Diastolic dysfunction and acute kidney injury in elderly patients with femoral neck fracture
Article information
Abstract
Background
Femoral neck fracture is common in the elderly population. Acute kidney injury (AKI) is an important risk factor for mortality in patients who have had such fracture. We evaluated the incidence of AKI in patients who had femoral neck fracture and identified risk factors for AKI and mortality.
Methods
This was an observational cohort study including 285 patients who were ≥ 65 years of age and who underwent femoral neck fracture surgery between 2013 and 2017.
Results
The mean age was 78.63 ± 6.75 years. A total of 67 (23.5%) patients developed AKI during the hospital stay: 57 (85.1%), 5 (7.5%), and 5 (7.5%) patients were classified as having stage 1, 2, and 3 AKI, respectively. Patients with AKI had a lower baseline estimated glomerular filtration rate and higher left atrial dimension, left ventricular mass index, pulmonary artery pressure, and the ratio of early mitral inflow velocity to early diastolic mitral annulus velocity (E/e’) and were more likely to have diabetes or hypertension (HTN) (P < 0.05). The presence of HTN (odds ratio [OR], 4.570; 95% confidence interval [CI], 1.632–12.797) higher E/e’ (OR, 1.105; 95% CI, 1.019–1.198), and lower hemoglobin (OR, 0.704; 95% CI, 0.528–0.938) were independently associated with a higher risk for developing AKI. Severe AKI (OR, 24.743; 95% CI, 2.822–212.401) was associated with a higher risk of mortality.
Conclusion
Elderly patients with femoral neck fracture had a high incidence of AKI. Diastolic dysfunction was associated with AKI. Severe AKI was associated with in-hospital mortality.
Introduction
Femoral neck fracture is common in the elderly population. A previous study anticipated that the number of hip fractures occurring worldwide will increase from 1.66 million in 1990 to 6.26 million by 2050 [1]. Elderly patients who have had femoral neck fracture have a lower quality of life and increased morbidity and mortality [2,3]. Acute kidney injury (AKI) is one of the most common complications after surgery, and it is associated with increased hospital costs and mortality [4–6].
The aging kidney shows several structural and functional changes similar to those seen with chronic kidney disease (CKD). Structural changes include arteriosclerosis, glomerulosclerosis, tubular atrophy, and fibrosis. Functional changes include decreased glomerular filtration rate, altered renal sensitivity to vasoconstrictors and vasodilators, and lowered auto-regulatory capacity [7,8]. In addition, the elderly population has shown a higher prevalence of left hypertrophy and left ventricular (LV) diastolic dysfunction compared with a younger population [9,10]. Although elderly patients have a high risk of perioperative morbidity, few studies have evaluated orthopedic surgery including femoral fracture in the elderly population.
We evaluated the incidence of AKI along with not only the previously known risk factors, but also echocardiographic findings including peak early trans-mitral flow velocity (E) and early diastolic mitral annular velocity (e’) ratio (E/e’ ratio). The E/e’ ratio indicates the diastolic function that correlates with LV filling pressure. Furthermore, we evaluated the association between AKI and inhospital mortality, and identified risk factors for the development of in-hospital mortality.
Methods
Patients
This was a single-center, retrospective cohort study that included 285 patients who were older than 65 years of age and had undergone femoral neck fracture surgery in Korea University Anam Hospital from January 2013 to June 2017. Among 313 patients who had undergone femoral neck fracture surgery, we excluded 20 patients who did not have follow-up creatinine data and 8 patients who had undergone renal replacement therapy. Demographic and laboratory data were collected from electronic medical records.
The glomerular filtration rate was estimated by the Modification of Diet in Renal Disease Study equation [11]. CKD was defined by baseline estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2. The eGFR at admission was defined as the first eGFR after the admission date. Left atrial (LA) dimension, LV mass index, E/A ratio, deceleration time, ejection fraction (EF), E/e’, and pulmonary artery (PA) pressure were estimated by echocardiography including tissue Doppler imaging conducted within 6 months prior to surgery. Heart failure with reduced EF (HFrEF) was defined as an EF consistently below 40%. Coronary artery disease (CAD) was defined as a history of myocardial infarction, angina, percutaneous coronary intervention, or coronary artery stenosis of more than 50% of the diameter as documented by coronary angiography. Cerebrovascular accident (CVA) was defined as stroke or transient ischemic accident. The use of nonsteroidal anti-inflammatory drugs, starch, angiotensin-converting-enzyme inhibitor (ACEI)/angiotensin II receptor blocker (ARB), and diuretics was evaluated during one week after the femur neck surgery. The administration of contrast was evaluated within a week before and after the surgery. Transfusion was defined as the administration of blood product within one week after surgery. The incidence of gastrointestinal bleeding, septic shock, mechanical ventilation, cardiac event, and pneumonia was evaluated during admission period after the surgery. A cardiac event was defined by the incidence of angina, myocardial infarction, and aggravation of heart failure during the admission period after the surgery. This study was reviewed and approved by the Institutional Review Board of the Korea University Anam Hospital (IRB number: 2018AN0222). This study was conducted in accordance with the Declaration of Helsinki.
Outcomes
AKI was defined by the Kidney Disease Improving Global Outcomes criteria as an increase in serum creatinine of more than 0.3 mg/dL within 48 hours or an increase in serum creatinine of more than 1.5 times baseline within a week [12]. Baseline creatinine value was defined as the creatinine value measured 7 to 365 days before hospitalization [13]. For patients who did not have pre-admission creatinine data, the lowest creatinine concentration during hospitalization was defined as the baseline creatinine [14]. Urine output criteria were not included. AKI was classified into stages 1, 2, and 3: stage 1 was defined as serum creatinine 1.5 to 1.9 times the baseline or a ≥ 0.3 mg/ dL increase; stage 2 as serum creatinine 2.0 to 2.9 times the baseline; and stage 3 as serum creatinine 3.0 times the baseline, an increase to ≥ 4.0 mg/dL, or initiation of renal replacement therapy [12]. Severe AKI was defined as AKI stage 2 or 3. In-hospital mortality was defined as death occurring during the initial hospitalization.
Statistical analysis
Data were analyzed using IBM SPSS Statistics (version 24.0; IBM Corp., Armonk, NY, USA). Continuous variables are presented as means ± standard deviations, and not equally distributed data were presented as medians and interquartile ranges. Comparisons were made using a Student’s t test for normally distributed data and a Mann–Whitney U test for not normally distributed data. Categorical variables are presented as proportions and were compared with a chi-square test. A two-tailed P value of < 0.05 was considered significant. To identify the risk factors for the development of AKI and to identify factors for in-hospital mortality, we initially conducted a univariate logistic regression analysis. Variables that were statistically significant (P < 0.1) in this analysis were then included in a multivariate logistic regression analysis. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated.
Results
Baseline characteristics
The baseline characteristics of the study patients are shown in Table 1. The mean age of the overall population was 78.63 ± 6.75 years and 80.00 ± 6.68 vs. 78.21 ± 6.74 for the AKI and non-AKI groups, respectively, and 75.4% were women. Patients who developed AKI had a higher prevalence of diabetes mellitus (DM) (44.8% vs. 28.0%, P = 0.010) and hypertension (HTN) (79.1% vs. 56.2%, P = 0.001). They also had a lower eGFR at baseline (86.55 ± 32.47 vs. 100.67 ± 37.60, P = 0.006) and admission (63.71 ± 22.82 vs. 79.42 ± 24.87, P < 0.001). There was no significant difference between groups in regard to age, sex, blood pressure, body mass index, hemoglobin, erythrocyte sedimentation rate (ESR), C-reactive protein, liver function test, albumin, CKD, CAD, chronic obstructive pulmonary disease, CVA, proteinuria, and hematuria. The length of hospital stay was similar between groups.
The type of femoral neck surgery was evaluated: 66.0% of patients underwent bipolar hemiarthroplasty, 16.8% was total hip replacement arthroplasty, 6.7% was intramedullary nailing, and 10.5% was screw fixation. The type of surgery was not different between the AKI and non-AKI group. In patients with AKI, the post-operative use of ACEI/ARB and diuretics was significantly higher than non-AKI patients (P = 0.015). Transfusion was more common in patients with AKI, and the higher transfusion volume was administered in AKI patients (P = 0.009) (Table 1).
Echocardiographic measurements of study patients
In patients with AKI, the preoperative measurement of LA dimension (37.1 ± 7.0 vs. 34.5 ± 7.2, P = 0.017), LV mass index (96.2 ± 26.5 vs. 86.0 ± 22.1, P = 0.006), and PA pressure (42.7 ± 10.7 vs. 39.1 ± 9.1, P = 0.027) were significantly higher than non-AKI patients (P < 0.05). In addition, LV filling pressure measured by E/e’ ratio was significantly higher in patients with AKI (14.5 ± 5.8 vs. 11.6 ± 4.2, P < 0.001). However, EF, the presence of HFrEF, and the presence of valvular disease were not different between AKI and non-AKI patients (Table 2).
The incidence and risk factors of AKI in elderly patients with femoral neck fracture
Among 285 patients who underwent femoral neck fracture surgery, 67 (23.5%) developed AKI postoperatively during their initial hospitalization: 57 (85.1%), 5 (7.5%), and 5 (7.5%) patients were classified as having AKI stage 1, 2 and 3, respectively. None required renal replacement therapy.
We analyzed factors associated with AKI stages 1 to 3. In the univariate logistic analysis, baseline eGFR (OR, 0.988; 95% CI, 0.980–0.997), E/e’ ratio (OR, 1.128; 95% CI, 1.057–1.203), higher LV mass index (OR, 1.018; 95% CI, 1.006–1.030), higher LA dimension (OR, 1.051; 95% CI, 1.007–1.097), higher PA pressure (OR, 1.038; 95% CI, 1.004–1.073), DM (OR, 2.087; 95% CI, 1.186–3.672), HTN (OR, 2.948; 95% CI, 1.543–5.631), use of ACEI/ARB, diuretics, and transfusion were significantly associated with AKI (P < 0.05). The presence of chronic obstructive pulmonary disease (OR, 9.571; 95% CI, 1.711–53.539), lower albumin (OR, 0.293; 95% CI, 0.090–0.959), higher LV mass index (OR, 1.032; 95% CI, 1.009–1.055), and lower EF (OR, 0.900; 95% CI, 0.832–0.973) were significantly associated with severe AKI.
The multivariate analysis revealed that the presence of HTN (OR, 4.570; 95% CI, 1.632–12.797), higher E/e’ ratio (OR, 1.105; 95% CI, 1.019–1.198), and lower hemoglobin (OR, 0.704; 95% CI, 0.528–0.938) were independently associated with a higher risk for development of AKI (Table 3). In addition, higher mean blood pressure (MBP) (OR, 1.064; 95% CI, 1.006–1.125), higher ESR (OR, 1.047; 95% CI, 1.011–1.083), and lower EF (OR, 0.854; 95% CI, 0.753–0.969) were associated with an increased risk for the development of severe AKI.
Risk factors predicting in-hospital mortality
Six patients died during hospitalization: 3 (4.5%) in the AKI group and 3 (1.4%) in the non-AKI group. In the AKI group, 2 (3.0%) patients who developed severe AKI died. Development of AKI stages 1 to 3 did not show a significant association with in-hospital mortality. However, a Kaplan–Meier curve for in-hospital mortality based on AKI showed that patients with AKI 2 or 3 had a significantly increased risk for in-hospital mortality compared with stage 1 AKI or no AKI (log rank test, P = 0.018) (Fig. 1).
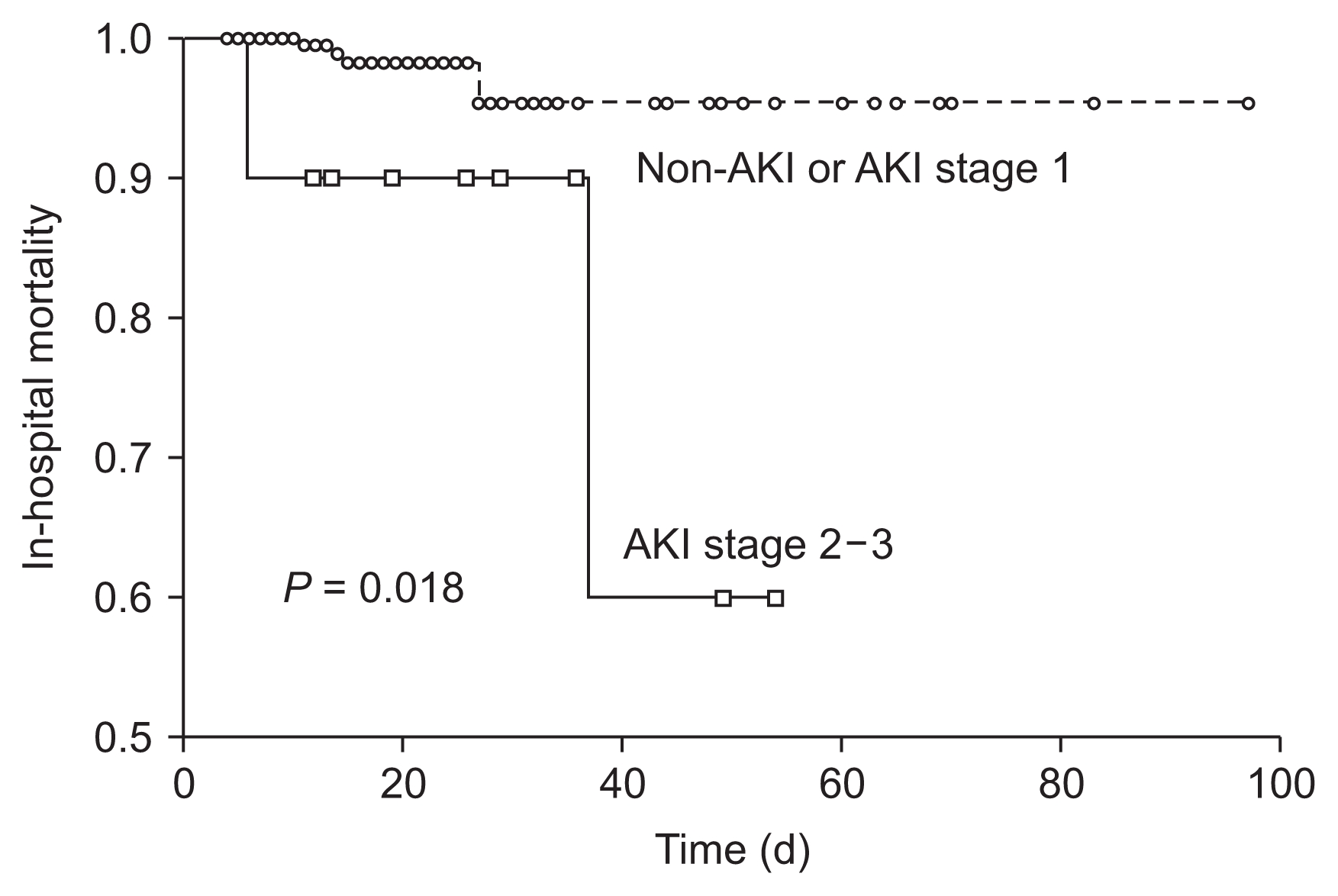
In-hospital mortality for the presence of severe AKI
A Kaplan–Meier curve for in-hospital mortality based on acute kidney injury (AKI) shows that patients with AKI 2 or 3 had a significantly increased risk for in hospital mortality compared with those having stage 1 AKI or non-AKI (log rank test, P = 0.018).
In the univariate analysis, higher age, higher MBP, lower serum albumin, lower baseline eGFR, higher E/e’ ratio, lower EF, higher LV mass index, presence of HFrEF, CAD, incidence of gastrointestinal bleeding, septic shock, mechanical ventilation, cardiac event, pneumonia, transfusion, and severe AKI were significantly associated with in-hospital mortality (P < 0.05) (Table 4). In the multivariate analysis, lower serum albumin (OR, 0.114; 95% CI, 0.011–1.165) was significantly associated with in-hospital mortality. Severe AKI showed a 24.743-fold higher risk for the development of in-hospital mortality (95% CI, 2.822–212.401) (Table 5).

The association of risk factors with in-hospital mortality in elderly patients with femoral neck fracture
Discussion
AKI is a common complication after surgery and is associated with higher hospital cost, prolonged hospital stay, morbidity, and mortality [15–17]. Patients who have undergone AKI are at a higher risk of developing CKD, cardiovascular events, and stroke [15,18].
In our study, 23.5% developed AKI, which is higher than the incidence of up to approximately 10% associated with other non-cardiac surgeries in previous studies [15,16,19–21]. The reports of incidence of AKI have varied by up to 40%, according to the type of surgery [3,15,16,19–22]. Orthopedic surgery was the second most frequent type of surgery associated with AKI in a major surgical setting, following cardiovascular surgery in patients in the intensive care unit [19]. However, most studies have involved critically ill patients or those who have undergone cardiac surgery, and few studies have evaluated AKI in patients who had orthopedic surgery. Previous studies have evaluated the incidence and the risk factors of AKI as a major complication after hip fracture. The incidence of AKI was similar in our study [23,24]. Also consistent with previous studies, use of ACEI/ARB, transfusion, and baseline eGFR were associated with AKI in univariate analysis [23,24]. However, our study showed that E/e’ ratio, hemoglobin, and hypertension were independent risk factors after the adjustment. Our study is meaningful because we showed the relationship of the echocardiographic parameters to AKI.
Multiple factors are associated with postoperative AKI, including neuroendocrine responses; hemodynamic changes such as bleeding, volume imbalance, and systemic inflammation; and nephrotoxic agents that cause tubular injury [22]. In previous studies, multiple factors such as older age, obesity, CKD, HTN, DM, cardiovascular disease, chronic obstructive pulmonary disease, peripheral vascular disease, hypoalbuminemia, use of nephrotoxic agents, and emergency surgery were associated with perioperative AKI [16,19,25–27]. In our study, hypertension, lower hemoglobin, and higher E/e’ ratio were associated with perioperative AKI. These factors, except the E/e’ ratio, are consistent with the classic predictors revealed in the previous studies.
Heart failure with preserved EF is manifested by diastolic function disorder, which is characterized by an increase of the stiffness of the left ventricle and a decrease in the left ventricle [28]. The E/e’ ratio indicates the diastolic function, which correlates well with LV filling pressure [29]. Ventricular hypertrophy can lead to diastolic dysfunction, which in turn leads to impaired distensibility of the myocardium and decreased cardiac output [30]. The reduced cardiac output then decreases renal perfusion and increases the activation of the renin-angiotensin-aldosterone and sympathetic systems, which triggers salt and water retention, which in turn causes venous congestion. The result is an increase in renal venous and intra-abdominal pressure, which worsens renal function [30,31]. A higher E/e’ ratio is an independent predictor of AKI occurring after cardiac surgery [32,33]. An E/e’ ratio > 15 is associated with AKI among patients with ST-segment elevation myocardial infarction [34].
Elderly patients have more severe LV hypertrophy and LV diastolic dysfunction than younger patients [9,10]. The average age of patients with proximal femur fracture has been increasing, so it is meaningful to focus on diastolic function in patients who have experienced femur fracture [35]. We evaluated the echocardiographic parameters associated with diastolic function such as LA dimension, LV mass index, and PA pressure [36–38]. Patients who developed postoperative AKI, preoperative measurements of LA dimension, LV mass index, PA pressure, and E/e’ ratio were significantly higher than non-AKI patients. However, only E/e’ ratio was significant after the adjustment. E/e’ ratio was known to be closely associated with fluid overload [39]. Preoperative volume overload status could be associated the development of AKI after surgery. Careful volume control is needed before and after the surgery, especially in elderly patients.
Unlike stage 1 AKI, EF was an independent risk factor for the development AKI above stage 2. Severe AKI was significantly associated with in-hospital mortality. In univariate analysis, preoperative E/e’ ratio was higher in non-survivors (P = 0.044). However, we could not evaluate the risk of E/e’ ratio for the incidence of mortality in multivariate analysis because the E/e’ ratio was calculated only in 3 (50%) non-survivors. Malnutrition and the presence of severe AKI were significant risk factors for inhospital mortality. We observed only in-hospital mortality, and the incidence was low (2.1%). To better evaluate the association between the E/e’ ratio and mortality, a long-term follow-up study is needed.
This study has several limitations. First, this study is retrospective in nature. Second, the correct baseline renal function was not known in some of the patients. For patients who did not have creatinine laboratory data from 7 to 365 days prior to the study, we defined the baseline creatinine value as the lowest creatinine concentration during the hospitalization. Therefore, the incidence of AKI could have been overestimated. Third, we did not include urine output criteria in the definition of AKI. Finally, the observation period for the development of mortality was short.
In conclusion, this study showed an association between diastolic dysfunction and AKI in elderly patients who underwent surgery for femur neck fracture. Echocardiography and strict volume management can be helpful for improving perioperative outcomes in these patients. In conclusion, elderly patients with femoral neck fracture had a high incidence of AKI. HTN, lower hemoglobin, and higher E/e’ ratio were all associated with AKI, and severe AKI was associated with in-hospital mortality. Therefore, careful management is necessary for high-risk patients after they undergo femoral neck surgery.
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.



