1. Levey AS, Andreoli SP, DuBose T, Provenzano R, Collins AJ. Chronic kidney disease: common, harmful, and treatable--World Kidney Day 2007.
J Am Soc Nephrol 18:374–378. 2007;


3. MacNeill SJ, Casula A, Shaw C, Castledine C. UK renal registry 18th annual report: chapter 2 UK renal replacement therapy prevalence in 2014: national and centre-specific analyses.
Nephron 132:Suppl 1. 41–68. 2016;


4. Dhoul N, de Lusignan S, Dmitrieva O, Stevens P, O’Donoghue D. Quality achievement and disease prevalence in primary care predicts regional variation in renal replacement therapy (RRT) incidence: an ecological study.
Nephrol Dial Transplant 27:739–746. 2012;


5. Allon M. Current management of vascular access.
Clin J Am Soc Nephrol 2:786–800. 2007;


6. Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG. Vascular access and all-cause mortality: a propensity score analysis.
J Am Soc Nephrol 15:477–486. 2004;


7. Asif A, Cherla G, Merrill D, et al. Conversion of tunneled hemodialysis catheter-consigned patients to arteriovenous fistula.
Kidney Int 67:2399–2406. 2005;


8. Nassar GM. Endovascular management of the “failing to mature” arteriovenous fistula.
Tech Vasc Interv Radiol 11:175–180. 2008;


10. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II).
J Vasc Surg 45(Suppl S):S5–S67. 2007;


11. National Kidney Foundation. KDOQI clinical practice guidelines and clinical practice recommendations 2006 updates: hemodialysis adequacy, peritoneal dialysis adequacy, vascular access.
Am J Kidney Dis 48:S1–S322. 2006.

12. Patel ST, Hughes J, Mills JL Sr.. Failure of arteriovenous fistula maturation: an unintended consequence of exceeding dialysis outcome quality initiative guidelines for hemodialysis access.
J Vasc Surg 38:439–445. discussion 445. 2003


13. Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures.
Epidemiology 21:128–138. 2010;


14. Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors.
Stat Med 15:361–387. 1996;


15. Vergouwe Y, Steyerberg EW, Eijkemans MJ, Habbema JD. Substantial effective sample sizes were required for external validation studies of predictive logistic regression models.
J Clin Epidemiol 58:475–483. 2005;


16. Weale AR, Bevis P, Neary WD, et al. Radiocephalic and brachiocephalic arteriovenous fistula outcomes in the elderly.
J Vasc Surg 47:144–150. 2008;


17. Zeebregts C, van den Dungen J, Bolt A, Franssen C, Verhoeven E, van Schilfgaarde R. Factors predictive of failure of Brescia-Cimino arteriovenous fistulas.
Eur J Surg 168:29–36. 2002;


18. Jindal K, Chan CT, Deziel C, et al. Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology.
J Am Soc Nephrol 17(3 Suppl 1):S1–S27. 2006;

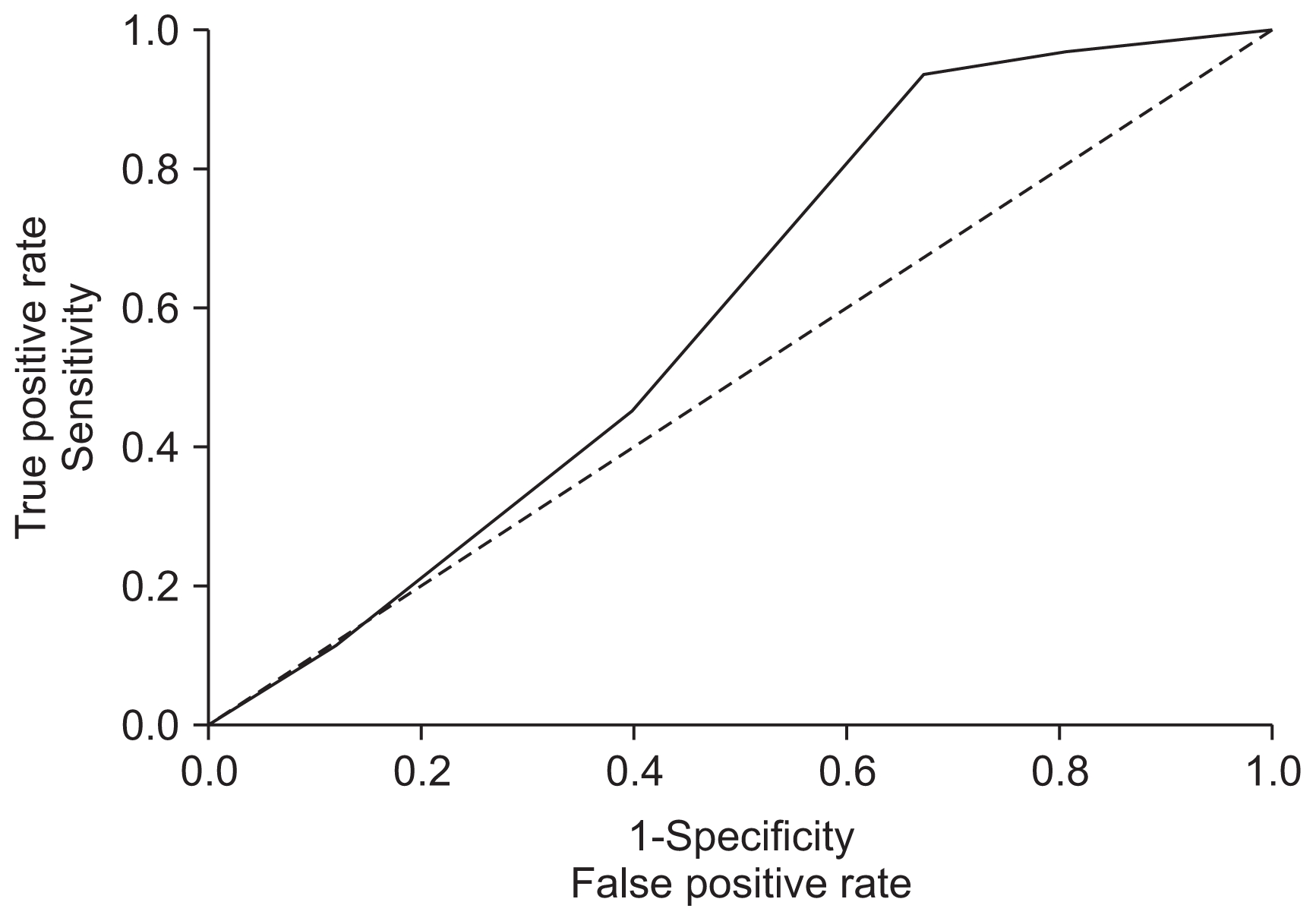
19. Brubaker PH. Do not be statistically cenophobic: time to roc and roll!
J Cardiopulm Rehabil Prev 28:420–421. 2008;

20. Miller PE, Tolwani A, Luscy CP, et al. Predictors of adequacy of arteriovenous fistulas in hemodialysis patients.
Kidney Int 56:275–280. 1999;


21. Iyem H. Early follow-up results of arteriovenous fistulae created for hemodialysis.
Vasc Health Risk Manag 7:321–325. 2011;



22. Lok CE, Allon M, Moist L, Oliver MJ, Shah H, Zimmerman D. Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I).
J Am Soc Nephrol 17:3204–3212. 2006;


23. Başer M, Sayarlıoğlu H, Doğan E, Erkoç R, Çiftçi A, Çetin Kotan M. Comparison of proximal distal success rate in A-V fistulas settled for haemodialysis. Van Med J 13:42–45. 2006.
24. Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction.
Circulation 115:928–935. 2007;


25. Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond.
Stat Med 27:157–172. discussion 207–212. 2008


26. Obialo CI, Tagoe AT, Martin PC, Asche-Crowe PE. Adequacy and survival of autogenous arteriovenous fistula in African American hemodialysis patients.
ASAIO J 49:435–439. 2003;

27. Chan MR, Young HN, Becker YT, Yevzlin AS. Obesity as a predictor of vascular access outcomes: analysis of the USRDS DMMS Wave II study.
Semin Dial 21:274–279. 2008;


28. Feldman HI, Joffe M, Rosas SE, Burns JE, Knauss J, Brayman K. Predictors of successful arteriovenous fistula maturation.
Am J Kidney Dis 42:1000–1012. 2003;


29. Bashar K, Zafar A, Elsheikh S, et al. Predictive parameters of arteriovenous fistula functional maturation in a population of patients with end-stage renal disease.
PLoS One 10:e01199582015;



30. Mendes RR, Farber MA, Marston WA, Dinwiddie LC, Keagy BA, Burnham SJ. Prediction of wrist arteriovenous fistula maturation with preoperative vein mapping with ultrasonography.
J Vasc Surg 36:460–463. 2002;


31. Khavanin Zadeh M, Gholipour F, Naderpour Z, Porfakharan M. Relationship between vessel diameter and time to maturation of arteriovenous fistula for hemodialysis access.
Int J Nephrol 2012:9429502012;


32. Brimble KS, Rabbat ChG, Treleaven DJ, Ingram AJ. Utility of ultrasonographic venous assessment prior to forearm arteriovenous fistula creation.
Clin Nephrol 58:122–127. 2002;


33. Wong V, Ward R, Taylor J, Selvakumar S, How TV, Bakran A. Factors associated with early failure of arteriovenous fistulae for haemodialysis access.
Eur J Vasc Endovasc Surg 12:207–213. 1996;


34. Royston P, Moons KG, Altman DG, Vergouwe Y. Prognosis and prognostic research: developing a prognostic model.
BMJ 338:b6042009;


35. Grzegorczyk-Martin V, Khrouf M, Bringer-Deutsch S, et al. Low circulating anti-Müllerian hormone and normal follicle stimulating hormone levels: which prognosis in an IVF program?
Gynecol Obstet Fertil 40:411–418. 2012 In French.

36. Steyerberg EW, Borsboom GJ, van Houwelingen HC, Eijkemans MJ, Habbema JD. Validation and updating of predictive logistic regression models: a study on sample size and shrinkage.
Stat Med 23:2567–2586. 2004;


37. Monroy-Cuadros M, Yilmaz S, Salazar-Bañuelos A, Doig C. Risk factors associated with patency loss of hemodialysis vascular access within 6 months.
Clin J Am Soc Nephrol 5:1787–1792. 2010;



38. Grandaliano G, Teutonico A, Allegretti A, et al. The role of hyperparathyroidism, erythropoietin therapy, and CMV infection in the failure of arteriovenous fistula in hemodialysis.
Kidney Int 64:715–719. 2003;


39. Chan CY, Chen YS, Ma MC, Chen CF. Remodeling of experimental arteriovenous fistula with increased matrix metalloproteinase expression in rats.
J Vasc Surg 45:804–811. 2007;


40. Lee ES, Shen Q, Pitts RL, et al. Serum metalloproteinases MMP-2, MMP-9 and metalloproteinase tissue inhibitors in patients are associated with arteriovenous fistula maturation.
J Vasc Surg 54:454–459. discussion 459–460. 2011







 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















