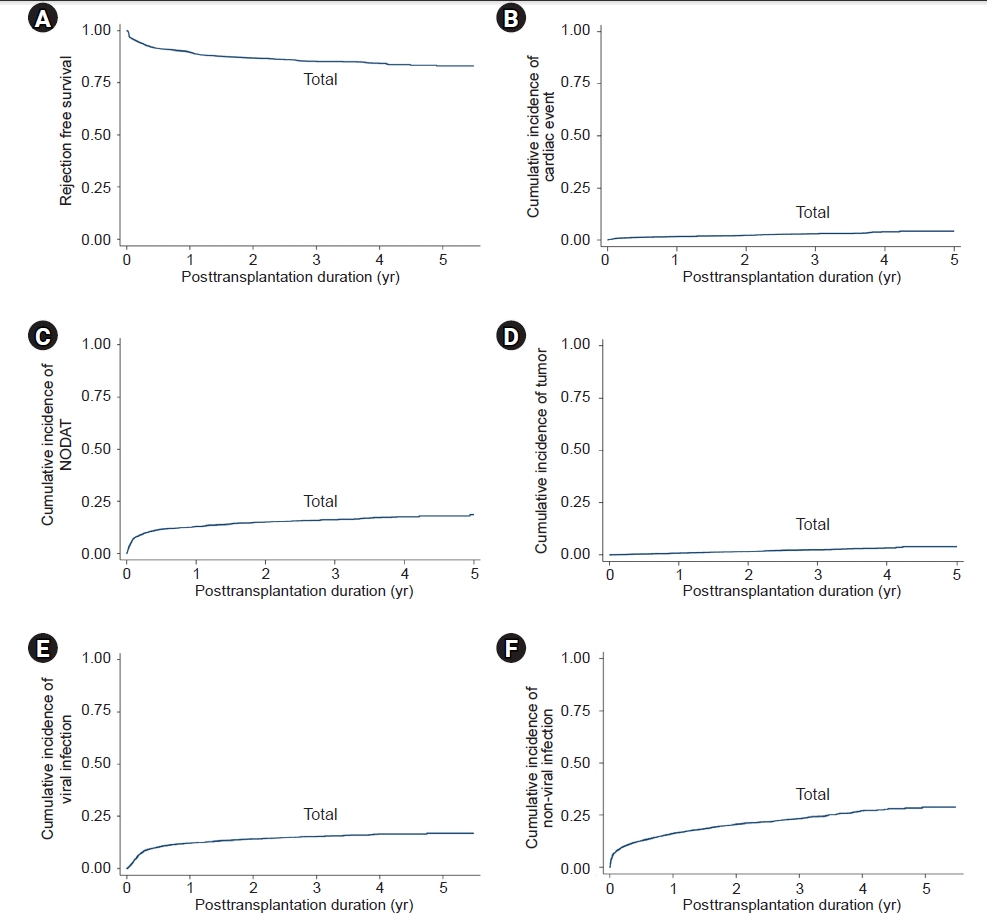
Posttransplant complications and comorbidities of kidney-transplant recipients in KOTRY. (A) Rejection (biopsy-proven)-free survival rate. Cumulative incidence rates of (B) cardiac events after kidney transplantation, (C) NODAT, (D) malignancy after kidney transplantation, (E) viral infection after kidney transplantation, and (F) nonviral infection after kidney transplantation.
KOTRY, Korean Organ Transplantation Registry; NODAT, new-onset diabetes after transplantation.
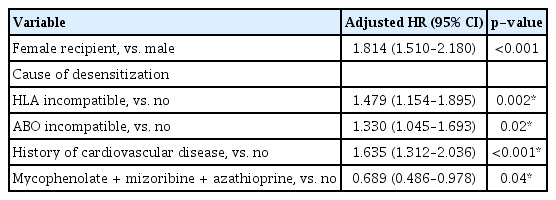
Summary of the registered kidney-transplant donors
The mean age of registered kidney-transplant donors was 47.3 ± 12.9 years, with the largest age group being those in their 50s. The mean ages of living and deceased donors were 46.7 ± 11.8 and 48.5 ± 14.7 years, respectively. The age range of living donors was 19 to 76 years, and that of deceased donors was 0 to 81 years (Fig. 4A, B). Among all registered kidney donors, 3,221 (52.6%) were male and 2,907 (47.4%) were female. The proportion of male donors was 43.4% in LDKTs and 69.4% in DDKTs. In LDKTs, donations from spouses were the most common (1,518 cases, 38.2%), followed by those from siblings (921 cases, 23.2%), offspring (672 cases, 16.9%), parents (629 cases, 15.8%), and unrelated donors (133 cases, 3.3%) (Fig. 4C). The total number of deceased donations was 2,156, of which donation after circulatory death occurred in 78 cases (3.6%), and 31.2% of donors belonged to the expanded-criteria donors (Fig. 4D). At 1 year after kidney donation, there were no mortalities among the 2,140 LDKT donors who were followed up with. The mean serum creatinine concentration of the living donors at baseline was 0.78 ± 0.62 mg/dL (range, 0.09–1.75 mg/dL), and that at 1 year after kidney donation was 1.09 ± 0.24 mg/dL (range, 0.25–1.88 mg/dL). The mean eGFRs at baseline and at 1 year after donation among living kidney donors were 97.6 ± 27.7 and 65.5 ± 13.8 mL/min/1.73 m2, respectively.
Discussion
In this study, we introduced the basic design and current status of the KOTRY, which consists of five organ-transplant cohorts. Furthermore, the baseline characteristics and outcomes of the kidney-transplant cohort in the KOTRY were summarized.
The number of patients with end-stage renal disease in Korea increased to more than 100,000 in 2019, doubling since 2010 [11]. Despite several risks, such as rejection, infection, cardiovascular disease, and malignancy, kidney transplantation remains a preeminent treatment for kidney failure, with the number of kidney-transplant recipients growing continuously [7,8,10,12]. The Korean Network for Organ Sharing (KONOS) was founded in 2000 to manage aspects of organ transplantation nationwide, such as patient registration, approval of living-donor organ transplantation, and allocation of deceased-donor organs to patients on a waiting list. However, the KONOS database does not contain comprehensive posttransplant data, including treatment outcomes and long-term prognoses. For this reason, the Korean Society for Transplantation and the KONOS launched the KOTRY under the sponsorship of the Korea Centers for Disease Control and Prevention Agency in April 2014. The KOTRY consists of five organ-transplant cohorts (kidney, liver, heart, lung, and pancreas), for which baseline and posttransplant data of organ donors and recipients are recorded [9,10]. Annual KOTRY reports have been published every year since 2015, and the input data have proven reliable to date.
Several other countries have similar nationwide, integrated databases for systematic management of the information related to organ transplants and donations. These systems include the Scientific Registry of Transplant Recipients in the United States [13], the Australia and New Zealand Dialysis and Transplant Registry and the Australia and New Zealand Organ Donor Registry [14], the Collaborative Transplant Study [15], the China Liver Transplant Registry [16], the Japan Renal Transplantation Registry [17], the Thai Transplant Registry [5], and others [18–21]. As most transplant centers that conduct kidney transplantation in Korea have been included in the KOTRY and as all large-volume transplant hospitals have joined the KOTRY, the KOTRY has expanded to contain more than half of all kidney-transplant patients registered in the KONOS each year. Therefore, the KOTRY kidney cohort can be considered a nationally representative cohort of Korean kidney transplants. However, cautious interpretation is required because data were collected only from patients who agreed to participate in the KOTRY study. Additionally, KOTRY had an inherent limitation of being a multicenter registry study in terms of inter-center and inter-clinician differences in clinical practice for kidney transplantation.
Despite the relatively short follow-up duration of our report, it identified the independent risk factors for mortality of Korean kidney-transplant patients, including older age, a history of cardiovascular disease, bortezomib use, cyclosporine rather than tacrolimus usage at discharge, no usage of antimetabolite drugs at discharge, a higher serum creatinine concentration at discharge, and DDKT rather than LDKT. Older recipient age, cardiovascular disease, lower graft function, and DDKT are well-known risk factors for patient death in kidney transplant in previous studies [22–24], and Gonzalez-Molina et al. [25] reported that treatment with mycophenolate mofetil and the use of tacrolimus instead of cyclosporine reduced the risk of patient death by 43%. In addition, although there are scarce data of the effect of bortezomib use on mortality in kidney transplantation, several previous studies have reported a higher incidence of adverse events, such as infectious disease, gastrointestinal and hematologic toxicity for bortezomib use in kidney transplantation [26–28]. Independent risk factors for graft loss were as follows: no antimetabolite drugs used at discharge, a higher serum creatinine concentration at discharge, and episodes of acute T-cell–mediated or antibody-mediated rejection. These findings are in parallel with several other studies [23,29–31]. Moreover, age, HLA-incompatible transplantation, and a higher number of HLA mismatches were associated with rejection after transplantation, in agreement with results from previous reports [32–34]. Our study indicated that episodes of viral or nonviral infection requiring hospitalization were associated with older age, deceased rather than living donors, female sex, HLA-incompatible and ABO-incompatible kidney transplantation, and ATG rather than basiliximab induction, in accordance with previous studies [32,33,35–37]. Because a compromised capacity to repair injury in older kidneys could lead to accelerated immune response and acute rejection, the risks of rejection might be higher in older donor kidney transplantation [38]. Older donor age is also associated with the occurrence of delayed graft function and could be a risk factor for viral infection [39]. Interestingly, nonuse of antimetabolite drugs at discharge was associated with nonviral infection after transplantation, which may reflect a discontinuation of antimetabolite drugs because of infection episodes during hospitalization. In addition, the association of usage of mTOR inhibitors with malignancy after kidney transplantation may reflect the tendency for patients with a history of tumors or at high risk of malignancy to be prescribed such treatments [40].
Maintaining the KOTRY will enable the analysis of longer-term outcomes of patients and grafts as well as the identification of prognostic factors for transplantation. Furthermore, KOTRY data may contribute to the scientific progress of organ transplantation worldwide by collaboration with transplant cohort studies in other countries and participation in international comparison studies. In addition, it is expected that these data will provide scientific evidence not only for the development of national policies to improve the availability and efficiency of organ transplantation but also for the research and development of cutting-edge transplantation techniques. In terms of living kidney donors, data about complications and prognosis, including changes in renal function after donation, are being collected in the KOTRY. These data can provide objective information of the postdonation clinical course and assist in the development of future guidelines and decision-making for living-donor selection and management.
The KOTRY, as a systematic and nationwide transplant cohort, can serve as a valuable epidemiological database of Korean kidney transplants. The KOTRY kidney-transplant cohort will provide nationwide, real-world data that can be leveraged to improve kidney transplantation in Korea. We believe that the KOTRY kidney cohort will contribute to improvements in patient and graft survival, enhancement of the quality of life of transplant recipients, and the development of treatment guidelines tailored to the national situation.
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.
Funding
This research was supported by funding (2014-ER6301-00, 2014-ER6301-01, 2014-ER6301-02, 2017-ER6301-00, 2017-ER6301-01, and 2017-ER6301-02) provided by the Research of Korea Centers for Disease Control and Prevention Agency. This study was supported by a new faculty research seed money grant of Yonsei University College of Medicine for 2021 (2021-32-0079).
Authors’ contributions
Conceptualization: MSK, JCJ, CA, JY
Data curation: HJJ, MKJ, DWC, SJNC, MSK, JHR, JCJ, JY
Formal analysis: HJJ, TYK, JHR, JCJ, JY
Investigation: TYK, MKJ, DWC, SJNC, MSK, JHR, CA, JY
Methodology: MSK, JCJ, CA, JY
Writing–original draft: HJJ, JY
Writing–review & editing: All authors
All authors read and approved the final manuscript.
Supplementary Materials
Supplementary data are available at Kidney Research and Clinical Practice online (https://doi.org/10.23876/j.krcp.21.185).
Acknowledgements
The names of the participating hospitals and principal investigators of the KOTRY kidney cohort are as follows: Myoung Soo Kim1, Jaeseok Yang2, Jin Min Kong3, Oh Jung Kwon4, Deok Gie Kim5, Cheol Woong Jung6, Yeong Hoon Kim7, Joong Kyung Kim8, Chan-Duck Kim9, Ji Won Min10, Sung Kwang Park11, Yeon Ho Park12, Jae Berm Park13, Jung Hwan Park14, Jong-Won Park15, Tae Hyun Ban16, Sang Heon Song17, Seung Hwan Song18, Ho Sik Shin19, Chul Woo Yang20, Hye Eun Yoon21, Kang Wook Lee22, Dong Ryeol Lee23, Dong Won Lee24, Jieun Oh25, Sang-Ho Lee26, Su Hyung Lee27, Yu Ho Lee28, Jung Pyo Lee29, Jeong-Hoon Lee30, Jin Seok Jeon31, Heungman Jun32, Kyung Hwan Jeong33, Ku Yong Chung34, Jong Soo Lee35, Man Ki Ju36, Dong-Wan Chae37, Soo Jin Na Choi38, Sung Shin39, Seungyeup Han40, Kyu Ha Huh1.
1Department of Surgery, Yonsei University College of Medicine, Seoul, Republic of Korea
2Department of Surgery, Seoul National University Hospital, Seoul, Republic of Korea
3Department of Nephrology, BHS Hanseo Hospital, Busan, Republic of Korea
4Department of Surgery, Hanyang University College of Medicine, Seoul, Republic of Korea
5Department of Surgery, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Republic of Korea
6Department of Surgery, Korea University Anam Hospital, Seoul, Republic of Korea
7Department of Internal Medicine, Inje University Busan Paik Hospital, Busan, Republic of Korea
8Department of Internal Medicine, Bongseng Memorial Hospital, Busan, Republic of Korea
9Department of Internal Medicine, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Republic of Korea
10Division of Nephrology, Department of Internal Medicine, The Catholic University of Korea, Bucheon St. Mary’s Hospital, Bucheon, Republic of Korea
11Department of Internal Medicine, Chonbuk National University Medical School, Jeonju, Republic of Korea
12Department of Surgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Republic of Korea
13Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
14Department of Nephrology, Konkuk University School of Medicine, Seoul, Republic of Korea
15Department of Nephrology, Yeungnam University Medical Center, Daegu, Republic of Korea
16Division of Nephrology, Department of Internal Medicine, The Catholic University of Korea, Eunpyeong St. Mary’s Hospital, Seoul, Republic of Korea
17Department of Internal Medicine, Pusan National University Hospital, Busan, Republic of Korea
18Department of Surgery, Ewha Womans University Seoul Hospital, Seoul, Republic of Korea
19Division of Nephrology, Department of Internal Medicine, Kosin University College of Medicine, Busan, Republic of Korea
20Division of Nephrology, Department of Internal Medicine, The Catholic University of Korea, Seoul St. Mary’s Hospital, Seoul, Republic of Korea
21Department of Internal Medicine, The Catholic University of Korea, Incheon St. Mary’s Hospital, Incheon, Republic of Korea
22Department of Nephrology, Chungnam National University Hospital, Daejeon, Republic of Korea
23Division of Nephrology, Department of Internal Medicine, Maryknoll Medical Center, Busan, Republic of Korea
24Division of Nephrology, Department of Internal Medicine, Pusan National University School of Medicine, Busan, Republic of Korea
25Department of Internal Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Republic of Korea
26Department of Nephrology, Kyung Hee University Hospital at Gangdong, Seoul, Republic of Korea
27Department of Surgery, Ajou University School of Medicine, Suwon, Republic of Korea
28Division of Nephrology, Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Republic of Korea
29Department of Nephrology, SMG-SNU Boramae Medical Center, Seoul, Republic of Korea
30Department of Surgery, Myongji Hospital, Goyang, Republic of Korea
31Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Seoul, Republic of Korea
32Department of Surgery, Inje University Ilsan Paik Hospital, Goyang, Republic of Korea
33Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Republic of Korea
34Department of Surgery, Ewha Womans University Mokdong Hospital, Seoul, Republic of Korea
35Department of Surgery, Ulsan University Hospital, Ulsan, Republic of Korea
36Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
37Division of Nephrology, Seoul National University Bundang Hospital, Seongnam, Republic of Korea
38Department of Surgery, Chonnam National University Medical School, Gwangju, Republic of Korea
39Department of Surgery, Asan Medical Center, Seoul, Republic of Korea
40Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Republic of Korea