1. Romagnani P, Remuzzi G, Glassock R, et al. Chronic kidney disease.
Nat Rev Dis Primers 2017;3:17088.



2. de Cos M, Xipell M, García-Herrera A, et al. Assessing and counteracting fibrosis is a cornerstone of the treatment of CKD secondary to systemic and renal limited autoimmune disorders.
Autoimmun Rev 2022;21:103014.


3. Zatz R, Meyer TW, Rennke HG, Brenner BM. Predominance of hemodynamic rather than metabolic factors in the pathogenesis of diabetic glomerulopathy.
Proc Natl Acad Sci U S A 1985;82:5963–5967.



4. Foresto-Neto O, Albino AH, Arias SC, et al. NF-κB system is chronically activated and promotes glomerular injury in experimental type 1 diabetic kidney disease.
Front Physiol 2020;11:84.



5. Andrade-Oliveira V, Foresto-Neto O, Watanabe IK, Zatz R, Câmara NO. Inflammation in renal diseases: new and old players.
Front Pharmacol 2019;10:1192.



6. DeFronzo RA, Alvestrand A, Smith D, Hendler R, Hendler E, Wahren J. Insulin resistance in uremia.
J Clin Invest 1981;67:563–568.



7. Basso PJ, Andrade-Oliveira V, Câmara NO. Targeting immune cell metabolism in kidney diseases.
Nat Rev Nephrol 2021;17:465–480.



8. Legouis D, Ricksten SE, Faivre A, et al. Altered proximal tubular cell glucose metabolism during acute kidney injury is associated with mortality.
Nat Metab 2020;2:732–743.



9. Mayrhofer C, Krieger S, Huttary N, et al. Alterations in fatty acid utilization and an impaired antioxidant defense mechanism are early events in podocyte injury: a proteomic analysis.
Am J Pathol 2009;174:1191–1202.


10. Giardino L, Armelloni S, Corbelli A, et al. Podocyte glutamatergic signaling contributes to the function of the glomerular filtration barrier.
J Am Soc Nephrol 2009;20:1929–1940.



11. Zhu C, Huang S, Yuan Y, et al. Mitochondrial dysfunction mediates aldosterone-induced podocyte damage: a therapeutic target of PPARγ.
Am J Pathol 2011;178:2020–2031.


12. Müller-Deile J, Schiffer M. The podocyte power-plant disaster and its contribution to glomerulopathy.
Front Endocrinol (Lausanne) 2014;5:209.


13. Stieger N, Worthmann K, Teng B, et al. Impact of high glucose and transforming growth factor-β on bioenergetic profiles in podocytes.
Metabolism 2012;61:1073–1086.


14. Daehn I, Casalena G, Zhang T, et al. Endothelial mitochondrial oxidative stress determines podocyte depletion in segmental glomerulosclerosis.
J Clin Invest 2014;124:1608–1621.



15. Kriz W, Hosser H, Hähnel B, Gretz N, Provoost AP. From segmental glomerulosclerosis to total nephron degeneration and interstitial fibrosis: a histopathological study in rat models and human glomerulopathies.
Nephrol Dial Transplant 1998;13:2781–2798.


17. Liu Y. Renal fibrosis: new insights into the pathogenesis and therapeutics.
Kidney Int 2006;69:213–217.


18. Kang HM, Ahn SH, Choi P, et al. Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development.
Nat Med 2015;21:37–46.



19. Han SH, Malaga-Dieguez L, Chinga F, et al. Deletion of Lkb1 in renal tubular epithelial cells leads to CKD by altering metabolism.
J Am Soc Nephrol 2016;27:439–453.


20. DeBerardinis RJ, Thompson CB. Cellular metabolism and disease: what do metabolic outliers teach us?
Cell 2012;148:1132–1144.



21. Li C, Ding XY, Xiang DM, et al. Enhanced M1 and impaired M2 macrophage polarization and reduced mitochondrial biogenesis via inhibition of AMP kinase in chronic kidney disease.
Cell Physiol Biochem 2015;36:358–372.



22. Andris F, Leo O. AMPK in lymphocyte metabolism and function.
Int Rev Immunol 2015;34:67–81.


23. Dengler VL, Galbraith M, Espinosa JM. Transcriptional regulation by hypoxia inducible factors.
Crit Rev Biochem Mol Biol 2014;49:1–15.


24. Lee JW, Bae SH, Jeong JW, Kim SH, Kim KW. Hypoxia-inducible factor (HIF-1)alpha: its protein stability and biological functions.
Exp Mol Med 2004;36:1–12.



25. Gunaratnam L, Bonventre JV. HIF in kidney disease and development.
J Am Soc Nephrol 2009;20:1877–1887.


27. Haase VH. Hypoxic regulation of erythropoiesis and iron metabolism.
Am J Physiol Renal Physiol 2010;299:F1–F13.



28. Pugh CW, O’Rourke JF, Nagao M, Gleadle JM, Ratcliffe PJ. Activation of hypoxia-inducible factor-1; definition of regulatory domains within the alpha subunit.
J Biol Chem 1997;272:11205–11214.

29. O’Rourke JF, Tian YM, Ratcliffe PJ, Pugh CW. Oxygen-regulated and transactivating domains in endothelial PAS protein 1: comparison with hypoxia-inducible factor-1alpha.
J Biol Chem 1999;274:2060–2071.

31. Befani C, Liakos P. The role of hypoxia-inducible factor-2 alpha in angiogenesis.
J Cell Physiol 2018;233:9087–9098.



33. Hu CJ, Wang LY, Chodosh LA, Keith B, Simon MC. Differential roles of hypoxia-inducible factor 1alpha (HIF-1alpha) and HIF-2alpha in hypoxic gene regulation.
Mol Cell Biol 2003;23:9361–9374.


34. Elvert G, Kappel A, Heidenreich R, et al. Cooperative interaction of hypoxia-inducible factor-2alpha (HIF-2alpha) and Ets-1 in the transcriptional activation of vascular endothelial growth factor receptor-2 (Flk-1).
J Biol Chem 2003;278:7520–7530.

35. Yang SL, Wu C, Xiong ZF, Fang X. Progress on hypoxia-inducible factor-3: its structure, gene regulation and biological function (Review).
Mol Med Rep 2015;12:2411–2416.


36. Huang LE, Gu J, Schau M, Bunn HF. Regulation of hypoxia-inducible factor 1alpha is mediated by an O2-dependent degradation domain via the ubiquitin-proteasome pathway.
Proc Natl Acad Sci U S A 1998;95:7987–7992.


37. Strowitzki MJ, Cummins EP, Taylor CT. Protein hydroxylation by hypoxia-inducible factor (HIF) hydroxylases: unique or ubiquitous?
Cells 2019;8:384.



38. Chen R, Lai UH, Zhu L, Singh A, Ahmed M, Forsyth NR. Reactive oxygen species formation in the brain at different oxygen levels: the role of hypoxia inducible factors.
Front Cell Dev Biol 2018;6:132.



39. Singhal R, Shah YM. Oxygen battle in the gut: hypoxia and hypoxia-inducible factors in metabolic and inflammatory responses in the intestine.
J Biol Chem 2020;295:10493–10505.



40. Koh MY, Powis G. HAF : the new player in oxygen-independent HIF-1alpha degradation.
Cell Cycle 2009;8:1359–1366.


41. Hansell P, Welch WJ, Blantz RC, Palm F. Determinants of kidney oxygen consumption and their relationship to tissue oxygen tension in diabetes and hypertension.
Clin Exp Pharmacol Physiol 2013;40:123–137.



42. Eckardt KU, Bernhardt WM, Weidemann A, et al. Role of hypoxia in the pathogenesis of renal disease.
Kidney Int Suppl 2005;(99):S46–S51.



43. Evans RG, Smith DW, Lee CJ, Ngo JP, Gardiner BS. What makes the kidney susceptible to hypoxia?
Anat Rec (Hoboken) 2020;303:2544–2552.



44. Mayer G. Capillary rarefaction, hypoxia, VEGF and angiogenesis in chronic renal disease.
Nephrol Dial Transplant 2011;26:1132–1137.



46. Agarwal A, Nick HS. Renal response to tissue injury: lessons from heme oxygenase-1 GeneAblation and expression.
J Am Soc Nephrol 2000;11:965–973.

47. Warnecke C, Zaborowska Z, Kurreck J, et al. Differentiating the functional role of hypoxia-inducible factor (HIF)-1alpha and HIF-2alpha (EPAS-1) by the use of RNA interference: erythropoietin is a HIF-2alpha target gene in Hep3B and Kelly cells.
FASEB J 2004;18:1462–1464.



49. Kim JW, Tchernyshyov I, Semenza GL, Dang CV. HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia.
Cell Metab 2006;3:177–185.


50. Samanta D, Semenza GL. Metabolic adaptation of cancer and immune cells mediated by hypoxia-inducible factors.
Biochim Biophys Acta Rev Cancer 2018;1870:15–22.


51. Iyer NV, Kotch LE, Agani F, et al. Cellular and developmental control of O2 homeostasis by hypoxia-inducible factor 1 alpha.
Genes Dev 1998;12:149–162.



52. Huang D, Li T, Li X, et al. HIF-1-mediated suppression of acyl-CoA dehydrogenases and fatty acid oxidation is critical for cancer progression.
Cell Rep 2014;8:1930–1942.


54. Schaub JA, Venkatachalam MA, Weinberg JM. Proximal tubular oxidative metabolism in acute kidney injury and the transition to CKD.
Kidney360 2020;2:355–364.



55. Sugahara M, Tanaka T, Nangaku M. Hypoxia-inducible factor and oxygen biology in the kidney.
Kidney360 2020;1:1021–1031.



56. Freeburg PB, Robert B, St John PL, Abrahamson DR. Podocyte expression of hypoxia-inducible factor (HIF)-1 and HIF-2 during glomerular development.
J Am Soc Nephrol 2003;14:927–938.


57. Fu J, Shinjo T, Li Q, et al. Regeneration of glomerular metabolism and function by podocyte pyruvate kinase M2 in diabetic nephropathy.
JCI Insight 2022;7:e155260.



58. Semenza GL. Hypoxia-inducible factors in physiology and medicine.
Cell 2012;148:399–408.



59. Haase VH. Regulation of erythropoiesis by hypoxia-inducible factors.
Blood Rev 2013;27:41–53.



60. Rosenberger C, Mandriota S, Jürgensen JS, et al. Expression of hypoxia-inducible factor-1alpha and -2alpha in hypoxic and ischemic rat kidneys.
J Am Soc Nephrol 2002;13:1721–1732.

61. Li H, Satriano J, Thomas JL, et al. Interactions between HIF-1α and AMPK in the regulation of cellular hypoxia adaptation in chronic kidney disease.
Am J Physiol Renal Physiol 2015;309:F414–F428.



62. Wang Z, Zhu Q, Li PL, et al. Silencing of hypoxia-inducible factor-1α gene attenuates chronic ischemic renal injury in two-kidney, one-clip rats.
Am J Physiol Renal Physiol 2014;306:F1236–F1242.



63. Fang Y, Yu X, Liu Y, et al. miR-29c is downregulated in renal interstitial fibrosis in humans and rats and restored by HIF-α activation.
Am J Physiol Renal Physiol 2013;304:F1274–F1282.



64. Higgins DF, Kimura K, Bernhardt WM, et al. Hypoxia promotes fibrogenesis in vivo via HIF-1 stimulation of epithelial-to-mesenchymal transition.
J Clin Invest 2007;117:3810–3820.



65. Kimura K, Iwano M, Higgins DF, et al. Stable expression of HIF-1alpha in tubular epithelial cells promotes interstitial fibrosis.
Am J Physiol Renal Physiol 2008;295:F1023–F1029.


67. Zhu Q, Wang Z, Xia M, et al. Silencing of hypoxia-inducible factor-1α gene attenuated angiotensin II-induced renal injury in Sprague-Dawley rats.
Hypertension 2011;58:657–664.


68. Baumann B, Hayashida T, Liang X, Schnaper HW. Hypoxia-inducible factor-1α promotes glomerulosclerosis and regulates COL1A2 expression through interactions with Smad3.
Kidney Int 2016;90:797–808.



69. Zhao H, Jiang N, Han Y, et al. Aristolochic acid induces renal fibrosis by arresting proximal tubular cells in G2/M phase mediated by HIF-1α.
FASEB J 2020;34:12599–12614.



70. Kobayashi H, Gilbert V, Liu Q, et al. Myeloid cell-derived hypoxia-inducible factor attenuates inflammation in unilateral ureteral obstruction-induced kidney injury.
J Immunol 2012;188:5106–5115.



71. Bernhardt WM, Câmpean V, Kany S, et al. Preconditional activation of hypoxia-inducible factors ameliorates ischemic acute renal failure.
J Am Soc Nephrol 2006;17:1970–1978.


72. Ito M, Tanaka T, Ishii T, Wakashima T, Fukui K, Nangaku M. Prolyl hydroxylase inhibition protects the kidneys from ischemia via upregulation of glycogen storage.
Kidney Int 2020;97:687–701.


73. Yang Y, Yu X, Zhang Y, et al. Hypoxia-inducible factor prolyl hydroxylase inhibitor roxadustat (FG-4592) protects against cisplatin-induced acute kidney injury.
Clin Sci (Lond) 2018;132:825–838.



74. Schley G, Klanke B, Kalucka J, et al. Mononuclear phagocytes orchestrate prolyl hydroxylase inhibition-mediated renoprotection in chronic tubulointerstitial nephritis.
Kidney Int 2019;96:378–396.


75. Kabei K, Tateishi Y, Shiota M, et al. Effects of orally active hypoxia inducible factor alpha prolyl hydroxylase inhibitor, FG4592 on renal fibrogenic potential in mouse unilateral ureteral obstruction model.
J Pharmacol Sci 2020;142:93–100.


76. Ganz T, Nemeth E. Iron balance and the role of hepcidin in chronic kidney disease.
Semin Nephrol 2016;36:87–93.



77. Provenzano R, Besarab A, Sun CH, et al. Oral hypoxia-inducible factor prolyl hydroxylase inhibitor roxadustat (FG-4592) for the treatment of anemia in patients with CKD.
Clin J Am Soc Nephrol 2016;11:982–991.



78. Fishbane S, El-Shahawy MA, Pecoits-Filho R, et al. Roxadustat for treating anemia in patients with CKD not on dialysis: results from a randomized phase 3 study.
J Am Soc Nephrol 2021;32:737–755.



79. Besarab A, Chernyavskaya E, Motylev I, et al. Roxadustat (FG-4592): correction of anemia in incident dialysis patients.
J Am Soc Nephrol 2016;27:1225–1233.

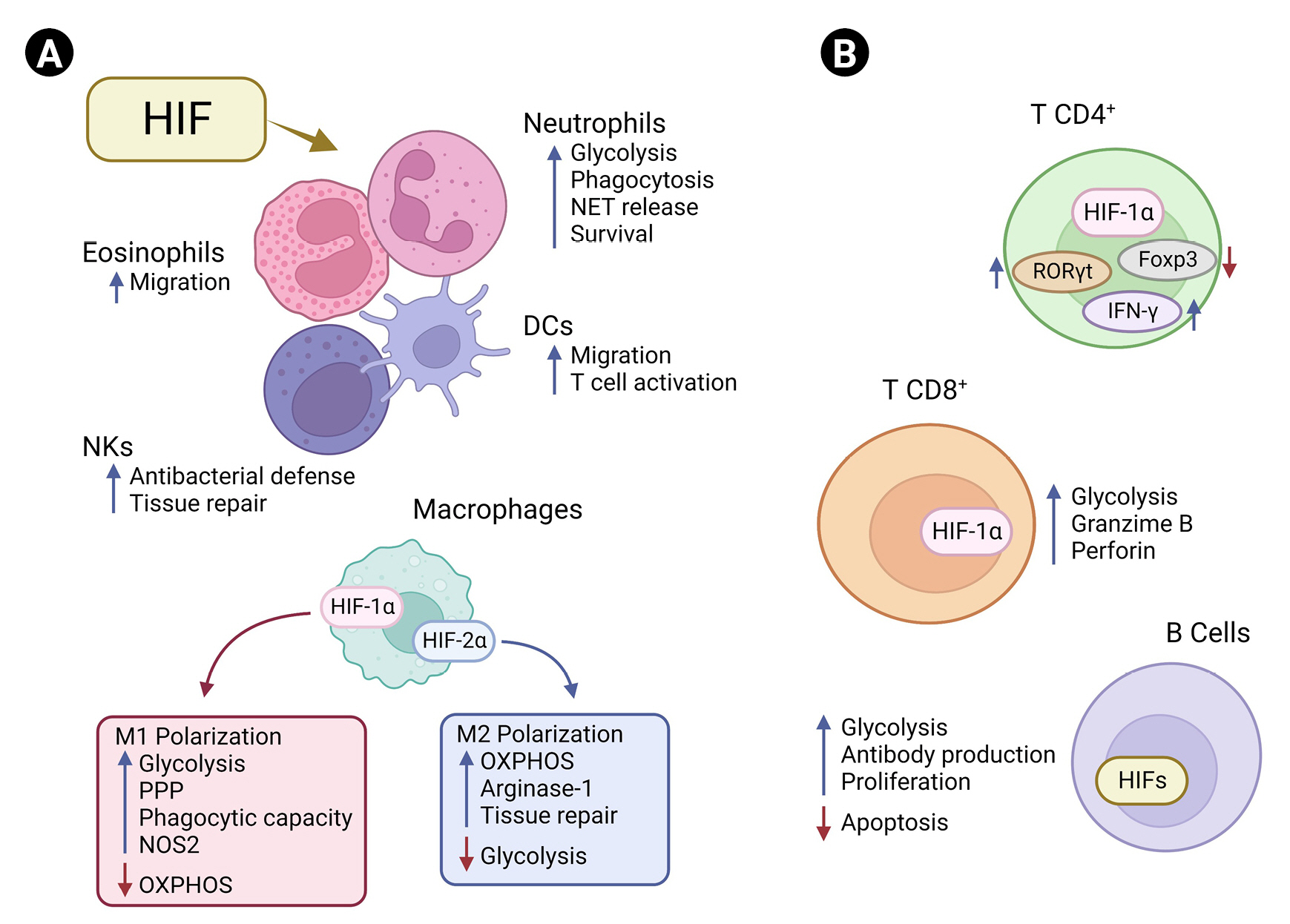
80. Chen Y, Gaber T. Hypoxia/HIF modulates immune responses.
Biomedicines 2021;9:260.



81. McGettrick AF, O’Neill LAJ. The role of HIF in immunity and inflammation.
Cell Metab 2020;32:524–536.


83. Jantsch J, Chakravortty D, Turza N, et al. Hypoxia and hypoxia-inducible factor-1 alpha modulate lipopolysaccharide-induced dendritic cell activation and function.
J Immunol 2008;180:4697–4705.

85. Crotty Alexander LE, Akong-Moore K, Feldstein S, et al. Myeloid cell HIF-1α regulates asthma airway resistance and eosinophil function.
J Mol Med (Berl) 2013;91:637–644.



87. Ortiz-Masià D, Díez I, Calatayud S, et al. Induction of CD36 and thrombospondin-1 in macrophages by hypoxia-inducible factor 1 and its relevance in the inflammatory process.
PLoS One 2012;7:e48535.



88. Tannahill GM, Curtis AM, Adamik J, et al. Succinate is an inflammatory signal that induces IL-1β through HIF-1α.
Nature 2013;496:238–242.


89. Selak MA, Armour SM, MacKenzie ED, et al. Succinate links TCA cycle dysfunction to oncogenesis by inhibiting HIF-alpha prolyl hydroxylase.
Cancer Cell 2005;7:77–85.


90. Mills EL, Kelly B, Logan A, et al. Succinate dehydrogenase supports metabolic repurposing of mitochondria to drive inflammatory macrophages.
Cell 2016;167:457–470.



91. Takeda N, O’Dea EL, Doedens A, et al. Differential activation and antagonistic function of HIF-{alpha} isoforms in macrophages are essential for NO homeostasis.
Genes Dev 2010;24:491–501.



92. Dehn S, DeBerge M, Yeap XY, et al. HIF-2α in resting macrophages tempers mitochondrial reactive oxygen species to selectively repress MARCO-dependent phagocytosis.
J Immunol 2016;197:3639–3649.



94. Abbott RK, Thayer M, Labuda J, et al. Germinal center hypoxia potentiates immunoglobulin class switch recombination.
J Immunol 2016;197:4014–4020.



95. Dang EV, Barbi J, Yang HY, et al. Control of T(H)17/T(reg) balance by hypoxia-inducible factor 1.
Cell 2011;146:772–784.



96. Harris TJ, Grosso JF, Yen HR, et al. Cutting edge: an in vivo requirement for STAT3 signaling in TH17 development and TH17-dependent autoimmunity.
J Immunol 2007;179:4313–4317.



97. Zhou L, Ivanov II, Spolski R, et al. IL-6 programs T(H)-17 cell differentiation by promoting sequential engagement of the IL-21 and IL-23 pathways.
Nat Immunol 2007;8:967–974.



98. Shehade H, Acolty V, Moser M, Oldenhove G. Cutting edge: hypoxia-inducible factor 1 negatively regulates Th1 function.
J Immunol 2015;195:1372–1376.



99. Peng M, Yin N, Chhangawala S, Xu K, Leslie CS, Li MO. Aerobic glycolysis promotes T helper 1 cell differentiation through an epigenetic mechanism.
Science 2016;354:481–484.



101. Li ZL, Ji JL, Wen Y, et al. HIF-1α is transcriptionally regulated by NF-κB in acute kidney injury.
Am J Physiol Renal Physiol 2021;321:F225–F235.


102. Yamaguchi J, Tanaka T, Eto N, Nangaku M. Inflammation and hypoxia linked to renal injury by CCAAT/enhancer-binding protein δ.
Kidney Int 2015;88:262–275.



104. Huang X, He Z, Jiang X, et al. Folic acid represses hypoxia-induced inflammation in THP-1 cells through inhibition of the PI3K/Akt/HIF-1α pathway.
PLoS One 2016;11:e0151553.



105. Xu EY, Perlina A, Vu H, et al. Integrated pathway analysis of rat urine metabolic profiles and kidney transcriptomic profiles to elucidate the systems toxicology of model nephrotoxicants.
Chem Res Toxicol 2008;21:1548–1561.


106. Ahn JM, You SJ, Lee YM, et al. Hypoxia-inducible factor activation protects the kidney from gentamicin-induced acute injury.
PLoS One 2012;7:e48952.



107. Sharp CN, Doll M, Dupre TV, Beverly LJ, Siskind LJ. Moderate aging does not exacerbate cisplatin-induced kidney injury or fibrosis despite altered inflammatory cytokine expression and immune cell infiltration.
Am J Physiol Renal Physiol 2019;316:F162–F172.


108. Sears SM, Vega AA, Kurlawala Z, et al. F4/80hi resident macrophages contribute to cisplatin-induced renal fibrosis.
Kidney360 2022;3:818–833.



109. Liu H, Li Y, Xiong J. The role of hypoxia-inducible factor-1 alpha in renal disease.
Molecules 2022;27:7318.



111. Rempel LC, Faustino VD, Foresto-Neto O, et al. Chronic exposure to hypoxia attenuates renal injury and innate immunity activation in the remnant kidney model.
Am J Physiol Renal Physiol 2019;317:F1285–F1292.


112. Xie D, Zhao H, Xu X, et al. Intensity of macrophage infiltration in glomeruli predicts response to immunosuppressive therapy in patients with IgA nephropathy.
J Am Soc Nephrol 2021;32:3187–3196.



113. Caliskan Y, Demir E, Karatay E, et al. Oxidative stress and macrophage infiltration in IgA nephropathy.
J Nephrol 2022;35:1101–1111.



114. Silva GE, Costa RS, Ravinal RC, et al. Renal macrophage infiltration is associated with a poor outcome in IgA nephropathy.
Clinics (Sao Paulo) 2012;67:697–703.



115. Hung TW, Liou JH, Yeh KT, et al. Renal expression of hypoxia inducible factor-1α in patients with chronic kidney disease: a clinicopathologic study from nephrectomized kidneys.
Indian J Med Res 2013;137:102–110.


116. Knutson AK, Williams AL, Boisvert WA, Shohet RV. HIF in the heart: development, metabolism, ischemia, and atherosclerosis.
J Clin Invest 2021;131:e137557.



117. Bertorello AM, Sznajder JI. The dopamine paradox in lung and kidney epithelia: sharing the same target but operating different signaling networks.
Am J Respir Cell Mol Biol 2005;33:432–437.



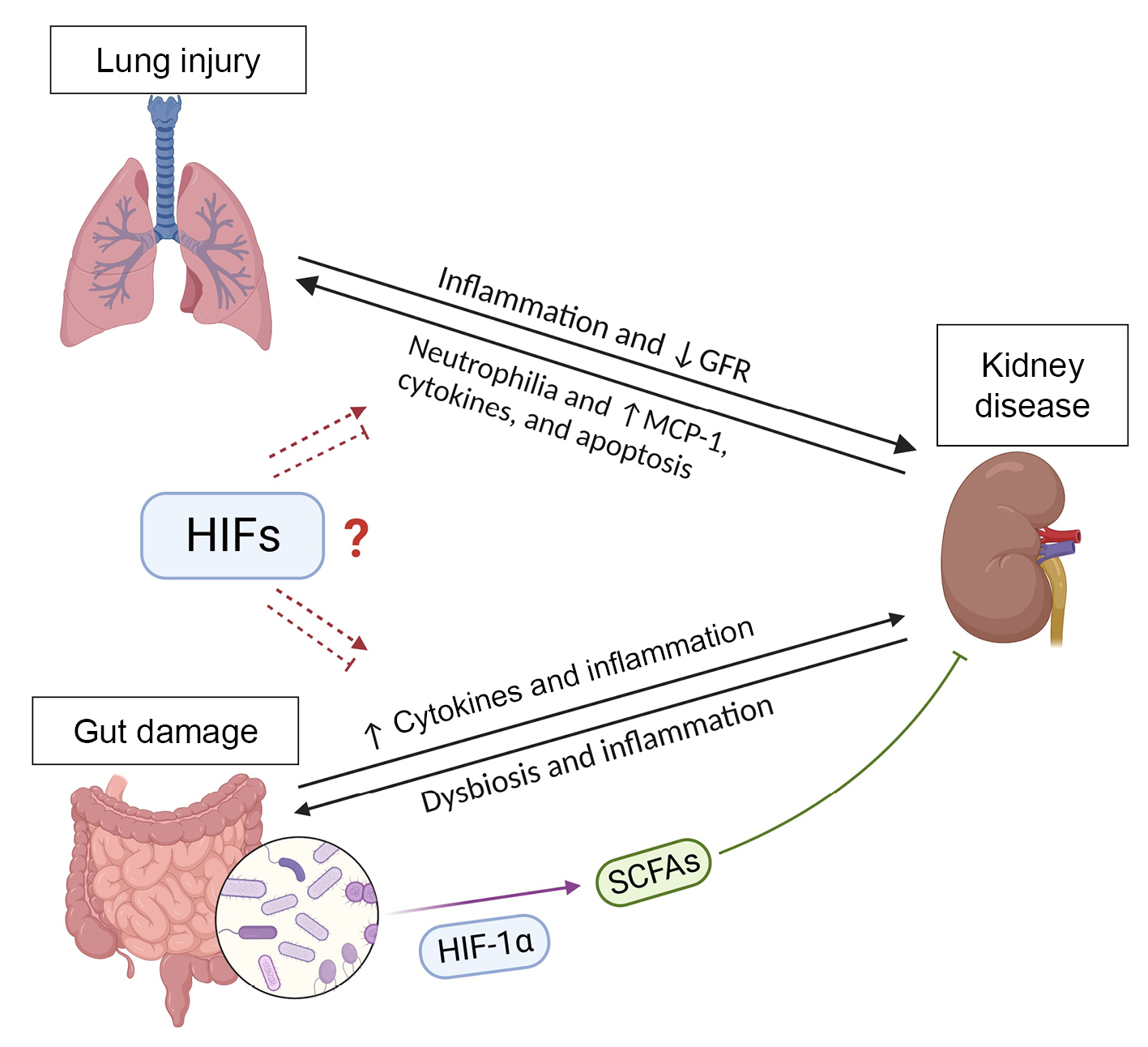
118. Domenech P, Perez T, Saldarini A, Uad P, Musso CG. Kidney-lung pathophysiological crosstalk: its characteristics and importance.
Int Urol Nephrol 2017;49:1211–1215.



119. Husain-Syed F, Slutsky AS, Ronco C. Lung-kidney cross-talk in the critically ill patient.
Am J Respir Crit Care Med 2016;194:402–414.


121. Jandl K, Mutgan AC, Eller K, Schaefer L, Kwapiszewska G. The basement membrane in the cross-roads between the lung and kidney.
Matrix Biol 2022;105:31–52.


122. Vohwinkel CU, Hoegl S, Eltzschig HK. Hypoxia signaling during acute lung injury.
J Appl Physiol (1985) 2015;119:1157–1163.



123. Vadivel A, Alphonse RS, Etches N, et al. Hypoxia-inducible factors promote alveolar development and regeneration.
Am J Respir Cell Mol Biol 2014;50:96–105.


124. van Tuyl M, Liu J, Wang J, Kuliszewski M, Tibboel D, Post M. Role of oxygen and vascular development in epithelial branching morphogenesis of the developing mouse lung.
Am J Physiol Lung Cell Mol Physiol 2005;288:L167–L178.


125. Tibboel J, Groenman FA, Selvaratnam J, et al. Hypoxia-inducible factor-1 stimulates postnatal lung development but does not prevent O2-induced alveolar injury.
Am J Respir Cell Mol Biol 2015;52:448–458.


126. Huang Y, Kempen MB, Munck AB, et al. Hypoxia-inducible factor 2α plays a critical role in the formation of alveoli and surfactant.
Am J Respir Cell Mol Biol 2012;46:224–232.


127. Yamashita T, Ohneda O, Nagano M, et al. Abnormal heart development and lung remodeling in mice lacking the hypoxia-inducible factor-related basic helix-loop-helix PAS protein NEPAS.
Mol Cell Biol 2008;28:1285–1297.



128. Corrado C, Fontana S. Hypoxia and HIF signaling: one axis with divergent effects.
Int J Mol Sci 2020;21:5611.



129. Lee JW, Ko J, Ju C, Eltzschig HK. Hypoxia signaling in human diseases and therapeutic targets.
Exp Mol Med 2019;51:1–13.


130. Carpenter TC, Stenmark KR. Hypoxia decreases lung neprilysin expression and increases pulmonary vascular leak.
Am J Physiol Lung Cell Mol Physiol 2001;281:L941–L948.


131. Madjdpour C, Jewell UR, Kneller S, et al. Decreased alveolar oxygen induces lung inflammation.
Am J Physiol Lung Cell Mol Physiol 2003;284:L360–L367.


132. Wiesener MS, Jürgensen JS, Rosenberger C, et al. Widespread hypoxia-inducible expression of HIF-2alpha in distinct cell populations of different organs.
FASEB J 2003;17:271–273.



134. Thiel M, Chouker A, Ohta A, et al. Oxygenation inhibits the physiological tissue-protecting mechanism and thereby exacerbates acute inflammatory lung injury.
PLoS Biol 2005;3:e174.



135. Wu G, Xu G, Chen DW, et al. Hypoxia exacerbates inflammatory acute lung injury via the toll-like receptor 4 signaling pathway.
Front Immunol 2018;9:1667.



136. Tang M, Tian Y, Li D, et al. TNF-α mediated increase of HIF-1α inhibits VASP expression, which reduces alveolar-capillary barrier function during acute lung injury (ALI).
PLoS One 2014;9:e102967.



137. Tojo K, Tamada N, Nagamine Y, Yazawa T, Ota S, Goto T. Enhancement of glycolysis by inhibition of oxygen-sensing prolyl hydroxylases protects alveolar epithelial cells from acute lung injury.
FASEB J 2018;32:2258–2268.



138. Woods PS, Kimmig LM, Sun KA, et al. HIF-1α induces glycolytic reprograming in tissue-resident alveolar macrophages to promote cell survival during acute lung injury.
Elife 2022;11:e77457.


139. Goodwin J, Choi H, Hsieh MH, et al. Targeting hypoxia-inducible factor-1α/pyruvate dehydrogenase kinase 1 axis by dichloroacetate suppresses bleomycin-induced pulmonary fibrosis.
Am J Respir Cell Mol Biol 2018;58:216–231.



141. Yu H, Li Q, Kolosov VP, Perelman JM, Zhou X. Regulation of cigarette smoke-mediated mucin expression by hypoxia-inducible factor-1α via epidermal growth factor receptor-mediated signaling pathways.
J Appl Toxicol 2012;32:282–292.


143. Gjerde B, Bakke PS, Ueland T, Hardie JA, Eagan TM. The prevalence of undiagnosed renal failure in a cohort of COPD patients in western Norway.
Respir Med 2012;106:361–366.


144. Faubel S, Edelstein CL. Mechanisms and mediators of lung injury after acute kidney injury.
Nat Rev Nephrol 2016;12:48–60.



145. Basu RK, Donaworth E, Wheeler DS, Devarajan P, Wong HR. Antecedent acute kidney injury worsens subsequent endotoxin-induced lung inflammation in a two-hit mouse model.
Am J Physiol Renal Physiol 2011;301:F597–F604.


147. Shi J, Yu T, Song K, et al. Dexmedetomidine ameliorates endotoxin-induced acute lung injury in vivo and in vitro by preserving mitochondrial dynamic equilibrium through the HIF-1a/HO-1 signaling pathway.
Redox Biol 2021;41:101954.



148. Rossi M, Delbauve S, Roumeguère T, et al. HO-1 mitigates acute kidney injury and subsequent kidney-lung cross-talk.
Free Radic Res 2019;53:1035–1043.


150. Glover LE, Lee JS, Colgan SP. Oxygen metabolism and barrier regulation in the intestinal mucosa.
J Clin Invest 2016;126:3680–3688.



151. Foresto-Neto O, Ghirotto B, Câmara NO. Renal sensing of bacterial metabolites in the gut-kidney axis.
Kidney360 2021;2:1501–1509.



152. Pral LP, Fachi JL, Corrêa RO, Colonna M, Vinolo MA. Hypoxia and HIF-1 as key regulators of gut microbiota and host interactions.
Trends Immunol 2021;42:604–621.



154. Comerford KM, Wallace TJ, Karhausen J, Louis NA, Montalto MC, Colgan SP. Hypoxia-inducible factor-1-dependent regulation of the multidrug resistance (MDR1) gene.
Cancer Res 2002;62:3387–3394.

155. Karhausen J, Furuta GT, Tomaszewski JE, Johnson RS, Colgan SP, Haase VH. Epithelial hypoxia-inducible factor-1 is protective in murine experimental colitis.
J Clin Invest 2004;114:1098–1106.



156. Glover LE, Bowers BE, Saeedi B, et al. Control of creatine metabolism by HIF is an endogenous mechanism of barrier regulation in colitis.
Proc Natl Acad Sci U S A 2013;110:19820–19825.



157. Campbell EL, Bruyninckx WJ, Kelly CJ, et al. Transmigrating neutrophils shape the mucosal microenvironment through localized oxygen depletion to influence resolution of inflammation.
Immunity 2014;40:66–77.



158. Giatromanolaki A, Sivridis E, Maltezos E, et al. Hypoxia inducible factor 1alpha and 2alpha overexpression in inflammatory bowel disease.
J Clin Pathol 2003;56:209–213.


159. Robinson A, Keely S, Karhausen J, Gerich ME, Furuta GT, Colgan SP. Mucosal protection by hypoxia-inducible factor prolyl hydroxylase inhibition.
Gastroenterology 2008;134:145–155.


160. Tambuwala MM, Cummins EP, Lenihan CR, et al. Loss of prolyl hydroxylase-1 protects against colitis through reduced epithelial cell apoptosis and increased barrier function.
Gastroenterology 2010;139:2093–2101.


161. Keely S, Campbell EL, Baird AW, et al. Contribution of epithelial innate immunity to systemic protection afforded by prolyl hydroxylase inhibition in murine colitis.
Mucosal Immunol 2014;7:114–123.



162. Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar Reddy D. Role of the normal gut microbiota.
World J Gastroenterol 2015;21:8787–8803.



163. Thorburn AN, Macia L, Mackay CR. Diet, metabolites, and “western-lifestyle” inflammatory diseases.
Immunity 2014;40:833–842.


164. Li F, Wang M, Wang J, Li R, Zhang Y. Alterations to the gut microbiota and their correlation with inflammatory factors in chronic kidney disease.
Front Cell Infect Microbiol 2019;9:206.



165. Raj D, Tomar B, Lahiri A, Mulay SR. The gut-liver-kidney axis: novel regulator of fatty liver associated chronic kidney disease.
Pharmacol Res 2020;152:104617.


166. Parada Venegas D, De la Fuente MK, Landskron G, et al. Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases.
Front Immunol 2019;10:277.


168. Liu L, Xu W, Kong P, Dou Y. The relationships among gut microbiota, hypoxia-inducible factor and anaemia with chronic kidney disease.
Nephrology (Carlton) 2022;27:851–858.



169. Zhou C, Li L, Li T, et al. SCFAs induce autophagy in intestinal epithelial cells and relieve colitis by stabilizing HIF-1α.
J Mol Med (Berl) 2020;98:1189–1202.



170. Fachi JL, Felipe JS, Pral LP, et al. Butyrate protects mice from Clostridium difficile-induced colitis through an HIF-1-dependent mechanism.
Cell Rep 2019;27:750–761.


171. Yin J, Zhou C, Yang K, et al. Mutual regulation between butyrate and hypoxia-inducible factor-1α in epithelial cell promotes expression of tight junction proteins.
Cell Biol Int 2020;44:1405–1414.



172. Kelly CJ, Zheng L, Campbell EL, et al. Crosstalk between microbiota-derived short-chain fatty acids and intestinal epithelial HIF augments tissue barrier function.
Cell Host Microbe 2015;17:662–671.



173. Koury J, Deitch EA, Homma H, et al. Persistent HIF-1alpha activation in gut ischemia/reperfusion injury: potential role of bacteria and lipopolysaccharide.
Shock 2004;22:270–277.


174. Andrade-Oliveira V, Amano MT, Correa-Costa M, et al. Gut bacteria products prevent AKI induced by ischemia-reperfusion.
J Am Soc Nephrol 2015;26:1877–1888.



175. Plata C, Cruz C, Cervantes LG, Ramírez V. The gut microbiota and its relationship with chronic kidney disease.
Int Urol Nephrol 2019;51:2209–2226.



176. Watanabe IK, Andrade-Silva M, Foresto-Neto O, et al. Gut microbiota and intestinal epithelial Myd88 signaling are crucial for renal injury in UUO mice.
Front Immunol 2020;11:578623.












 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















