3. Bugnicourt JM, Godefroy O, Chillon JM, Choukroun G, Massy ZA. Cognitive disorders and dementia in CKD: the neglected kidney-brain axis.
J Am Soc Nephrol 2013;24:353–363.

4. Viggiano D, Wagner CA, Martino G, et al. Mechanisms of cognitive dysfunction in CKD.
Nat Rev Nephrol 2020;16:452–469.



5. Niwa T. Indoxyl sulfate is a nephro-vascular toxin.
J Ren Nutr 2010;20:S2–S6.


6. Schulman G, Berl T, Beck GJ, et al. Randomized placebo-controlled EPPIC trials of AST-120 in CKD.
J Am Soc Nephrol 2015;26:1732–1746.


7. Konishi K, Nakano S, Tsuda S, Nakagawa A, Kigoshi T, Koya D. AST-120 (Kremezin) initiated in early stage chronic kidney disease stunts the progression of renal dysfunction in type 2 diabetic subjects.
Diabetes Res Clin Pract 2008;81:310–315.


8. Yorioka N, Kiribayashi K, Naito T, et al. An oral adsorbent, AST-120, combined with a low-protein diet and RAS blocker, for chronic kidney disease.
J Nephrol 2008;21:213–220.

9. Su PY, Lee YH, Kuo LN, et al. Efficacy of AST-120 for patients with chronic kidney disease: a network meta-analysis of randomized controlled trials.
Front Pharmacol 2021;12:676345.



10. Adesso S, Magnus T, Cuzzocrea S, et al. Indoxyl sulfate affects glial function increasing oxidative stress and neuroinflammation in chronic kidney disease: interaction between astrocytes and microglia.
Front Pharmacol 2017;8:370.



12. Siracusa R, Fusco R, Cuzzocrea S. Astrocytes: role and functions in brain pathologies.
Front Pharmacol 2019;10:1114.



13. Shigetomi E, Saito K, Sano F, Koizumi S. Aberrant calcium signals in reactive astrocytes: a key process in neurological disorders.
Int J Mol Sci 2019;20:996.



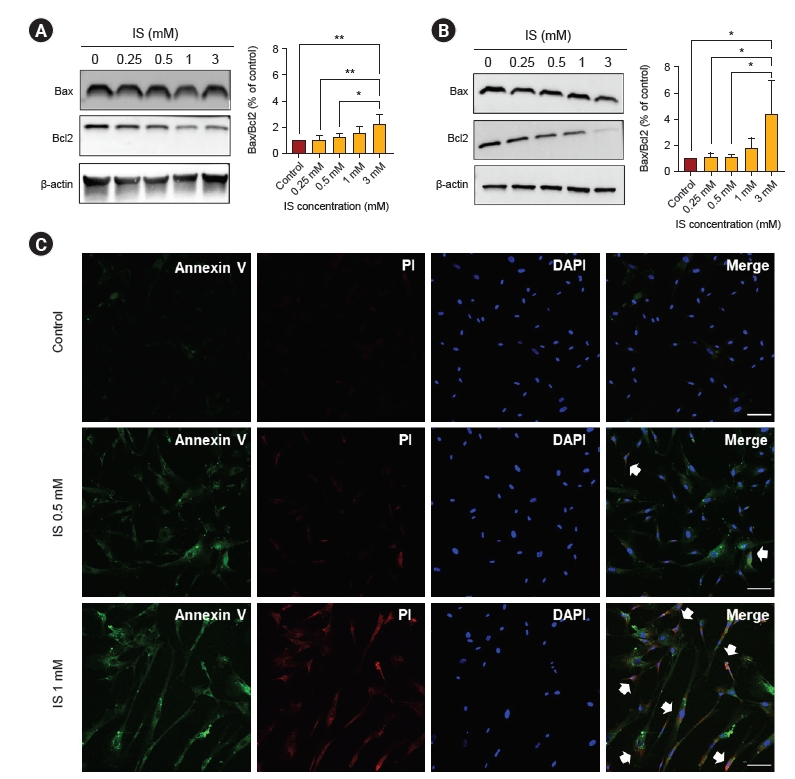
14. Lin YT, Wu PH, Tsai YC, et al. Indoxyl sulfate induces apoptosis through oxidative stress and mitogen-activated protein kinase signaling pathway inhibition in human astrocytes.
J Clin Med 2019;8:191.



15. Bobot M, Thomas L, Moyon A, et al. Uremic toxic blood-brain barrier disruption mediated by AhR activation leads to cognitive impairment during experimental renal dysfunction.
J Am Soc Nephrol 2020;31:1509–1521.



16. Li LC, Chen WY, Chen JB, et al. The AST-120 recovers uremic toxin-induced cognitive deficit via NLRP3 inflammasome pathway in astrocytes and microglia.
Biomedicines 2021;9:1252.



17. Yoo ID, Park MW, Cha HW, et al. Elevated CLOCK and BMAL1 contribute to the impairment of aerobic glycolysis from astrocytes in Alzheimer’s disease.
Int J Mol Sci 2020;21:7862.



18. Park MW, Cha HW, Kim J, et al. NOX4 promotes ferroptosis of astrocytes by oxidative stress-induced lipid peroxidation via the impairment of mitochondrial metabolism in Alzheimer’s diseases.
Redox Biol 2021;41:101947.



19. Grünewald A, Kumar KR, Sue CM. New insights into the complex role of mitochondria in Parkinson’s disease.
Prog Neurobiol 2019;177:73–93.


20. Vlassenko AG, Raichle ME. Brain aerobic glycolysis functions and Alzheimer’s disease.
Clin Transl Imaging 2015;3:27–37.



21. Xiong XY, Tang Y, Yang QW. Metabolic changes favor the activity and heterogeneity of reactive astrocytes.
Trends Endocrinol Metab 2022;33:390–400.


22. Ardanaz CG, Ramírez MJ, Solas M. Brain metabolic alterations in Alzheimer’s disease.
Int J Mol Sci 2022;23:3785.



23. Hasel P, Liddelow SA. Astrocytes.
Curr Biol 2021;31:R326–R327.


24. Vicente-Gutierrez C, Bonora N, Bobo-Jimenez V, et al. Astrocytic mitochondrial ROS modulate brain metabolism and mouse behaviour.
Nat Metab 2019;1:201–211.



25. Park S, Kim JI, Cho NJ, et al. Decreased glucose utilization contributes to memory impairment in patients with glufosinate ammonium intoxication.
J Clin Med 2020;9:1213.



26. Bélanger M, Allaman I, Magistretti PJ. Brain energy metabolism: focus on astrocyte-neuron metabolic cooperation.
Cell Metab 2011;14:724–738.


27. Zhang Y, Chen K, Sloan SA, et al. An RNA-sequencing transcriptome and splicing database of glia, neurons, and vascular cells of the cerebral cortex.
J Neurosci 2014;34:11929–11947.



28. Yu YH, Kim SW, Park DK, Song HY, Kim DS, Gil HW. Altered emotional phenotypes in chronic kidney disease following 5/6 nephrectomy.
Brain Sci 2021;11:882.



29. Assem M, Lando M, Grissi M, et al. The impact of uremic toxins on cerebrovascular and cognitive disorders.
Toxins (Basel) 2018;10:303.



31. Yu YH, Kim SW, Im H, et al. Cognitive sequelae and hippocampal dysfunction in chronic kidney disease following 5/6 nephrectomy.
Brain Sci 2022;12:905.



33. Gray LR, Tompkins SC, Taylor EB. Regulation of pyruvate metabolism and human disease.
Cell Mol Life Sci 2014;71:2577–2604.



34. Patel KP, O’Brien TW, Subramony SH, Shuster J, Stacpoole PW. The spectrum of pyruvate dehydrogenase complex deficiency: clinical, biochemical and genetic features in 371 patients.
Mol Genet Metab 2012;106:385–394.



36. Xu Y, Fu EL, Clase CM, Mazhar F, Jardine MJ, Carrero JJ. GLP-1 receptor agonist versus DPP-4 inhibitor and kidney and cardiovascular outcomes in clinical practice in type-2 diabetes.
Kidney Int 2022;101:360–368.


37. Chen JJ, Wu CY, Jenq CC, et al. Association of glucagon-like peptide-1 receptor agonist vs dipeptidyl peptidase-4 inhibitor use with mortality among patients with type 2 diabetes and advanced chronic kidney disease.
JAMA Netw Open 2022;5:e221169.



38. Zheng J, Xie Y, Ren L, et al. GLP-1 improves the supportive ability of astrocytes to neurons by promoting aerobic glycolysis in Alzheimer’s disease.
Mol Metab 2021;47:101180.



39. Takuma K, Baba A, Matsuda T. Astrocyte apoptosis: implications for neuroprotection.
Prog Neurobiol 2004;72:111–127.


40. Adesso S, Paterniti I, Cuzzocrea S, et al. AST-120 reduces neuroinflammation induced by indoxyl sulfate in glial cells.
J Clin Med 2018;7:365.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















