1. Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2017 annual data report: epidemiology of kidney disease in the United States.
Am J Kidney Dis 2018;71:A7.


2. Eknoyan G, Beck GJ, Cheung AK, et al. Effect of dialysis dose and membrane flux in maintenance hemodialysis.
N Engl J Med 2002;347:2010ŌĆō2019.


3. Tattersall JE, Ward RA; EUDIAL group. Online haemodiafiltration: definition, dose quantification and safety revisited.
Nephrol Dial Transplant 2013;28:542ŌĆō550.


4. Akizawa T, Koiwa F. Clinical expectation of online hemodiafiltration: a Japanese perspective.
Blood Purif 2015;40 Suppl 1:12ŌĆō16.



5. Schmid H, Schiffl H. Hemodiafiltration and survival of end-stage renal disease patients: the long journey goes on.
Int Urol Nephrol 2012;44:1435ŌĆō1440.



6. Ok E, Asci G, Toz H, et al. Mortality and cardiovascular events in online haemodiafiltration (OL-HDF) compared with high-flux dialysis: results from the Turkish OL-HDF Study.
Nephrol Dial Transplant 2013;28:192ŌĆō202.


7. Nub├® MJ, Peters SA, Blankestijn PJ, et al. Mortality reduction by post-dilution online-haemodiafiltration: a cause-specific analysis.
Nephrol Dial Transplant 2017;32:548ŌĆō555.

8. Morena M, Jaussent A, Chalabi L, et al. Treatment tolerance and patient-reported outcomes favor online hemodiafiltration compared to high-flux hemodialysis in the elderly.
Kidney Int 2017;91:1495ŌĆō1509.


9. Grooteman MP, van den Dorpel MA, Bots ML, et al. Effect of online hemodiafiltration on all-cause mortality and cardiovascular outcomes.
J Am Soc Nephrol 2012;23:1087ŌĆō1096.



10. Peters SA, Bots ML, Canaud B, et al. Haemodiafiltration and mortality in end-stage kidney disease patients: a pooled individual participant data analysis from four randomized controlled trials.
Nephrol Dial Transplant 2016;31:978ŌĆō984.


11. Kim DH, Lee YK, Park HC, et al. Stepwise achievement of high convection volume in post-dilution hemodiafiltration: a prospective observational study.
Semin Dial 2021;34:368ŌĆō374.



12. Marticorena RM, Hunter J, Cook R, et al. A simple method to create buttonhole cannulation tracks in a busy hemodialysis unit.
Hemodial Int 2009;13:316ŌĆō321.


13. Atkar RK, MacRae JM. The buttonhole technique for fistula cannulation: pros and cons.
Curr Opin Nephrol Hypertens 2013;22:629ŌĆō636.

14. van Loon M. How to improve vascular access care.
Contrib Nephrol 2015;184:222ŌĆō233.

15. Ball LK. The buttonhole technique for arteriovenous fistula cannulation.
Nephrol Nurs J 2006;33:299ŌĆō304.

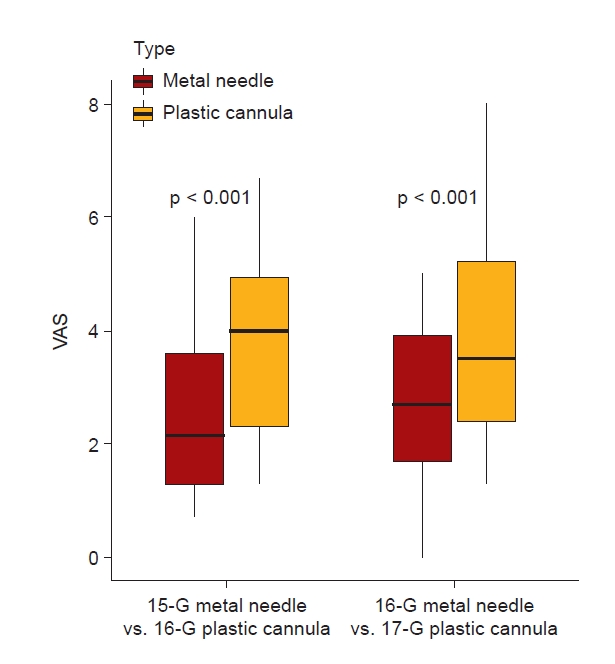
16. Choi YS, Lee HS, Joo N, et al. Efficacy and safety of plastic cannulae compared with metal needles in the initial use of an arteriovenous fistulae in incident hemodialysis patients: a randomized controlled study.
Am J Nephrol 2021;52:479ŌĆō486.



17. Smith V, Schoch M. Plastic cannula use in hemodialysis access.
J Vasc Access 2016;17:405ŌĆō410.



18. Nalesso F, Garzotto F, Muraro E, Brendolan A, Ronco C. Fistula cannulation with a novel fistula cannula: a review of cannulation devices and procedures.
Blood Purif 2018;45:278ŌĆō283.



19. Parisotto MT, Schoder VU, Miriunis C, et al. Cannulation technique influences arteriovenous fistula and graft survival.
Kidney Int 2014;86:790ŌĆō797.



21. Schiffl H. Online hemodiafiltration and mortality risk in end-stage renal disease patients: a critical appraisal of current evidence.
Kidney Res Clin Pract 2019;38:159ŌĆō168.



22. National Kidney Foundation. KDOQI clinical practice guideline for hemodialysis adequacy: 2015 update.
Am J Kidney Dis 2015;66:884ŌĆō930.

23. Bergstr├Čm J, Wehle B. No change in corrected beta 2-microglobulin concentration after cuprophane haemodialysis.
Lancet 1987;1:628ŌĆō629.

24. de Roij van Zuijdewijn CL, Chapdelaine I, Nub├® MJ, et al. Achieving high convection volumes in postdilution online hemodiafiltration: a prospective multicenter study.
Clin Kidney J 2017;10:804ŌĆō812.



25. Delgado DA, Lambert BS, Boutris N, et al. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults.
J Am Acad Orthop Surg Glob Res Rev 2018;2:e088.



26. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain.
Int J Rehabil Res 2008;31:165ŌĆō169.


27. Penne EL, van der Weerd NC, Bots ML, et al. Patient- and treatment-related determinants of convective volume in post-dilution haemodiafiltration in clinical practice.
Nephrol Dial Transplant 2009;24:3493ŌĆō3499.


28. Chapdelaine I, de Roij van Zuijdewijn CL, Mostovaya IM, et al. Optimization of the convection volume in online post-dilution haemodiafiltration: practical and technical issues.
Clin Kidney J 2015;8:191ŌĆō198.



29. Tordoir J, Canaud B, Haage P, et al. EBPG on vascular access.
Nephrol Dial Transplant 2007;22 Suppl 2:ii88ŌĆōii117.


30. Parisotto MT, Pelliccia F, Bedenbender-Stoll E, Gallieni M. Haemodialysis plastic cannulae: a possible alternative to traditional metal needles?
J Vasc Access 2016;17:373ŌĆō379.



31. Shi K, Jiang H, Wakabayashi M. Effect of early cannulation with plastic cannula on arteriovenous fistula patency in hemodialysis patients.
Blood Purif 2020;49:79ŌĆō84.



32. Kikuchi K, Hamano T, Wada A, Nakai S, Masakane I. Predilution online hemodiafiltration is associated with improved survival compared with hemodialysis.
Kidney Int 2019;95:929ŌĆō938.


33. Mercadal L, Franck JE, Metzger M, Urena Torres P, de Cornelissen F, Edet S, et al. Hemodiafiltration versus hemodialysis and survival in patients with ESRD: te French Renal Epidemiology and Information Network (REIN) registry.
Am J Kidney Dis 2016;68:247ŌĆō255.

34. Susantitaphong P, Siribamrungwong M, Jaber BL. Convective therapies versus low-flux hemodialysis for chronic kidney failure: a meta-analysis of randomized controlled trials.
Nephrol Dial Transplant 2013;28:2859ŌĆō2874.


35. Mostovaya IM, Blankestijn PJ, Bots ML, et al. Clinical evidence on hemodiafiltration: a systematic review and a meta-analysis.
Semin Dial 2014;27:119ŌĆō127.


37. Marticorena RM, Donnelly SM. Impact of needles in vascular access for hemodialysis.
J Vasc Access 2016;17 Suppl 1:S32ŌĆōS37.



38. Leblanc M, Bosc JY, Vaussenat F, Maurice F, Leray-Moragues H, Canaud B. Effective blood flow and recirculation rates in internal jugular vein twin catheters: measurement by ultrasound velocity dilution.
Am J Kidney Dis 1998;31:87ŌĆō92.


39. Canaud B, Leray-Moragues H, Kerkeni N, Bosc JY, Martin K. Effective flow performances and dialysis doses delivered with permanent catheters: a 24-month comparative study of permanent catheters versus arterio-venous vascular accesses.
Nephrol Dial Transplant 2002;17:1286ŌĆō1292.


40. Masakane I, Sakurai K. Current approaches to middle molecule removal: room for innovation.
Nephrol Dial Transplant 2018;33:iii12ŌĆōiii21.






















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















