1. GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015.
Lancet 2016;388:1659–1724.


2. Yang YS, Han BD, Han K, Jung JH, Son JW; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019.
J Obes Metab Syndr 2022;31:169–177.



3. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014.
JAMA 2016;315:2284–2291.


5. Jung MH, Yi SW, An SJ, Yi JJ. Age-specific associations between systolic blood pressure and cardiovascular mortality.
Heart 2019;105:1070–1077.


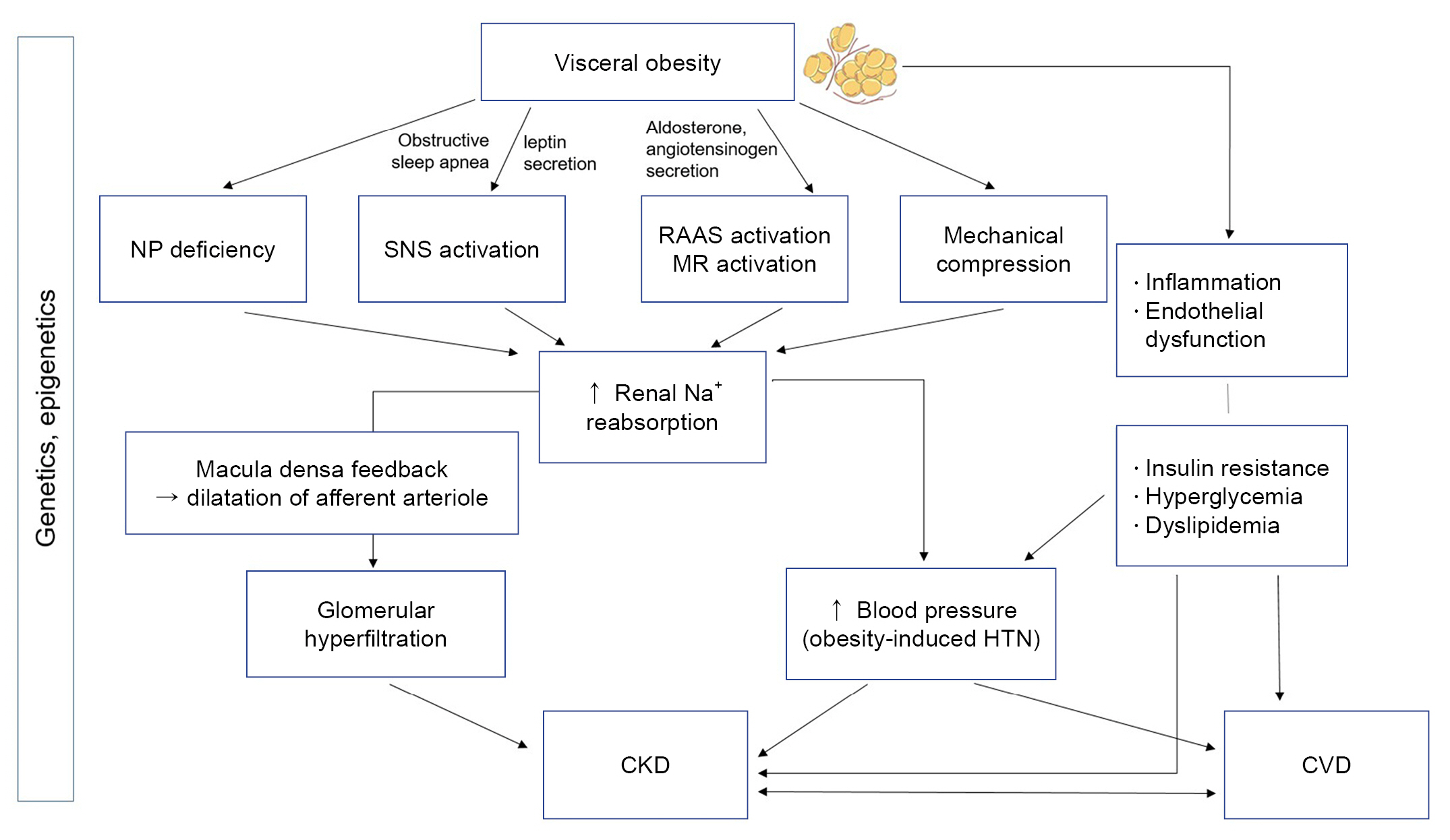
8. Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms.
Circ Res 2015;116:991–1006.



9. Hall JE, Mouton AJ, da Silva AA, et al. Obesity, kidney dysfunction, and inflammation: interactions in hypertension.
Cardiovasc Res 2021;117:1859–1876.



12. Jung MH, Ihm SH, Lee DH, et al. Combined effect of elevated blood pressure and obesity on left ventricular diastolic function.
CardioMetab Syndr J 2022;2:39–46.


13. Jung MH, Ihm SH, Lee DH, et al. Sex-specific associations of obesity with exercise capacity and diastolic function in Koreans.
Nutr Metab Cardiovasc Dis 2021;31:254–262.


14. Jung MH, Ihm SH, Park SM, et al. Effects of sarcopenia, body mass indices, and sarcopenic obesity on diastolic function and exercise capacity in Koreans.
Metabolism 2019;97:18–24.


17. Friedman AN, Kaplan LM, le Roux CW, Schauer PR. Management of obesity in adults with CKD.
J Am Soc Nephrol 2021;32:777–790.



18. Hall ME, Cohen JB, Ard JD, et al. Weight-loss strategies for prevention and treatment of hypertension: a scientific statement from the American Heart Association.
Hypertension 2021;78:e38–e50.

19. Kim HL, Chung J, Kim KJ, et al. Lifestyle modification in the management of metabolic syndrome: statement from Korean Society of CardioMetabolic Syndrome (KSCMS).
Korean Circ J 2022;52:93–109.



20. An SJ, Jung MH, Ihm SH, Yang YJ, Youn HJ. Effect of physical activity on the cardiometabolic profiles of non-obese and obese subjects: results from the Korea National Health and Nutritional Examination Survey.
PLoS One 2019;14:e0208189.



21. Ihm SH. Pathophysiology and optimal management of hypertension in patients with cardiometabolic syndrome.
CardioMetab Syndr J 2021;1:46–65.


22. Schiavon CA, Bersch-Ferreira AC, Santucci EV, et al. Effects of bariatric surgery in obese patients with hypertension: the GATEWAY Randomized Trial (gastric bypass to treat obese patients with steady hypertension).
Circulation 2018;137:1132–1142.


26. Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease.
Front Cardiovasc Med 2020;7:22.



29. Nauli AM, Matin S. Why do men accumulate abdominal visceral fat?
Front Physiol 2019;10:1486.



30. Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease.
Circ Res 2016;118:1752–1770.


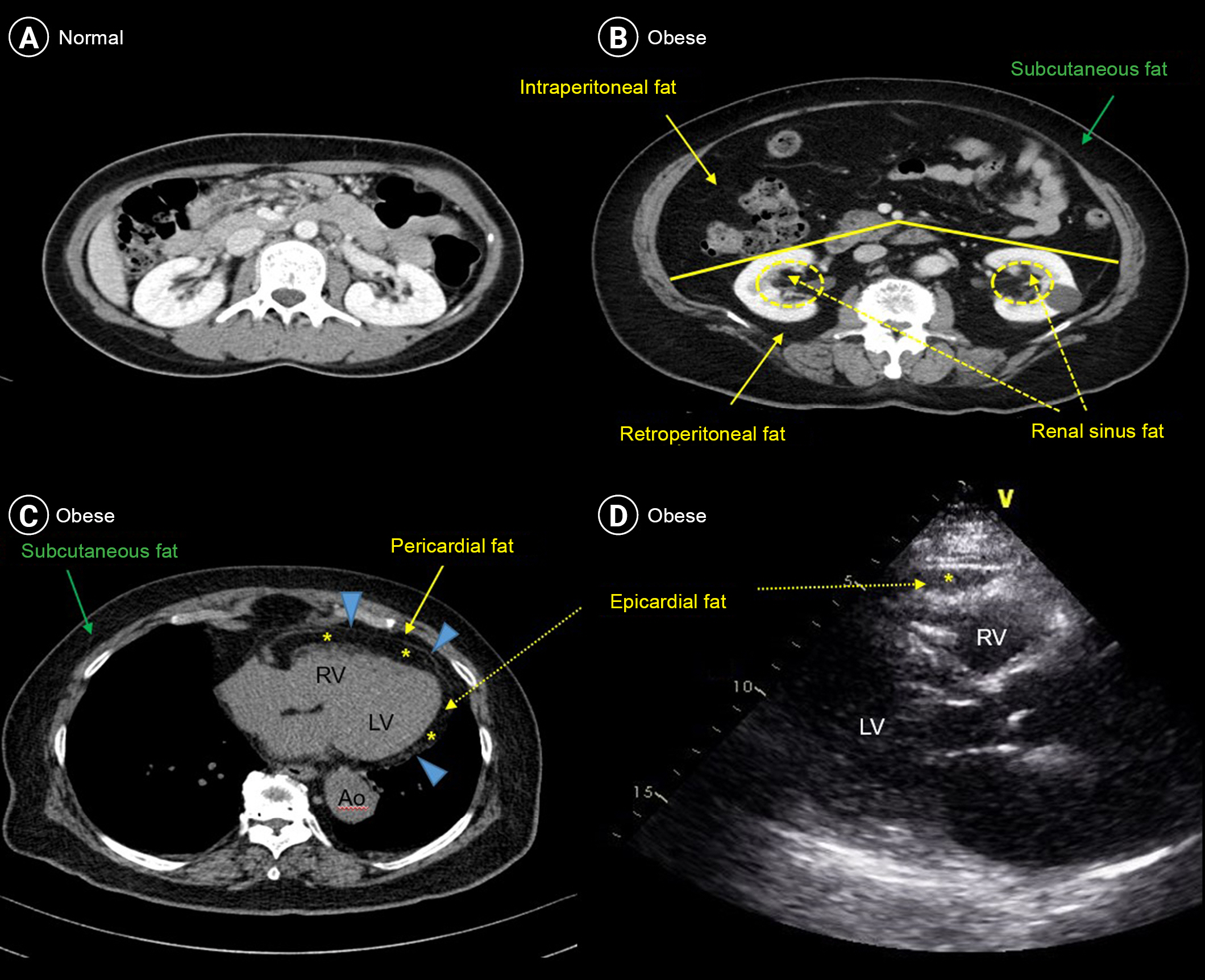
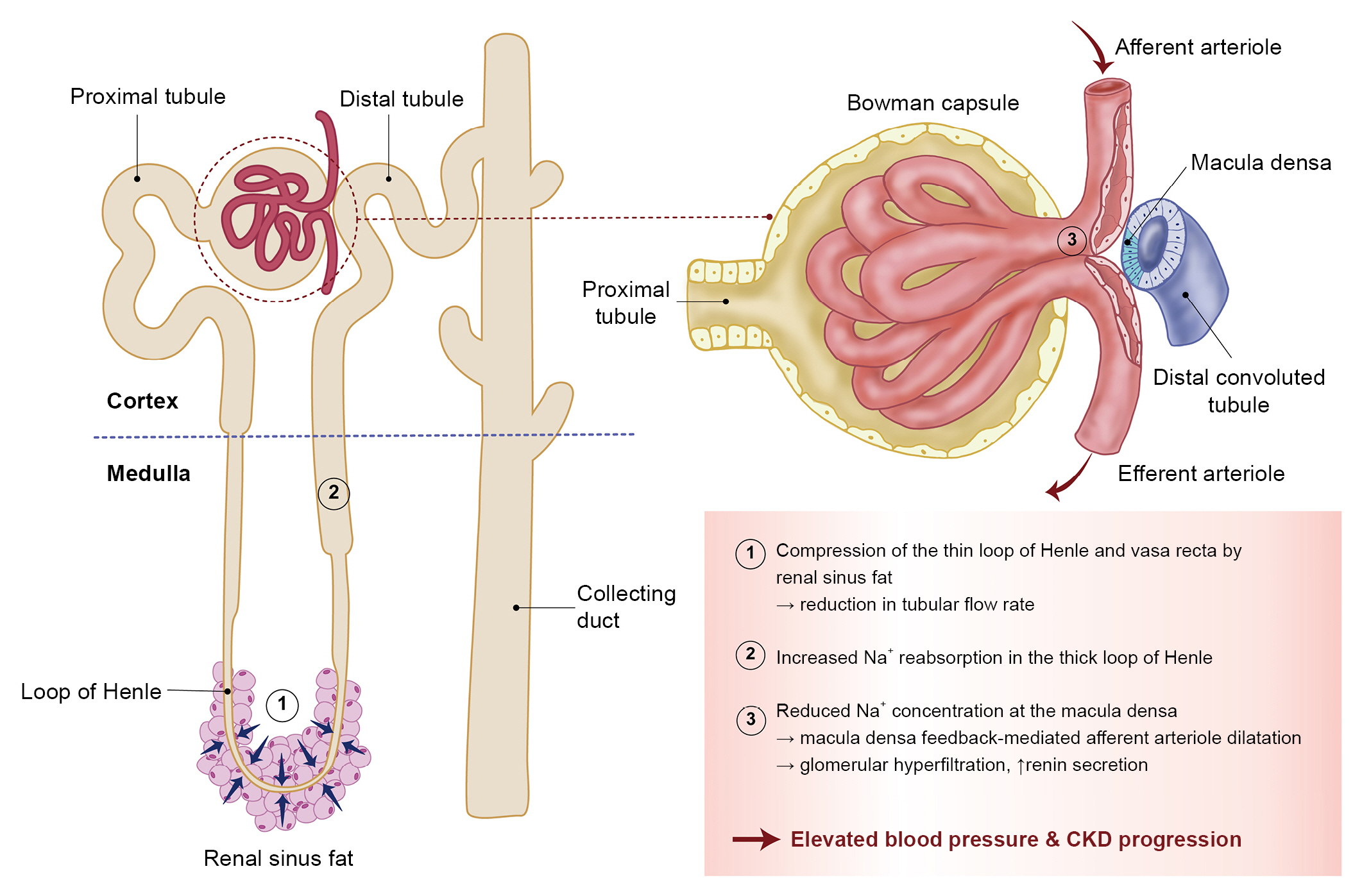
33. Chughtai HL, Morgan TM, Rocco M, et al. Renal sinus fat and poor blood pressure control in middle-aged and elderly individuals at risk for cardiovascular events.
Hypertension 2010;56:901–906.


34. Ayton SL, Gulsin GS, McCann GP, Moss AJ. Epicardial adipose tissue in obesity-related cardiac dysfunction.
Heart 2022;108:339–344.


35. Iacobellis G. Local and systemic effects of the multifaceted epicardial adipose tissue depot.
Nat Rev Endocrinol 2015;11:363–371.



36. Grigoraș A, Balan RA, Căruntu ID, et al. Perirenal adipose tissue-current knowledge and future opportunities.
J Clin Med 2021;10:1291.



37. Foster MC, Hwang SJ, Porter SA, Massaro JM, Hoffmann U, Fox CS. Fatty kidney, hypertension, and chronic kidney disease: the Framingham Heart Study.
Hypertension 2011;58:784–790.


38. Notohamiprodjo M, Goepfert M, Will S, et al. Renal and renal sinus fat volumes as quantified by magnetic resonance imaging in subjects with prediabetes, diabetes, and normal glucose tolerance.
PLoS One 2020;15:e0216635.



39. Spit KA, Muskiet MH, Tonneijck L, et al. Renal sinus fat and renal hemodynamics: a cross-sectional analysis.
MAGMA 2020;33:73–80.



40. Kotsis V, Stabouli S, Papakatsika S, Rizos Z, Parati G. Mechanisms of obesity-induced hypertension.
Hypertens Res 2010;33:386–393.



41. Kotsis V, Jordan J, Micic D, et al. Obesity and cardiovascular risk: a call for action from the European Society of Hypertension Working Group of Obesity, Diabetes and the High-risk Patient and European Association for the Study of Obesity: part A: mechanisms of obesity induced hypertension, diabetes and dyslipidemia and practice guidelines for treatment.
J Hypertens 2018;36:1427–1440.

42. Kotsis V, Tsioufis K, Antza C, et al. Obesity and cardiovascular risk: a call for action from the European Society of Hypertension Working Group of Obesity, Diabetes and the High-risk Patient and European Association for the Study of Obesity: part B: obesity-induced cardiovascular disease, early prevention strategies and future research directions.
J Hypertens 2018;36:1441–1455.

44. Hall JE, Brands MW, Henegar JR. Mechanisms of hypertension and kidney disease in obesity.
Ann N Y Acad Sci 1999;892:91–107.


45. Grassi G, Biffi A, Seravalle G, et al. Sympathetic neural overdrive in the obese and overweight state.
Hypertension 2019;74:349–358.


47. Lambert E, Sari CI, Dawood T, et al. Sympathetic nervous system activity is associated with obesity-induced subclinical organ damage in young adults.
Hypertension 2010;56:351–358.


48. Van Vliet BN, Hall JE, Mizelle HL, Montani JP, Smith MJ Jr. Reduced parasympathetic control of heart rate in obese dogs.
Am J Physiol 1995;269:H629–H637.


49. Armitage JA, Burke SL, Prior LJ, et al. Rapid onset of renal sympathetic nerve activation in rabbits fed a high-fat diet.
Hypertension 2012;60:163–171.


50. Barzel B, Lim K, Davern PJ, Burke SL, Armitage JA, Head GA. Central proopiomelanocortin but not neuropeptide Y mediates sympathoexcitation and hypertension in fat fed conscious rabbits.
J Hypertens 2016;34:464–473.


51. Lim K, Barzel B, Burke SL, Armitage JA, Head GA. Origin of aberrant blood pressure and sympathetic regulation in diet-induced obesity.
Hypertension 2016;68:491–500.


52. Mouton AJ, Li X, Hall ME, Hall JE. Obesity, hypertension, and cardiac dysfunction: novel roles of immunometabolism in macrophage activation and inflammation.
Circ Res 2020;126:789–806.



53. Shi Z, Zhao D, Cassaglia PA, Brooks VL. Sites and sources of sympathoexcitation in obese male rats: role of brain insulin.
Am J Physiol Regul Integr Comp Physiol 2020;318:R634–R648.



54. Grassi G, Seravalle G, Colombo M, et al. Body weight reduction, sympathetic nerve traffic, and arterial baroreflex in obese normotensive humans.
Circulation 1998;97:2037–2042.


55. Javaheri S, Barbe F, Campos-Rodriguez F, et al. Sleep apnea: types, mechanisms, and clinical cardiovascular consequences.
J Am Coll Cardiol 2017;69:841–858.


56. Dewan NA, Nieto FJ, Somers VK. Intermittent hypoxemia and OSA: implications for comorbidities.
Chest 2015;147:266–274.



58. Sarzani R, Salvi F, Dessì-Fulgheri P, Rappelli A. Renin-angiotensin system, natriuretic peptides, obesity, metabolic syndrome, and hypertension: an integrated view in humans.
J Hypertens 2008;26:831–843.


59. Briones AM, Nguyen Dinh Cat A, Callera GE, et al. Adipocytes produce aldosterone through calcineurin-dependent signaling pathways: implications in diabetes mellitus-associated obesity and vascular dysfunction.
Hypertension 2012;59:1069–1078.


60. Dinh Cat AN, Friederich-Persson M, White A, Touyz RM. Adipocytes, aldosterone and obesity-related hypertension.
J Mol Endocrinol 2016;57:F7–F21.


61. Wang TJ, Larson MG, Levy D, et al. Impact of obesity on plasma natriuretic peptide levels.
Circulation 2004;109:594–600.


62. Packer M. Leptin-aldosterone-neprilysin axis: identification of its distinctive role in the pathogenesis of the three phenotypes of heart failure in people with obesity.
Circulation 2018;137:1614–1631.


63. Sharma K. The link between obesity and albuminuria: adiponectin and podocyte dysfunction.
Kidney Int 2009;76:145–148.


64. Engeli S, Feldpausch M, Gorzelniak K, et al. Association between adiponectin and mediators of inflammation in obese women.
Diabetes 2003;52:942–947.



65. Wiecek A, Kokot F, Chudek J, Adamczak M. The adipose tissue: a novel endocrine organ of interest to the nephrologist.
Nephrol Dial Transplant 2002;17:191–195.


66. Wolf G, Hamann A, Han DC, et al. Leptin stimulates proliferation and TGF-beta expression in renal glomerular endothelial cells: potential role in glomerulosclerosis [seecomments].
Kidney Int 1999;56:860–872.

67. Coimbra S, Rocha S, Valente MJ, et al. New insights into adiponectin and leptin roles in chronic kidney disease.
Biomedicines 2022;10:2642.



68. Zhao S, Kusminski CM, Scherer PE. Adiponectin, leptin and cardiovascular disorders.
Circ Res 2021;128:136–149.



69. Lim CC, Teo BW, Tai ES, et al. Elevated serum leptin, adiponectin and leptin to adiponectin ratio is associated with chronic kidney disease in Asian adults.
PLoS One 2015;10:e0122009.



70. Ambarkar M, Pemmaraju SV, Gouroju S, et al. Adipokines and their relation to endothelial dysfunction in patients with chronic kidney disease.
J Clin Diagn Res 2016;10:BC04–BC08.

71. Arabi T, Shafqat A, Sabbah BN, et al. Obesity-related kidney disease: beyond hypertension and insulin-resistance.
Front Endocrinol (Lausanne) 2023;13:1095211.



72. Schwenk RW, Vogel H, Schürmann A. Genetic and epigenetic control of metabolic health.
Mol Metab 2013;2:337–347.



73. Jun HJ, Kim J, Hoang MH, Lee SJ. Hepatic lipid accumulation alters global histone h3 lysine 9 and 4 trimethylation in the peroxisome proliferator-activated receptor alpha network.
PLoS One 2012;7:e44345.



74. Barrès R, Yan J, Egan B, et al. Acute exercise remodels promoter methylation in human skeletal muscle.
Cell Metab 2012;15:405–411.


75. Rönn T, Volkov P, Davegårdh C, et al. A six months exercise intervention influences the genome-wide DNA methylation pattern in human adipose tissue.
PLoS Genet 2013;9:e1003572.



77. Gadde KM, Martin CK, Berthoud HR, Heymsfield SB. Obesity: pathophysiology and management.
J Am Coll Cardiol 2018;71:69–84.


78. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society.
J Am Coll Cardiol 2014;63:2985–3023.

79. Juraschek SP, Miller ER 3rd, Weaver CM, Appel LJ. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure.
J Am Coll Cardiol 2017;70:2841–2848.



81. Gay HC, Rao SG, Vaccarino V, Ali MK. Effects of different dietary interventions on blood pressure: systematic review and meta-analysis of randomized controlled trials.
Hypertension 2016;67:733–739.


82. Swift DL, McGee JE, Earnest CP, Carlisle E, Nygard M, Johannsen NM. The effects of exercise and physical activity on weight loss and maintenance.
Prog Cardiovasc Dis 2018;61:206–213.


84. Noone C, Leahy J, Morrissey EC, et al. Comparative efficacy of exercise and anti-hypertensive pharmacological interventions in reducing blood pressure in people with hypertension: a network meta-analysis.
Eur J Prev Cardiol 2020;27:247–255.



85. Foster-Schubert KE, Alfano CM, Duggan CR, et al. Effect of diet and exercise, alone or combined, on weight and body composition in overweight-to-obese postmenopausal women.
Obesity (Silver Spring) 2012;20:1628–1638.



88. Jung MH, Shin ES, Ihm SH, Jung JG, Lee HY, Kim CH. The effect of alcohol dose on the development of hypertension in Asian and Western men: systematic review and meta-analysis.
Korean J Intern Med 2020;35:906–916.



91. Sharretts J, Galescu O, Gomatam S, Andraca-Carrera E, Hampp C, Yanoff L. Cancer risk associated with lorcaserin: the FDA’s review of the CAMELLIA-TIMI 61 Trial.
N Engl J Med 2020;383:1000–1002.


93. Khera R, Murad MH, Chandar AK, et al. Association of pharmacological treatments for obesity with weight loss and adverse events: a systematic review and meta-analysis.
JAMA 2016;315:2424–2434.



96. Wilding JP, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity.
N Engl J Med 2021;384:989–1002.


97. Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases.
Kidney Int 2021;100:S1–S276.

98. Lee H, Kwon SH, Jeon JS, Noh H, Han DC, Kim H. Association between blood pressure and the risk of chronic kidney disease in treatment-naïve hypertensive patients.
Kidney Res Clin Pract 2022;41:31–42.










 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















