Obesity-related hypertension and chronic kidney disease: from evaluation to management
Article information
Abstract
With the recent obesity pandemic, obesity-related hypertension and its complications (e.g., heart failure, coronary disease, and chronic kidney disease [CKD]) are gaining attention in clinical and research fields. Obesity-related hypertension frequently precedes the onset of CKD and aggravates its progression. In this review, we discuss the role of visceral fat in the pathophysiology of obesity-related hypertension and the potential therapeutic strategies for its prevention and management. Various factors, including the sympathetic nervous system, renin-angiotensin-aldosterone system, and inflammatory pathways, are intricately involved in the pathogenesis of obesity-related hypertension. These factors individually and jointly contribute to the development of hypertension (usually sodium-sensitive or resistant hypertension) and, ultimately, to the progression of CKD. From a clinical standpoint, a decline in renal function in advanced CKD further makes blood pressure control challenging since only a few options are available for blood pressure-lowering medications. Proactive lifestyle modification, pharmacological treatment for obesity, and bariatric surgery can be considered for obesity control and management. Furthermore, intensive blood pressure control is required to prevent and halt the development and progression of CKD.
Introduction
Obesity is a significant chronic disease worldwide [1]. Similar to the global obesity pandemic, the prevalence of obesity in Korea has gradually increased over the last decade. According to the Obesity Fact Sheet in Korea 2021 (endorsed by the Korean Society for the Study of Obesity), the age-adjusted prevalence of obesity in 2019 was 36.3% (obesity is defined as body mass index [BMI] of ≥25 kg/m2) [2,3]. Hypertension is a major cause of death and has the highest disease burden worldwide [1,4,5]. In Korea, the estimated number of people with hypertension exceeded 12 million as of 2019 (hypertension is defined as blood pressure of ≥140/90 mmHg or the use of antihypertensive drugs) [6]. Individuals with hypertension had more comorbidities than normotensive individuals. According to a recent study based on the Korea National Health and Nutrition Examination Survey, the most common comorbidity in patients with hypertension was obesity, followed by dyslipidemia. Indeed, 60% of individuals with hypertension are reported to be obese [7].
Obesity-related hypertension is defined as hypertension accompanied by obesity. It accounts for 65% to 75% of essential hypertension [8–10], is characterized by increased salt sensitivity, and is frequently the cause of resistant hypertension [8–10]. Furthermore, obesity-related hypertension frequently precedes the onset of coronary artery disease, heart failure, and chronic kidney disease (CKD) [10–16]. Meanwhile, obesity is observed in approximately 20% to 25% of patients with CKD worldwide and is also a significant risk factor for CKD development [17]. The impact of obesity on CKD is particularly evident since hypertension and diabetes, which accounts for at least 70% to 75% of end-stage renal disease (ESRD), are mainly caused by obesity [9,17]. Therefore, obesity-related hypertension and resulting CKD necessitates early intervention for obesity and hypertension. Proactive lifestyle modifications, which include decreasing sedentary lifestyles and adopting a healthy diet, are highly recommended for obese individuals [16,18–21]. However, lifestyle modification alone cannot reverse obesity and obesity-related organ dysfunction. Moreover, its effects frequently do not last long. Several pharmacological agents for treating obesity are available; however, their clinical applications are limited. Bariatric surgery can be considered for severe obesity and could benefit blood pressure control [18,22]; however, its application is limited in most Asians with hypertension (including Koreans), as most obese individuals have a BMI of 25–35 kg/m2.
Therefore, it is crucial to understand the pathophysiology of obesity-induced hypertension and interrupt the vicious cycle of obesity-induced hypertension and its consequences. This review focuses on assessing obesity, the pathophysiology, and potential therapeutic strategies for obesity-related hypertension, which is a significant risk factor for CKD.
How to define obesity: fat distribution matters
BMI is widely used to define obesity in clinical practice and large-scale epidemiological studies. For Asians, a BMI of ≥25 kg/m2 is defined as obesity. In detail, BMIs of 25.0–29.9 kg/m2, 30.0–34.9 kg/m2, and ≥35 kg/m2 are classified as class I, II, and III obesity, respectively [2]. Waist circumference (WC) and the waist-to-hip ratio are widely used to assess abdominal obesity. Abdominal obesity is defined as a WC of ≥90 cm and ≥85 cm in males and females, respectively, in the Asian population [2]. Although WC is a feasible measure of abdominal obesity that could reflect the risk of metabolic disease or cardiovascular disease, it does not provide information on body composition (muscle vs. fat) or fat distribution (subcutaneous vs. visceral abdominal fat). Sarcopenic obesity or visceral obesity, frequently known as metabolically unhealthy obesity, is closely associated with adverse outcomes [13,14,23–30]. From this perspective, other methods, such as dual-energy X-ray absorptiometry, bioelectrical impedance analysis, and computed tomography, would provide more in-depth information.
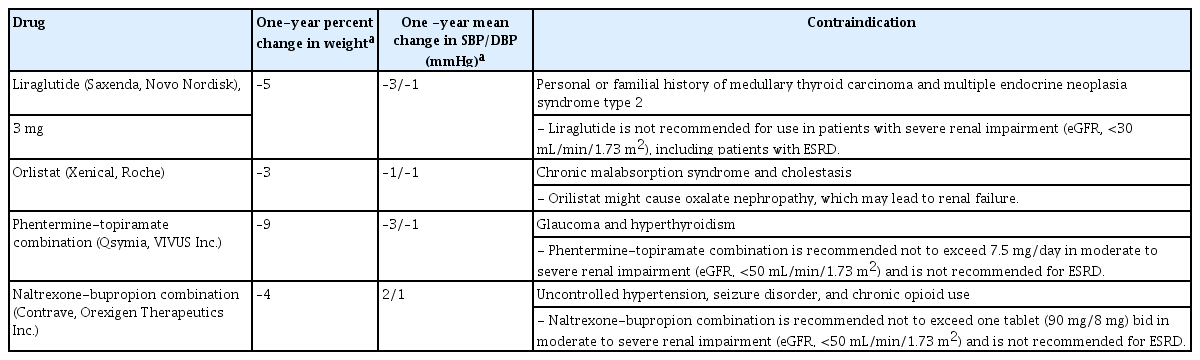
Fat is broadly classified into subcutaneous, visceral, and ectopic fat based on its location or distribution (Table 1). Subcutaneous fat is an adipose tissue located under the skin, which acts as an insulator to prevent heat loss, a barrier against infection, and a physiological buffer for excess lipid storage [24]. Compared to subcutaneous fat, visceral and ectopic fats are associated with an increased risk of metabolic disease, cardiovascular disease, and CKD [23–25,31–36]. Visceral abdominal and epicardial fats surround the intestine and heart, respectively, and correspond to visceral fat (Table 1, Fig. 1). Epicardial fat, which is a unique visceral fat, differs from pericardial fat in terms of its embryological origin, location, and metabolic consequences. It shares a common embryological origin with mesenteric and omental fat (splanchnopleuric mesoderm) and lies inside the visceral pericardium (Fig. 1), whereas pericardial fat originates from the primitive thoracic mesenchyme and is located outside the parietal pericardium [31]. The embryological origin of epicardial fat supports its role as visceral fat. Perirenal fat, including renal sinus fat, corresponds to visceral fat (specifically retroperitoneal fat; Fig. 1). Normally, the renal sinus is a fat-filled compartment located within the medial aspect of the kidney that contains the renal artery and vein, nerves, calyces, and lymphatic drainage. The amount of renal sinus fat also increases with obesity. Recently, there has been a growing interest in renal sinus fat as having a pathologic role in metabolic disease and CKD, given its anatomic location (i.e., a paracrine effect on the kidney and hemodynamic effect due to physical compression of the renal arteries and tubules) [33,36–39]. Increased renal sinus fat is associated with uncontrolled blood pressure and the presence of CKD, even after controlling for BMI [33,37].
Examples of subcutaneous and visceral fats.
Panels A and B are representative abdominal computed tomography (CT) images of normal-weight (A) and obese (B) individuals. Panels C and D show representative cardiac images of obese individuals (C, chest CT; D, echocardiography). Green and yellow colors denote subcutaneous and visceral fats, respectively. Yellow asterisks indicate epicardial fat.
Ao, aorta; LV, left ventricle; RV, right ventricle.
Postulated mechanisms behind obese-related hypertension and chronic kidney disease
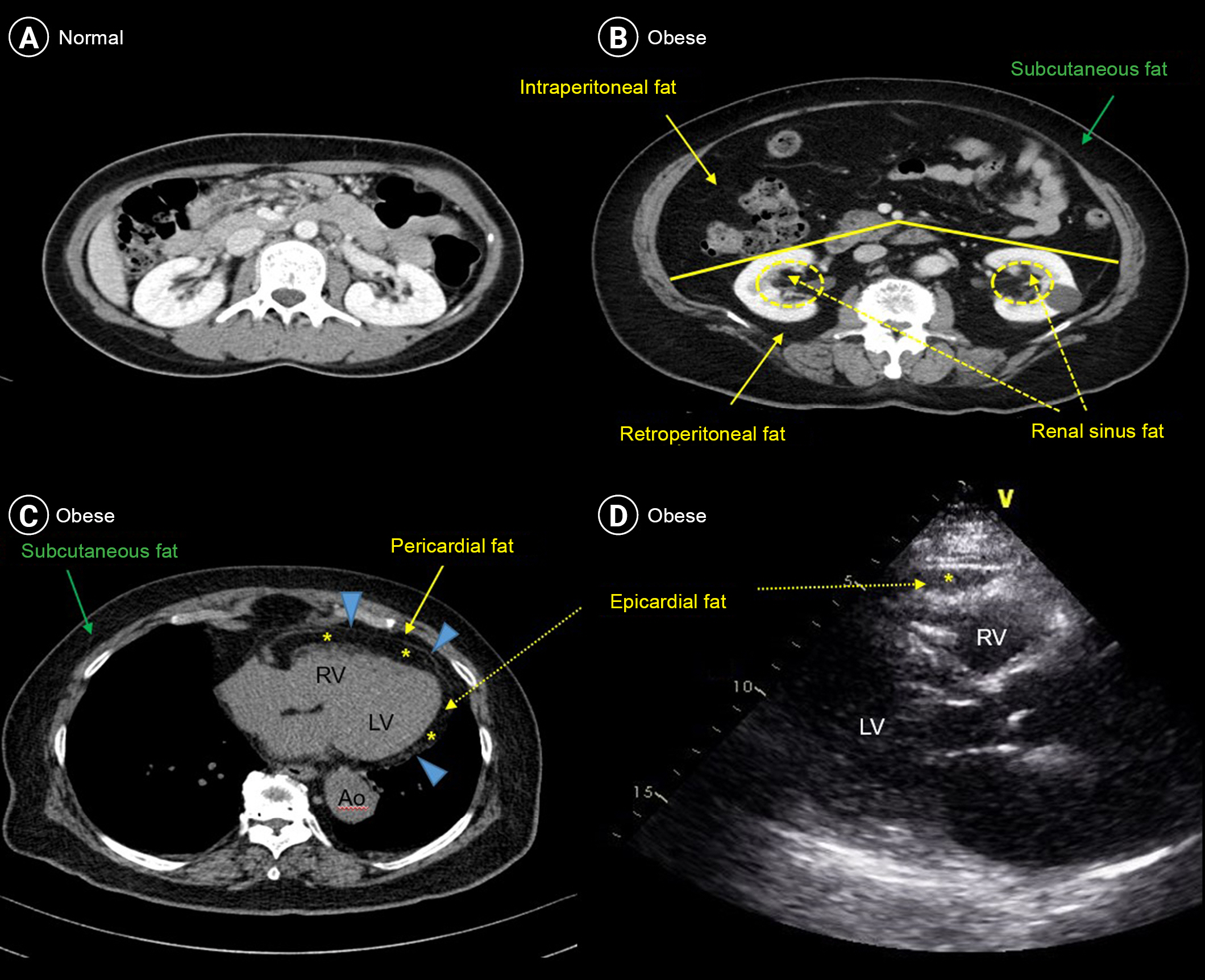
The obese population exhibits higher blood pressure than the normal-weight population, even before the development of hypertension [13,14,40]. However, the responsible mechanisms underlying the association between obesity, hypertension, and CKD are complex and are still an area of further research. As illustrated in Fig. 2, several pathophysiological factors, such as hemodynamic and inflammatory factors, genetic and epigenetic factors, and comorbidities, are intricately intertwined in the initiation and progression of obesity-induced hypertension and CKD [8-10,40–42].
Pathogenesis of obesity-related HTN and CKD.
Several factors have been implicated in the pathogenesis of obesity-related HTN, which ultimately causes CKD. Cardiovascular disease (CVD) is another commonly found adverse consequence of obesity-induced HTN, which also adversely affects CKD development and progression.
CKD, chronic kidney disease; HTN, hypertension; NP, natriuretic peptide; MR, mineralocorticoid receptor; RAAS, renin-angiotensin-aldosterone system; SNS, sympathetic nervous system.
Hemodynamic factors: sodium retention via the neurohormonal pathway
Renal sodium retention is a key factor in the pathogenesis of obesity-related hypertension and organ dysfunction [8,11,43]. Neurohormonal derangements, such as activation of the sympathetic nervous system (SNS) and renin-angiotensin-aldosterone system (RAAS) and deficiency of the natriuretic peptide system, are antedated by renal sodium retention.
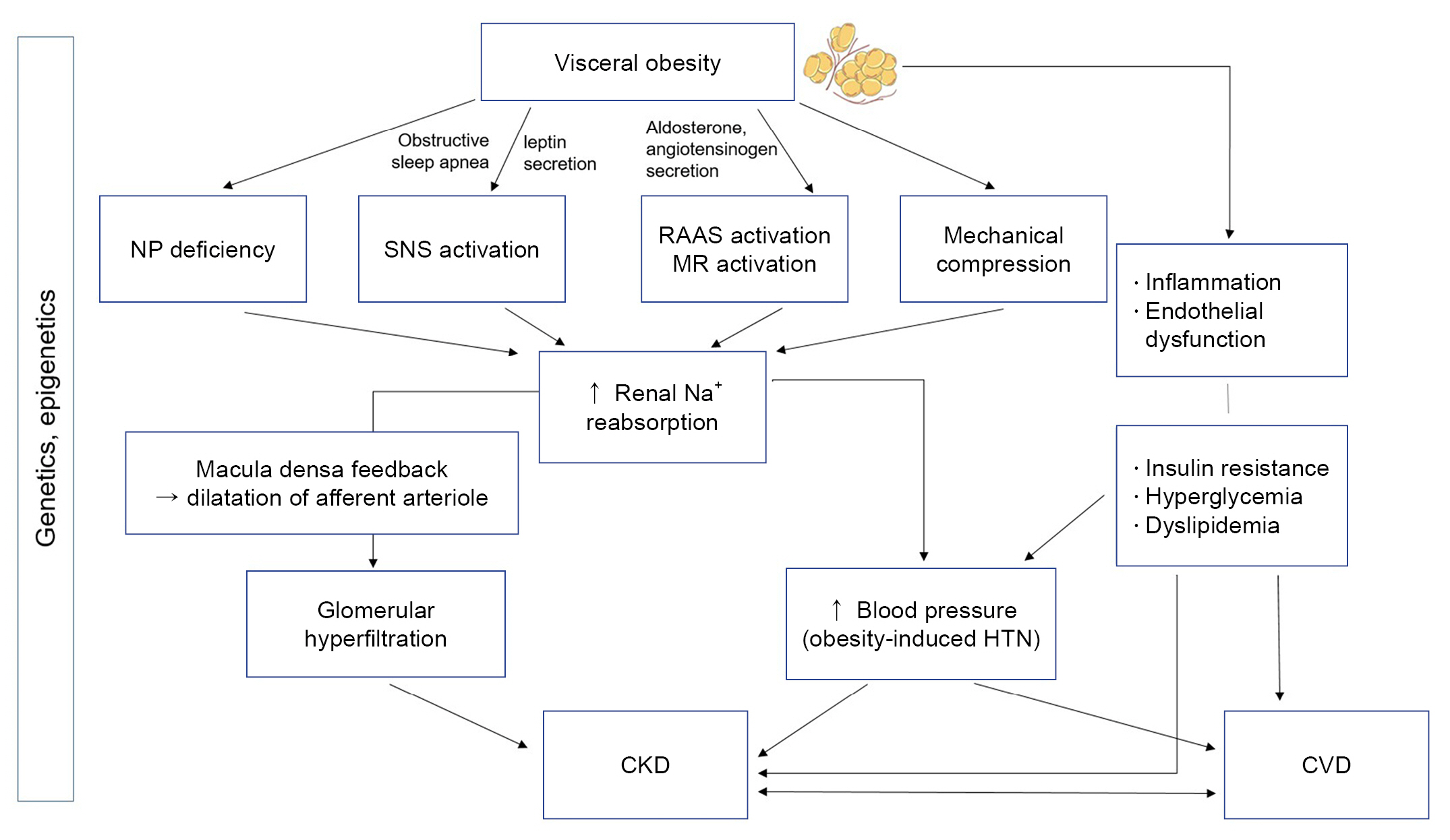
Mechanically, accumulated renal sinus fat might compress the thin loop of Henle (tubule) and vasa recta (arteriole), consequently reducing tubular and medullary blood flow. This leads to increased sodium reabsorption in the thick loop of Henle [44]. A decreased sodium concentration in the distal tubule is sensed by the macula densa, which activates afferent arteriole dilatation, contributing to glomerular hyperfiltration and, ultimately, CKD development. Sodium retention due to increased renal tubular sodium reabsorption is also directly linked to elevated blood pressure, contributing to CKD progression (Fig. 3).
The suggested renal hemodynamic mechanisms by which renal sinus fat induces hypertension and CKD progression.
CKD, chronic kidney disease.
SNS activation also mediates obesity-induced hypertension [45–48]. Obesity decreases the parasympathetic tone and increases the sympathetic tone [8]. Several factors are interwoven in obesity-related SNS-mediated hypertension, including impaired baroreceptor reflexes, chemoreceptor activation, the leptin-proopiomelanocortin pathway, and hyperinsulinemia [9,49–53]. In a previous animal study, a high-fat diet resulted in the rapid development of hypertension, accompanied by elevated insulin, leptin, and renal sympathetic nerve activity within 1 week. Intriguingly, resuming a normal diet recovered insulin and leptin levels, but not blood pressure or renal sympathetic nerve activity. This study’s findings suggest that elevated insulin and leptin levels are linked to the initiation of hypertension rather than its maintenance, and enhanced sympathetic drive and impaired baroreceptor reflexes may be involved in the pathogenesis of obesity-induced hypertension [49]. Conversely, body weight reduction with a hypocaloric diet resulted in increased insulin sensitivity and restoration of the baroreflex [54]. In obese individuals, hypoxemia may activate peripheral chemoreceptors, thereby contributing to SNS activation-mediated hypertension. Obstructive sleep apnea is a frequent comorbidity in obese individuals with resistant hypertension. Hypoxia during sleep activates chemoreceptors and the SNS, contributing to elevated blood pressure, particularly nocturnal hypertension [55,56]. Leptin is an adipokine that regulates autonomic, cardiovascular, and metabolic functions and is highly elevated in obese individuals. Specifically, leptin stimulates the leptin receptor and activates proopiomelanocortin neurons in the hypothalamus. Therefore, it leads to an increase in renal sympathetic nerve activity, sodium retention, and hypertension [8,57].
RAAS activation and natriuretic peptide deficiency also play an important role in obesity-related hypertension. Under normal conditions, volume overload or hypertension suppresses renin secretion and angiotensin II production. However, in obese individuals, renin activity, angiotensinogen, angiotensin II, and aldosterone levels are inappropriately normal or slightly elevated despite sodium retention and elevated blood pressure. The dysregulated RAAS system in obesity originates from a direct increase in the RAAS system and an indirect increase due to natriuretic peptide deficiency [58]. Adipocytes can directly produce angiotensinogen, angiotensin II, and aldosterone or indirectly enhance aldosterone secretion from the adrenal gland by releasing leptin and catecholamine [58–60]. The level of natriuretic peptide is reduced in obesity [11,61]. Increased levels of neprilysin in obesity lead to the degradation of the natriuretic peptide, which consequently stimulates the RAAS [62].
Inflammatory factors
Inflammation is another major pathophysiological axis involved in obesity-related hypertension, as extensively described in previous studies [8,9]. Recent research suggests that adipose tissue is a dynamic and complex endocrine organ that secretes various hormones rather than a simple energy storage organ. Adipokines (circulating cytokines released from adipose tissue, e.g., adiponectin, leptin, and resistin) and inflammatory cytokines (e.g., tumor necrosis factor [TNF] and interleukin-6 [IL-6]) may be important targets for managing obesity-related hypertension. An imbalance between the protective and pathologic adipokines contributes to the pathogenesis of obesity-related hypertension and CKD. Adiponectin is a representative adipokine that exerts a protective effect, such as anti-inflammatory and anti-atherosclerotic effects. A previous study showed increased albuminuria and renal fibrosis in an adiponectin knockout mouse [63]. Another study demonstrated decreased adiponectin and increased high-sensitivity C-reactive protein and IL-6 in obese women [64]. Adiponectin appears to exert its beneficial effect by stabilizing endothelial/podocyte function and reducing inflammation. The pathologic role of leptin in relation to SNS activation has been partly discussed in the previous section. CKD is associated with elevated leptin levels since the kidney is the primary organ for leptin clearance [65]. Leptin stimulates endocapillary proliferation and mesangial collagen deposition in the glomerulus by stimulating TNF-beta, leading to glomerulosclerosis [65,66]. In CKD and ESRD, different adipokine profiles of elevated leptin and adiponectin levels are observed [67]. Furthermore, cachexia (lower BMI) in the setting of a uremic milieu has also been reported to elevate the adiponectin level. Contrary to obesity or other metabolic diseases, the role of adiponectin in advanced CKD is unclear. A paradoxical increase in adiponectin in CKD is believed to be related to adiponectin resistance or compensatory elevation in CKD to counterbalance the effects of inflammatory cytokines in the uremic milieu [68]. A study among Asian adults showed that elevated levels of adiponectin, leptin, and leptin to adiponectin ratio were associated with CKD development [69]. Another study reported increased adiponectin, leptin, IL-6, and TNF-alpha levels in patients with CKD. Moreover, these adipokines and inflammatory cytokines levels increased with advancing CKD stages [70]. Although the exact effect of adipokines in obese patients with CKD requires further investigation, abnormal adipokine profiles in conjunction with inflammatory cytokine activation appear to play a role in CKD initiation and progression. Other novel adipokines are involved in obesity-related hypertension and CKD, such as resisistin, visfatin, progranulin, apelin, and chemerin, which warrant further studies [66]. TNF and IL-6 are proinflammatory cytokines that play a crucial role in the pathogenesis of obesity-related hypertension and CKD. Increased TNF-alpha and IL-6 levels contribute to low-grade systemic inflammation, oxidative stress, endothelial dysfunction, insulin resistance, and vasoconstriction, leading to the development of hypertension and CKD [71]. Furthermore, in the setting of CKD, adipose tissue undergoes changes that lead to adipose tissue aging, which is characterized by impaired adipogenesis, increased adipocyte size, and adipose tissue fibrosis [71]. These changes are believed to be related to increased inflammation, oxidative stress, and the accumulation of advanced glycation end-products in CKD [71]. Collectively, the release of adipokines and inflammatory cytokines from the adipose tissue can elevate blood pressure and damage the kidney through endothelial dysfunction, inflammation, and oxidative stress, while CKD-related metabolic dysfunction accelerates adipose tissue aging, leading to a vicious cycle, which indicates bidirectional relationship.
Other factors: comorbidities and genetic and epigenetic factors
Additionally, common comorbidities, such as diabetes and dyslipidemia, which are components of metabolic syndrome, also activate the RAAS, SNS, and inflammatory pathways and participate in the development and progression of obesity-related hypertension and target-organ damage. Furthermore, genetic and epigenetic factors are involved in obesity-related hypertension. Indeed, not all obese individuals develop hypertension or target-organ damage. Among individuals with a genetic predisposition, epigenetic gene regulation (such as DNA methylation and histone modification) coupled with lifestyle factors can play a role in disease presentation [72]. For example, nutrition and physical activity can positively and negatively modify epigenetic gene regulation. Jun et al. [73] previously reported that a high-fat diet altered histone modification in the peroxisome proliferator-activated receptor alpha (PPARα)-network in apolipoprotein E-deficient mice. Another study showed that an increase in exercise in sedentary adults leads to an increase in the expression of genes regulating mitochondrial function and fuel usage, such as PPAR-γ, PPAR-γ coactivator 1 alpha (PGC-1α), pyruvate dehydrogenase kinase isoenzyme 4 (PDK4), and PPAR-δ. This was accompanied by a decrease in methylation on the respective promoters of these proteins [74]. A recent study found that a 6-month exercise induces genome-wide changes in DNA methylation in human adipose tissue, potentially affecting adipocyte metabolism and altering the levels of DNA methylation in many genes, including those involved in obesity and type 2 diabetes [75].
In summary, multiple factors are involved in the pathogenesis of obesity-induced hypertension. These factors individually and jointly contribute to the development of hypertension (usually sodium-sensitive or resistant hypertension) and, ultimately, CKD progression (Fig. 2). Furthermore, a decline in renal function in advanced CKD makes blood pressure control more challenging since only a few options for blood pressure-lowering medications are available.
How to manage obesity-related hypertension
The management of obesity-related hypertension can target both obesity and hypertension (Fig. 4). Obese individuals with prehypertension (blood pressure, 130–139/80–89 mmHg) or stage 1 hypertension (blood pressure, 140–159/90–99 mmHg) with low cardiovascular risk profiles could be initially managed for obesity [76,77]. However, combined antihypertensive drug treatment and obesity management should be considered in obese individuals with prehypertension with multiple (≥3) cardiovascular risk factors/cardiovascular disease/CKD, inadequately controlled stage 1 hypertension despite intensive lifestyle modification, and stage 2 hypertension (blood pressure, ≥160/100 mmHg) [76,77]. Renal denervation therapy may be considered in selected cases of resistant hypertension.

Therapeutic strategies in obesity-related HTN according to obesity, blood pressure, and underlying diseases, including CKD and CVD.
In advanced CKD, these drugs (marked with asterisks) require close monitoring of renal function and electrolytes.
ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; BMI, body mass index; CCB, calcium channel blocker; CKD, chronic kidney disease; CVD, cardiovascular disease; HTN, hypertension.
Lifestyle modification
Intensive lifestyle modifications, such as diet modification, regular exercise, and alcohol moderation, are crucial for managing obesity-related hypertension. It is recommended to lose 5% to 10% of body weight over the first 6 months in obese people with comorbidities [77,78]. Therefore, to achieve this goal, multimodal lifestyle modifications should be jointly performed.
Diet modification includes calorie-reduced and low-sodium diets and healthy diet patterns [77–80]. The most widely accepted healthy diet pattern is the Mediterranean diet and Dietary Approaches to Stop Hypertension (DASH). A recent meta-analysis revealed that the overall pooled net effect of dietary intervention on systolic/diastolic blood pressure was –3.1/–1.8 mmHg. Among the various dietary interventions, the DASH diet had the strongest blood pressure-lowering effect (systolic/diastolic blood pressure, –7.6/–4.2 mmHg) [81]. The DASH-Sodium trial demonstrated that the blood pressure-lowering effect would be more potent if a low-sodium diet and a DASH diet were combined. Compared with the high-sodium control diet, the low-sodium DASH diet significantly reduced systolic blood pressure, which was more remarkable in patients who had elevated baseline blood pressure (reduction of 20.8 mmHg in the baseline systolic blood pressure ≥ 150 mmHg) [79].
Physical activity and exercise are important lifestyle factors for managing obesity and hypertension [82–84]. A recent network meta-analysis revealed that exercise could be as effective as pharmacologic therapy in lowering blood pressure, although the effect size of blood pressure-lowering was slightly greater with pharmacologic therapy than with exercise [84]. Interestingly, a study demonstrated that combined diet and exercise had the most considerable effect on weight loss compared to either diet or exercise alone (10.8%, 8.5%, and 0.8%, respectively) in postmenopausal women [85], which implies the necessity for multifaceted effort in diet and exercise.
Additionally, alcohol moderation is essential; however, it is frequently neglected in lifestyle modification for blood pressure control. Considerable evidence supports the association between heavy drinking and obesity [86,87]. A previous meta-analysis clearly showed that any amount of alcohol consumption was associated with blood pressure elevation in Asian men [88].
More comprehensive counseling is needed for overweight and obese patients with hypertension. However, long-term weight loss maintenance is often challenging due to the so-called yo-yo effect. Therefore, continued and regular counseling by medical professionals is required to promote proactive lifestyle modifications.
Pharmacological treatment for obesity
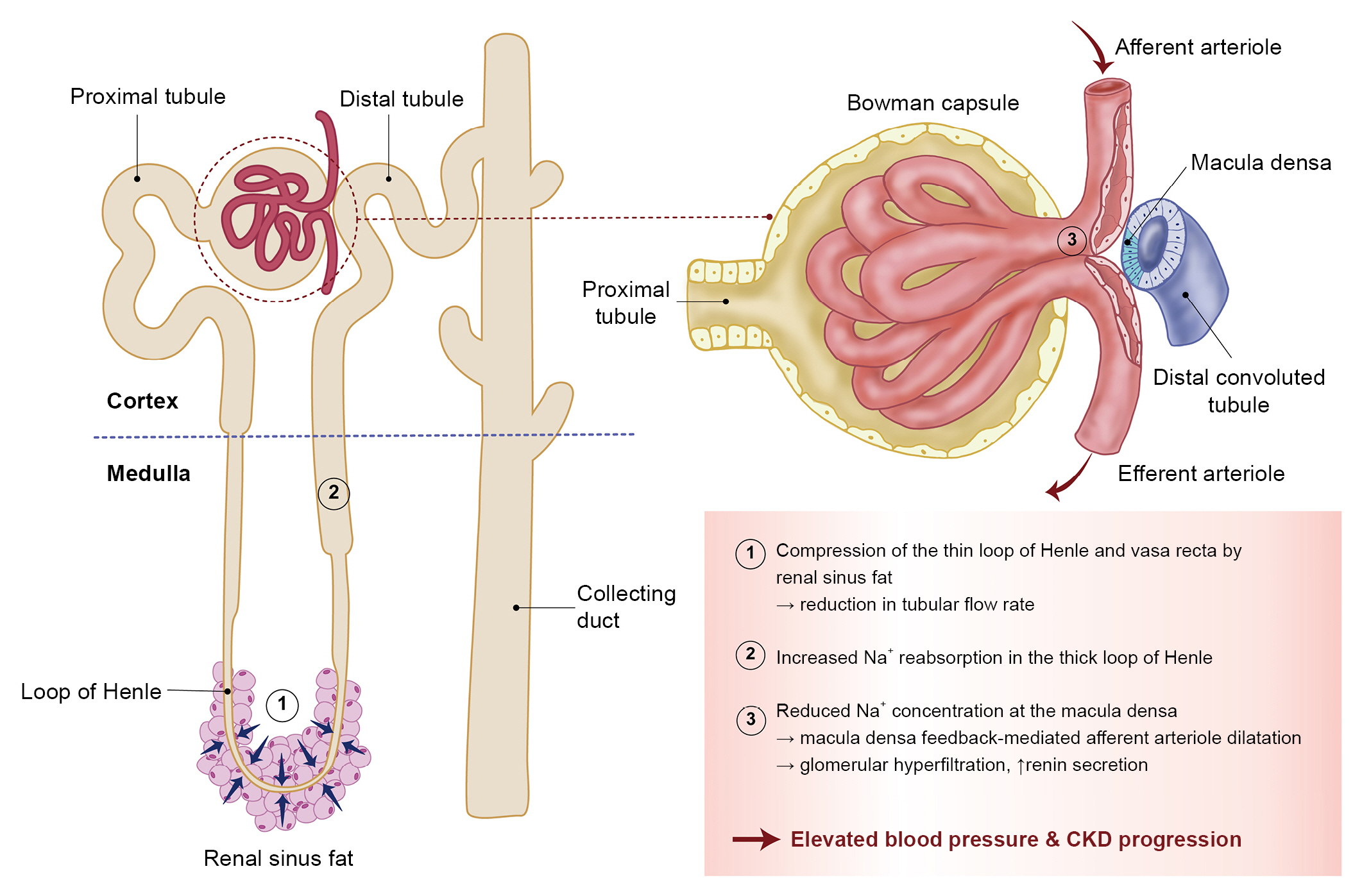
Currently, pharmacologic treatment could be considered in patients with obesity (BMI of ≥25 kg/m2) who could not lose weight despite comprehensive lifestyle modification according to the guidelines of the Korean Society for the Study of Obesity [89]. Although the insurance system does not cover these drugs, four medical options are available for long-term treatment (≥12 weeks) of obesity in Korea (liraglutide, orlistat, phentermine-topiramate combination, and naltrexone-bupropion combination) [90]. However, lorcaserin (Belviq, Eisai Inc.) is not currently allowed for use in Korea because of the increased risk of cancer development [91]. Detailed information regarding its weight loss effect and caution are beyond the scope of this review; however, such data can be found in other reviews [90,92]. Liraglutide (Saxenda, Novo Nordisk) is a glucagon-like peptide 1 (GLP-1) receptor agonist. At the highest dose of 3 mg/day, liraglutide showed a benefit in weight loss (5%–10% body weight loss). Orlistat acts by inhibiting intestinal fat absorption. The phentermine/topiramate combination has the most potent weight loss effect among currently available obesity drugs [93], although it should be avoided in patients with CKD because topiramate is related to the inhibition of carbonic anhydrase activity and potentially leads to metabolic acidosis, hypokalemia, and renal stones [77]. The naltrexone-bupropion combination results in weight loss but might cause slight blood pressure elevation (mean 2/1 mmHg increase in systolic/diastolic blood pressure) [94]. Table 2 presents additional information regarding the effects of each of the four drugs on weight loss, blood pressure, and contraindications for each of the four drugs. Other promising drugs, such as the sodium-glucose cotransporter 2 inhibitor, setmelanotide, and other GLP-1 agonists, are under development [11,90,95]. Semaglutide, which is another GLP-1 receptor agonist, at a 2.4-mg subcutaneous injection (higher dose formulation of semaglutide, once-weekly dose; Wegovy, Novo Nordisk), was approved by the U.S. Food and Drug Administration for weight loss. Recently (April 27, 2023), the Korean Food and Drug Administration also approved its use as an obesity drug and will be released in Korea shortly (around the end of 2023 or early 2024). Unlike liraglutide (Saxenda), Wegovi has the merit of the convenience of enabling once-weekly injection, and it demonstrated a larger reduction in body weight (14.9%) and systolic blood pressure (6.2 mmHg) from baseline to 68 weeks [96].
Bariatric surgery
Currently, bariatric surgery is indicated for patients with a BMI of ≥35 kg/m2 or ≥30 kg/m2 with comorbidities, such as hypertension and diabetes. The number of bariatric surgeries has increased since reimbursement in Korea in 2019. Common surgical procedures include gastric sleeve, gastric bypass, gastric band, and intragastric balloons. Weight loss and metabolic improvement (including lowering of blood pressure) are believed to be related to decreased appetite and enhanced satiety. In the Gastric Bypass to Treat Obese Patients With Steady Hypertension trial, patients randomized to gastric bypass were six times more likely to reduce ≥30% of the total number of antihypertensive drugs while maintaining controlled blood pressure levels than those randomized to medical therapy. Moreover, half of the patients who underwent gastric bypass (51%) also showed remission of hypertension (blood pressure, <140/90 mmHg without medication) [22].
Antihypertensive drug treatment
Despite proactive lifestyle modifications, most patients with obesity and hypertension eventually require antihypertensive medications. Similar to the general population, four drugs (angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, calcium channel blockers, diuretics, and β-blockers) can be considered for the treatment of obesity-related hypertension. Special attention, regular kidney function, and electrolyte status monitoring are warranted in patients with CKD. The Kidney Disease: Improving Global Outcomes (KDIGO) 2021 guidelines recommended strict blood pressure control in adult patients with CKD with elevated blood pressure when tolerated. It also emphasized the need for accurate blood pressure measurement [97–99]. However, the evidence supporting strict blood pressure in patients with CKD is rather weak (based on a single randomized clinical trial, the Systolic Blood Pressure Intervention Trial [SPRINT]), which warrants further studies [97]. In the recently updated guideline for hypertension in Korea, the target blood pressure goal in CKD differs according to the presence of albuminuria. A target blood pressure of <140/90 mmHg is recommended for patients with CKD without albuminuria. However, a stricter blood pressure goal of <130/80 mmHg is recommended for patients with CKD with albuminuria [76]. Moreover, a recent study by Lee et al. [100] demonstrated that intensive blood pressure control in patients with CKD is cost-effective.
Conclusion
Obesity, particularly visceral fat, can lead to hypertension and CKD. Multiple pathways, such as SNS and RAAS activation, natriuretic peptide deficiency, the inflammatory pathway, comorbidity, and genetic/epigenetic factors, are involved in the pathogenesis of obesity-related hypertension and CKD. Therefore, both obesity and hypertension should be considered for therapeutic target. Proactive lifestyle modification, pharmacological treatment for obesity, and bariatric surgery can be considered to control and manage obesity. Furthermore, intensive blood pressure control is warranted to prevent and halt CKD development and progression.
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (RS-2022-00166313 and NRF-2021R1A2C1093768).
Data sharing statement
The data presented here are available on request from the corresponding author.
Authors’ contributions
Conceptualization, Validation: MHJ, SHI
Investigation, Supervision: SHI
Funding acquisition: MHJ, SHI
Writing–original draft: MHJ
Writing–review & editing: SHI
All authors read and approved the final manuscript.