Asymptomatic hematuria in children: Korean Society of Pediatric Nephrology recommendations for diagnosis and management
Article information
Abstract
Hematuria is a relatively common condition among school-aged children. Because international guidelines for asymptomatic hematuria in children are unavailable, developing practical guidelines for the diagnosis and management of asymptomatic hematuria based on scientific evidence while considering real-world practice settings, values, and patient and physician preferences is essential. The Korean Society of Pediatric Nephrology developed clinical guidelines to address key questions regarding the diagnosis and management of asymptomatic hematuria in children.
Introduction
South Korea has implemented mass urine screening for elementary, middle, and high school students since 1998 under the School Health Act. Urinalysis detects occult blood, urine proteins, and urine glucose. Occult blood, indicating possible hematuria, is the most common reason for pediatric visits to doctors. Hematuria is the presence of blood in the urine, defined as five or more red blood cells (RBCs) per high power field (HPF) of view (×400) [1,2]. Even if the urine is red in color or the urine dipstick detects urinary occult blood, the urine may not contain RBCs; therefore, a microscopic examination is required to confirm hematuria. If the color of the urine appears red or dark due to hematuria, it is called gross hematuria, and if the color of the urine does not change but hematuria is visible under a microscope, it is called microscopic hematuria. In general, hematuria has clinical significance when hematuria persists on three or more urine microscopic examinations 2 weeks apart (persistent hematuria). When microscopic hematuria is not accompanied by proteinuria (defined as a single voided urine protein-creatinine ratio greater than 0.2 for patients aged 2 years or older and 0.5 for those under 2 years), it is called isolated microscopic hematuria [1]. Hematuria is a relatively common condition found in 0.2% to 6.0% of school-aged children [3]. Asymptomatic persistent hematuria in children should be differentiated through careful history-taking, including medical and family history; physical examination, including blood pressure measurement and growth assessment; blood and urine tests; and imaging studies, such as kidney and bladder ultrasound, if indicated. Children with abnormalities in this initial assessment should be referred to a pediatric nephrologist or urologist for further evaluation, and follow-up is recommended, even for children without obvious abnormalities [4,5] (Fig. 1).

Initial diagnostic process for children with persistent asymptomatic hematuria.
ANA, antinuclear antibodies; ANCA, anti-neutrophil cytoplasmic antibody; anti-dsDNA, anti-double-stranded DNA; BUN, blood urea nitrogen; HBV, hepatitis B virus.
Owing to the lack of practical guidelines for asymptomatic hematuria in children, the Korean Society of Pediatric Nephrology (KSPN) convened a multidisciplinary guideline development committee consisting of pediatric nephrologists, pediatric urologists, and methodology experts with a genuine interest in hematuria. Therefore, this recommendation is intended primarily for undiagnosed patients under 18 years of age for whom the cause of asymptomatic hematuria is currently being determined or for whom no cause has been found after differential diagnosis, and to help clinicians involved in the diagnosis and management of asymptomatic hematuria make evidence-based clinical decisions. The key questions were selected by reviewing existing guidelines, selecting clinical issues, reviewing evidence, and discussing each topic in the development committee. The GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) methodology was used to assess the level of evidence. Recommendations were provided by reviewing the latest evidence on key questions regarding the diagnosis, treatment, and follow-up of asymptomatic hematuria in children.
Methods
These guidelines were developed based on an adaptation of existing guidelines. For adaptive development, we used existing guidelines as the most important source of evidence, added the latest research results, and modified them to adapt to the healthcare situation in Korea. In addition, the “de novo” method was selectively reviewed when recommendations could not be found in existing guidelines. However, of the eight key questions selected, only two had existing guidelines that fit the target population; therefore, we applied a new creation method. Considering the expertise, representativeness, and continuity of practice guideline development, the KSPN established a practice guideline development committee. The guideline development committee organized a development working group and review committee consisting of pediatric nephrologists, pediatric urologists, and methodology experts. Conflict of interest disclosures were collected from all members of the guideline development committee prior to their participation in guideline development to identify financial and nonfinancial conflicts of interest. Details of the guideline development process are summarized in the Supplementary Materials (available online).
Key questions and recommendations
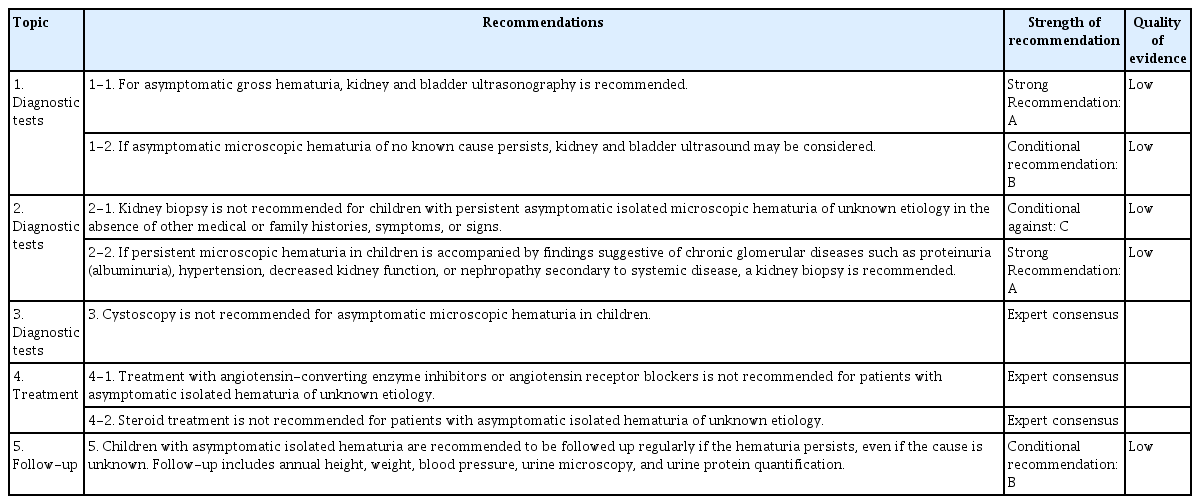
All key questions and recommendations regarding the diagnosis, treatment, and follow-up of asymptomatic hematuria in children are summarized in Table 1, and details of the evidence supporting each recommendation are described below.
Key question 1: What imaging tests should be performed to diagnose the cause of asymptomatic hematuria?
Background
International guidelines recommend kidney and bladder ultrasound for pediatric patients with microscopic hematuria and proteinuria, asymptomatic gross hematuria, or suspected nephrolithiasis. Guidelines state that if microscopic hematuria persists without a clear cause, kidney and bladder ultrasound may be considered [6,7]. Although, ultrasound is frequently performed in clinical practice for children with asymptomatic hematuria, its limitations—sensitivity and specificity can vary depending on the operator—have prompted debate regarding whether computed tomography (CT) should be performed. Because guidelines on the effectiveness of imaging modalities for asymptomatic hematuria in children are lacking, this Population, Intervention, Comparison, and Outcome (PICO) question was intended to initiate a review of the effectiveness or risk of CT compared with ultrasound in children with asymptomatic hematuria.
Recommendations
1-1. For asymptomatic gross hematuria, kidney and bladder ultrasonography is recommended.
(Level of evidence: Low, Recommendation grade: A, strong recommendation)
1-2. If asymptomatic microscopic hematuria of no known cause persists, kidney and bladder ultrasound may be considered.
(Level of evidence: Low, Recommendation grade: B, conditional recommendation)
Summary of evidence
Imaging could detect conditions including nephrolithiasis, congenital anomalies of the kidney and urinary tract, cystic kidney disease, kidney and bladder tumors, and nutcracker syndrome in children with asymptomatic hematuria. Ultrasound is recommended as the first imaging test when nephrolithiasis is clinically suspected [6,7]. However, ultrasonography has a sensitivity of 67% to 83% and a specificity of 78% to 97% in the diagnosis of nephrolithiasis, which is less accurate than CT, which has a sensitivity and specificity of >90%. Therefore, for diagnosing nephrolithiasis, non-contrast CT should be recommended in the presence of painful gross hematuria [8–11]. In contrast, congenital anomalies of the kidney and urinary tract, cystic kidney disease, and tumors of the kidneys and bladder are commonly detected by ultrasound. Doppler ultrasonography is recommended as the first imaging test when nutcracker syndrome is suspected [12]. One systematic review analyzed 736 patients with nutcracker syndrome and recommended ultrasound as an effective diagnostic imaging test, as 79% of patients were diagnosed using ultrasound [13]. The 2018 American College of Radiology (ACR) guidelines recommended that children with gross hematuria be evaluated with ultrasound first and that ultrasound may also be considered if microscopic hematuria without proteinuria persists without an identified cause [14]. Ultrasound can be performed in pediatric patients with hematuria when the above conditions are suspected; however, owing to the low likelihood of disease detection, ultrasound is not recommended in all cases of asymptomatic microscopic hematuria. Contrast CT may be considered if a tumor is diagnosed by ultrasound or if there is recurrent gross hematuria in the absence of abnormalities on kidney and bladder ultrasound. Non-contrast CT may be considered if nephrolithiasis is suspected. Ultrasonography is preferred over CT in pediatric patients with hematuria because of the risk of radiation exposure associated with CT. The ACR estimates that the effective dose of radiation with CT is 3 to 10 mSv, which is in the fourth of five of relative radiation level (annual dose limit of 1 mSv for the general population; the dose of 0.1–0.3 mSv per chest radiography) [6,11,14,15].
Key question 2: Should a kidney biopsy be performed if asymptomatic microscopic hematuria persists?
Background
International guidelines recommend kidney biopsy in the presence of glomerular hematuria or proteinuria. However, whether kidney biopsy should be performed in children with asymptomatic isolated microscopic hematuria is unclear [16]. This PICO question is intended to initiate a review of whether or not performing a kidney biopsy affects kidney outcomes in children with asymptomatic isolated microscopic hematuria.
Recommendations
2-1. Kidney biopsy is not recommended for children with persistent asymptomatic isolated microscopic hematuria of unknown etiology in the absence of other medical or family histories, symptoms, or signs.
(Level of evidence: Low, Recommendation grade: C, conditional against)
2-2. If persistent microscopic hematuria in children is accompanied by findings suggestive of chronic glomerular diseases such as proteinuria (albuminuria), hypertension, decreased kidney function, or nephropathy secondary to systemic disease, a kidney biopsy is recommended.
(Level of evidence: Low, Recommendation grade: A, strong recommendation)
Summary of evidence
Acute and chronic glomerulonephritis can be differentiated from persistent asymptomatic microscopic hematuria in children by a kidney biopsy. Nine studies have reported the results of kidney biopsies in patients with asymptomatic microscopic hematuria, including children [17–25]. The indications for kidney biopsy were hematuria lasting more than 6 months to 2 years, a family history of kidney disease, decreased serum complement, the presence of autoimmune antibodies, combined proteinuria, and gross hematuria. In 47% to 60% of patients with asymptomatic microscopic hematuria without proteinuria, the results of kidney biopsies were normal, and the diagnosed glomerular diseases included thin basement membrane disease (TBMD) (22%–59%), immunoglobulin A nephropathy (IgAN) (6%–50%), complement 3 glomerulonephritis (one case), and Alport syndrome (6%–22%) [18–26]. TBMD has recently been classified as autosomal dominant Alport syndrome; therefore, Alport syndrome and IgAN should be considered when deciding whether a kidney biopsy should be performed in an asymptomatic patient with microscopic hematuria [25,27].
Alport syndrome is treated with angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARB). Treatment is initiated immediately after diagnosis in patients with male X-linked or autosomal recessive Alport syndrome and when albuminuria, defined as a urine microalbumin-creatinine ratio greater than 30 mg/g, is observed in patients with female X-linked or autosomal dominant Alport syndrome. Clinical practice recommendations for the diagnosis and treatment of Alport syndrome, published in Pediatric Nephrology in 2021 [26], recommend diagnosis by kidney biopsy or genetic testing to determine early treatment if glomerular hematuria persists for >6 months [15,25]. However, except in cases of pre-diagnosed Alport syndrome, treatment is usually initiated when albuminuria is present; hence, performing a diagnostic test is never considered late (kidney biopsy or genetic test) when albuminuria occurs. Furthermore, genetic testing is more sensitive and specific than kidney biopsies for the diagnosis of Alport syndrome in recent years. Therefore, genetic testing should be performed first, if possible.
In contrast, IgAN is treated with ACEi or ARB, and, if necessary, with immunosuppressive agents. Japanese clinical practice guidelines for IgAN state that in cases of hematuria without proteinuria or with trace proteinuria, kidney biopsy is optional, as the results of kidney biopsy rarely change the treatment plan but may be necessary for differentiation from Alport syndrome [28,29]. Therefore, biopsies are not always recommended for the differential diagnosis of IgAN in patients with asymptomatic isolated hematuria.
In conclusion, kidney biopsy is not recommended in the absence of findings suggestive of chronic glomerular disease in children with asymptomatic isolated microscopic hematuria. However, if there are findings suggestive of glomerular disease such as proteinuria (albuminuria), high blood pressure (defined as blood pressure above the 95th percentile for age and height for both boys and girls under the age of 13 years, or ≥130/80 mmHg for those 13 years and older), decreased kidney function, or nephropathy secondary to systemic disease, a kidney biopsy is necessary for an accurate diagnosis [30]. However, if a genetic disorder such as Alport syndrome is suspected, genetic testing may be performed first. Conservative treatment may be prioritized if there is a possibility of spontaneously resolving kidney disease, such as postinfectious glomerulonephritis.
Key question 3: Should cystoscopy be performed if asymptomatic hematuria persists?
Background
Current guidelines regarding microscopic hematuria in adult patients recommend that clinicians consider cystoscopy in patients with microscopic hematuria who are at low risk for genitourinary malignancies [31]. The usefulness of cystoscopy for identifying the cause of asymptomatic hematuria in children is unknown, with no current guidelines or recommendations. This PICO question was intended to examine whether or not performing cystoscopy in children with asymptomatic isolated microscopic hematuria causes differences in kidney outcomes.
Recommendations
3. Cystoscopy is not recommended for asymptomatic microscopic hematuria in children.
(Recommendation grade: Expert consensus)
Summary of evidence
Conditions that can be diagnosed using cystoscopy in patients with hematuria include inflammation, masses, stones, foreign bodies in the bladder and urethra, urethral strictures, urethral valves, and nutcracker syndrome [32]. A cystoscope allows doctors to look directly into the bladder and urethra to observe their structure and function, the condition of the mucous membranes, and the presence of tumors, stones, and foreign bodies. In cases of persistent gross hematuria of the bladder or urethra, cystoscopy can help identify the source of bleeding. Although cystoscopy can be used to check for inflammation of the bladder or urethral mucosa during urinary tract infections; however, it is not recommended owing to the risk of exacerbation of the inflammation. The openings of the ureteral orifice can be observed during cystoscopy, which also helps to identify the shape and number of ureteral orifices as well as how urine travels from the kidneys to the bladder. Hematuria through the ureteral orifice is present in the absence of lesions within the bladder and urethra, suggesting hematuria of the kidney and upper urinary tract origin. Cystoscopy may reveal hematuria coming through the left ureteral orifice in nutcracker syndrome [32].
To our knowledge, studies on cystoscopy in asymptomatic microscopic hematuria in children are lacking, and in a study of 136 patients with gross hematuria for whom cystoscopy was performed, no abnormalities were observed in 44% of the patients. Of the remaining patients with abnormalities, inflammatory findings in the bladder and urethra, posterior urethral valve, urethral stricture, and bladder mass were observed in 50, 10, 6, and four patients, respectively [33]. Moreover, the four malignancies identified using cystoscopy were also detected using ultrasound, and the authors noted that cystoscopy is not generally necessary to differentiate them; however, patients with persistent hematuria with no abnormalities detected by imaging studies may be considered for cystoscopy. Because cystoscopy is used in patients with asymptomatic hematuria to differentiate malignancy, and malignancies of the bladder are extremely rare in children [34], cystoscopy should be limited to patients with unremarkable imaging results but persistent gross hematuria at the discretion of the urologist.
Key question 4: Do patients with asymptomatic isolated hematuria of unknown etiology require medications such as angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or steroids?
Background
The effectiveness of the medications frequently prescribed to treat glomerular disorders in children with asymptomatic hematuria is uncertain. No studies have investigated how the use of ACEi, ARB, or steroids in children with asymptomatic isolated hematuria of unknown cause affects kidney function. Therefore, the authors reviewed studies that investigated the causes of hematuria in children with asymptomatic isolated microscopic or gross hematuria and sought to determine the proportion of causal conditions that required treatment with medications such as ACEi, ARB, or steroids. This PICO question is intended to determine whether or not the administration of ACEi, ARB, or steroids affects kidney outcomes in children with asymptomatic isolated microscopic hematuria.
Recommendations
4-1. Treatment with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers is not recommended for patients with asymptomatic isolated hematuria of unknown etiology.
(Recommendation grade: Expert consensus)
4-2. Steroid treatment is not recommended for patients with asymptomatic isolated hematuria of unknown etiology.
(Recommendation grade: Expert consensus)
Summary of evidence
A systematic review of 857 children with asymptomatic isolated microscopic hematuria found no cause of hematuria in 57.6% of all patients, with the remainder attributed to Alport syndrome/TBMD (15.7%), IgAN (10.4%), hypercalciuria or nephrolithiasis (9.4%), or other causes (<3%) [35]. A study of 228 children with asymptomatic isolated gross hematuria found that the cause of hematuria could not be identified in 37.7% of cases. The confirmed causes included hypercalciuria or nephrolithiasis in 24.1%, IgAN in 15.8%, post-streptococcal glomerulonephritis in 9.2%, exercise-induced hematuria in 3.2%, and Alport syndrome/TBMD in 2.6% [26]. In these studies, IgAN and Alport syndrome/TBMD, both of which can or should be treated with medications, account for up to 16% of all cases of asymptomatic isolated hematuria.
The administration of ACEi and ARB can be beneficial for IgAN. The 2021 KDIGO (Kidney Disease: Improving Global Outcomes) recommendations suggest treatment with ACEi or ARB for all children with IgAN with proteinuria [16]. However, the Japanese Society of Nephrology’s 2020 clinical practice guidelines for IgAN recommends that in patients with proteinuria of less than 0.5 g/day, existing evidence to evaluate the effectiveness of ACEi or ARB is lacking. Therefore, medications should be prescribed based on pathologic findings, age, degree of hematuria, and the presence of hypertension [28]. In contrast, in IgAN, steroid treatment is reserved only for patients with proteinuria of greater than 1 g/day or mesangial hypercellularity [16]. We found no randomized controlled trials or clinical practice guidelines on the usefulness of steroid treatment for IgAN without proteinuria.
The 2020 practice guidelines for Alport syndrome recommend treatment in the presence of albuminuria in autosomal dominant Alport syndrome and female X-linked Alport syndrome, which are the most common forms [26]. In autosomal dominant Alport syndrome and female X-linked Alport syndrome, the efficacy of ACEi and ARB blockers before albuminuria develops is unknown. However, in male patients with X-linked and autosomal recessive Alport syndromes, treatment with ACEi or ARB is recommended even before proteinuria occurs.
Therefore, owing to the lack of evidence, treatment with ACEi or ARB for patients with asymptomatic isolated hematuria of unknown etiology is not recommended. In addition, the indication for steroid use is the development of severe proteinuria in patients with glomerulonephritis. Given the high incidence of side effects (stunted growth, overweight, hypertension, fractures, and elevated blood sugar) caused by steroid use, steroid therapy is not recommended for patients with asymptomatic isolated hematuria without a diagnosis of glomerular disease.
Key question 5: If asymptomatic isolated hematuria persists, should the patient be followed up regularly?
Background
International guidelines for follow-up plan for children with asymptomatic microscopic hematuria are unavailable. Japanese clinical practice guidelines recommend urinalysis four times in the first year, once or twice annually thereafter, and blood tests annually in children with asymptomatic hematuria of unknown etiology; however, they do not provide a clear rationale for this recommendation [36]. This PICO question was intended to examine whether regular follow-ups had an impact on kidney outcomes in children with asymptomatic isolated microscopic hematuria.
Recommendations
5. Children with persistent asymptomatic hematuria are recommended to be followed up regularly if the hematuria persists, even if the cause is unknown. Follow-up includes annual height, weight, blood pressure, urine microscopy, and urine protein quantification.
(Level of evidence: Low, Recommendation grade: B, conditional recommendation)
Summary of evidence
Although the long-term prognosis of children with asymptomatic hematuria is generally considered good [5], a literature search could not identify any randomized controlled trials or prospective observational studies of hematuria and long-term kidney outcomes in children. In a nationwide retrospective cohort study in Israel on the incidence of end-stage kidney disease (ESKD) in patients with persistent asymptomatic hematuria starting in adolescence at the age of 16 to 17 years with a mean follow-up of 22 years. The absolute risk of ESKD in the cohort was only 27.6 people per 100,000 (0.28%); however, the relative risk of developing ESKD was 17.9 times higher than in those without hematuria [37]. In addition, a Hungarian study followed 341 patients with persistent hematuria for at least 6 months and reported that 47 patients (13.8%) developed symptoms suggestive of glomerular disease and underwent kidney biopsy; 10.5% of the total patients showed a decrease in estimated glomerular filtration rate to 75 mL/min/1.73 m2 or less, with a mortality rate of 0.58% [19]. A Chinese study followed patients with asymptomatic isolated hematuria for 2 to 10 years and found that 6% (13 of 215) had concomitant proteinuria, hypertension, and kidney damage [38]. In addition, a Taiwanese study, which has been implementing school urine screening since 1990, reported that before school urine screening, 100% of rapidly progressive glomerulonephritis and approximately 50% of focal segmental glomerulosclerosis cases progressed to chronic kidney disease; however, after-school urine screening was started, 28.5% of rapidly progressive glomerulonephritis cases were detected early and the patients maintained kidney function, and only 5% of focal segmental glomerulosclerosis progressed to ESKD within 10 years [20]. In a Korean study, kidney biopsies from 149 pediatric patients with persistent microscopic hematuria revealed histological abnormalities in 139 patients (93.3%), including TBMD, IgAN, IgA vasculitis, and Alport syndrome [39]. Therefore, even if the cause of hematuria is not identified during the initial diagnosis, if hematuria persists without resolution, chronic glomerular disease may be present, and symptoms such as proteinuria, high blood pressure, decreased kidney function, and growth retardation may appear later. Accordingly, regular follow-up is necessary for the development of new clinical symptoms.
Studies on the long-term kidney prognosis of hematuria have mostly focused on adults, and hematuria is a risk factor for ESKD and mortality in adults. In Japan, where urine test abnormalities are screened through national health screening, a study of more than 100,000 people in the general population reported that adult men with hematuria had a 1.4-fold increased risk of mortality and a 2.3-fold increased risk of ESKD [40,41]. While examining the association between hematuria and ESKD in adult patients with glomerulonephritis, mild to moderate hematuria (1–29 RBC/HPF) was a risk factor for ESKD in patients with IgAN, even after adjusting for other clinical and pathological factors [37], and hematuria was identified as a risk factor for mortality in advanced chronic kidney disease (stages 3–5) [42]. Therefore, this recommendation suggests annual height, weight, and blood pressure measurements, urine microscopy, and quantitative urine protein, including albumin, using urine samples taken immediately after waking up.
Conclusions
This guideline was developed to provide directions for all frontline healthcare providers and stakeholders for diagnosing and managing children with asymptomatic hematuria. The guidelines provide eight recommendations for the diagnosis, treatment, and follow-up of patients with asymptomatic hematuria. However, all recommendations have a low level of evidence for certainty. We identified the need for well-designed and rigorous randomized controlled trials of asymptomatic hematuria in children.
Supplementary Materials
Supplementary data are available at Kidney Research and Clinical Practice online (https://doi.org/10.23876/j-krcp-23-231).
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.
Data sharing statement
The data presented in this study are available upon reasonable request from the corresponding author.
Authors’ contributions
Conceptualization, Data curation, Investigation: All authors
Supervision: HGK, JSS
Writing–original draft: EP
Writing–review & editing: EP
All authors read and approved to the final manuscript.
Acknowledgements
This guideline for asymptomatic hematuria in children was developed with the support of the Korean Society of Pediatric Nephrology.