1. Ahmad AA, Draves SO, Rosca M. Mitochondria in diabetic kidney disease.
Cells 2021;10:2945.



2. Tang C, Cai J, Yin XM, Weinberg JM, Venkatachalam MA, Dong Z. Mitochondrial quality control in kidney injury and repair.
Nat Rev Nephrol 2021;17:299ŌĆō318.



3. Sygitowicz G, Sitkiewicz D. Mitochondrial quality control: the role in cardiac injury.
Front Biosci (Landmark Ed) 2022;27:96.


4. Pickles S, Vigi├® P, Youle RJ. Mitophagy and quality control mechanisms in mitochondrial maintenance.
Curr Biol 2018;28:R170ŌĆōR185.



5. Yao L, Liang X, Qiao Y, Chen B, Wang P, Liu Z. Mitochondrial dysfunction in diabetic tubulopathy.
Metabolism 2022;131:155195.


6. Sharma K, Karl B, Mathew AV, et al. Metabolomics reveals signature of mitochondrial dysfunction in diabetic kidney disease.
J Am Soc Nephrol 2013;24:1901ŌĆō1912.



7. Zhan M, Usman IM, Sun L, Kanwar YS. Disruption of renal tubular mitochondrial quality control by Myo-inositol oxygenase in diabetic kidney disease.
J Am Soc Nephrol 2015;26:1304ŌĆō1321.


8. Hu Y, Chen H, Zhang L, et al. The AMPK-MFN2 axis regulates MAM dynamics and autophagy induced by energy stresses.
Autophagy 2021;17:1142ŌĆō1156.


9. Long J, Badal SS, Ye Z, et al. Long noncoding RNA Tug1 regulates mitochondrial bioenergetics in diabetic nephropathy.
J Clin Invest 2016;126:4205ŌĆō4218.



10. Magnani ND, Marchini T, Calabr├│ V, Alvarez S, Evelson P. Role of mitochondria in the redox signaling network and its outcomes in high impact inflammatory syndromes.
Front Endocrinol (Lausanne) 2020;11:568305.



11. Schulz E, Wenzel P, M├╝nzel T, Daiber A. Mitochondrial redox signaling: interaction of mitochondrial reactive oxygen species with other sources of oxidative stress.
Antioxid Redox Signal 2014;20:308ŌĆō324.



12. Quoilin C, Mouithys-Mickalad A, L├®cart S, Fontaine-Aupart MP, Hoebeke M. Evidence of oxidative stress and mitochondrial respiratory chain dysfunction in an in vitro model of sepsis-induced kidney injury.
Biochim Biophys Acta 2014;1837:1790ŌĆō1800.


13. Song J, Herrmann JM, Becker T. Quality control of the mitochondrial proteome.
Nat Rev Mol Cell Biol 2021;22:54ŌĆō70.



15. Jadiya P, Tomar D. Mitochondrial protein quality control mechanisms.
Genes (Basel) 2020;11:563.



16. Kazak L, Reyes A, Holt IJ. Minimizing the damage: repair pathways keep mitochondrial DNA intact.
Nat Rev Mol Cell Biol 2012;13:659ŌĆō671.



17. Sharma P, Sampath H. Mitochondrial DNA integrity: role in health and disease.
Cells 2019;8:100.



18. Zinovkina LA. Mechanisms of mitochondrial DNA repair in mammals.
Biochemistry (Mosc) 2018;83:233ŌĆō249.



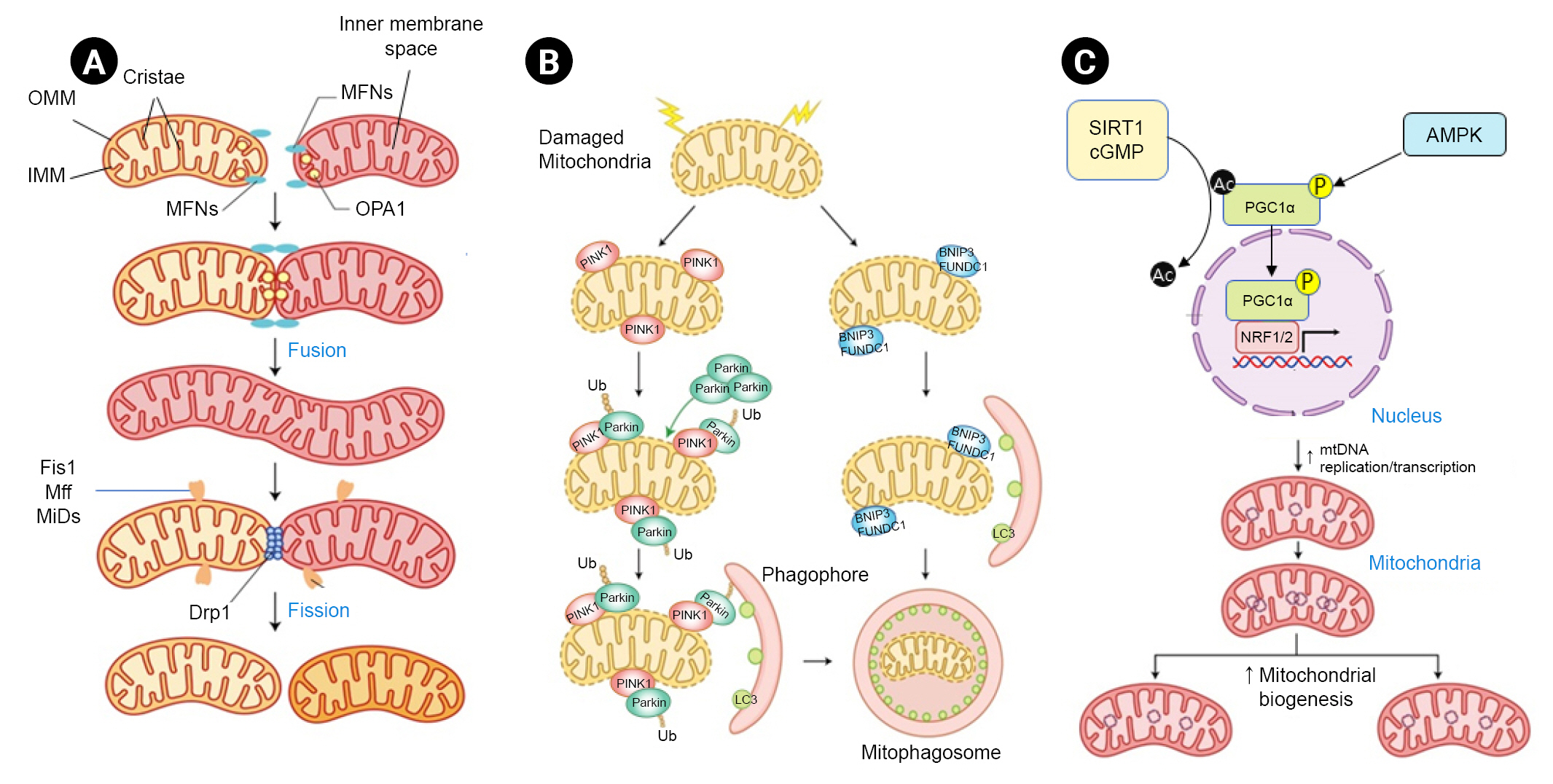
19. van der Bliek AM, Shen Q, Kawajiri S. Mechanisms of mitochondrial fission and fusion.
Cold Spring Harb Perspect Biol 2013;5:a011072.



20. Westermann B. Mitochondrial fusion and fission in cell life and death.
Nat Rev Mol Cell Biol 2010;11:872ŌĆō884.



21. Bhatia D, Choi ME. The emerging role of mitophagy in kidney diseases.
J Life Sci (Westlake Village) 2019;1:13ŌĆō22.



22. Ma K, Chen G, Li W, Kepp O, Zhu Y, Chen Q. Mitophagy, mitochondrial homeostasis, and cell fate.
Front Cell Dev Biol 2020;8:467.



24. Fernandez-Marcos PJ, Auwerx J. Regulation of PGC-1╬▒, a nodal regulator of mitochondrial biogenesis.
Am J Clin Nutr 2011;93:884SŌĆō890S.



25. Balzer MS, Rohacs T, Susztak K. How many cell types are in the kidney and what do they do?
Annu Rev Physiol 2022;84:507ŌĆō531.


26. Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW. Brenner & RectorŌĆÖs the kidney. 11th ed. Elsevier; 2019. Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MWBrenner & RectorŌĆÖs the kidney. 11th ed. Elsevier; 2019.
27. Gerich JE. Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications.
Diabet Med 2010;27:136ŌĆō142.



28. ├śstergaard JA, Cooper ME, Jandeleit-Dahm KA. Targeting oxidative stress and anti-oxidant defence in diabetic kidney disease.
J Nephrol 2020;33:917ŌĆō929.



29. Hall AM, Unwin RJ, Parker N, Duchen MR. Multiphoton imaging reveals differences in mitochondrial function between nephron segments.
J Am Soc Nephrol 2009;20:1293ŌĆō1302.



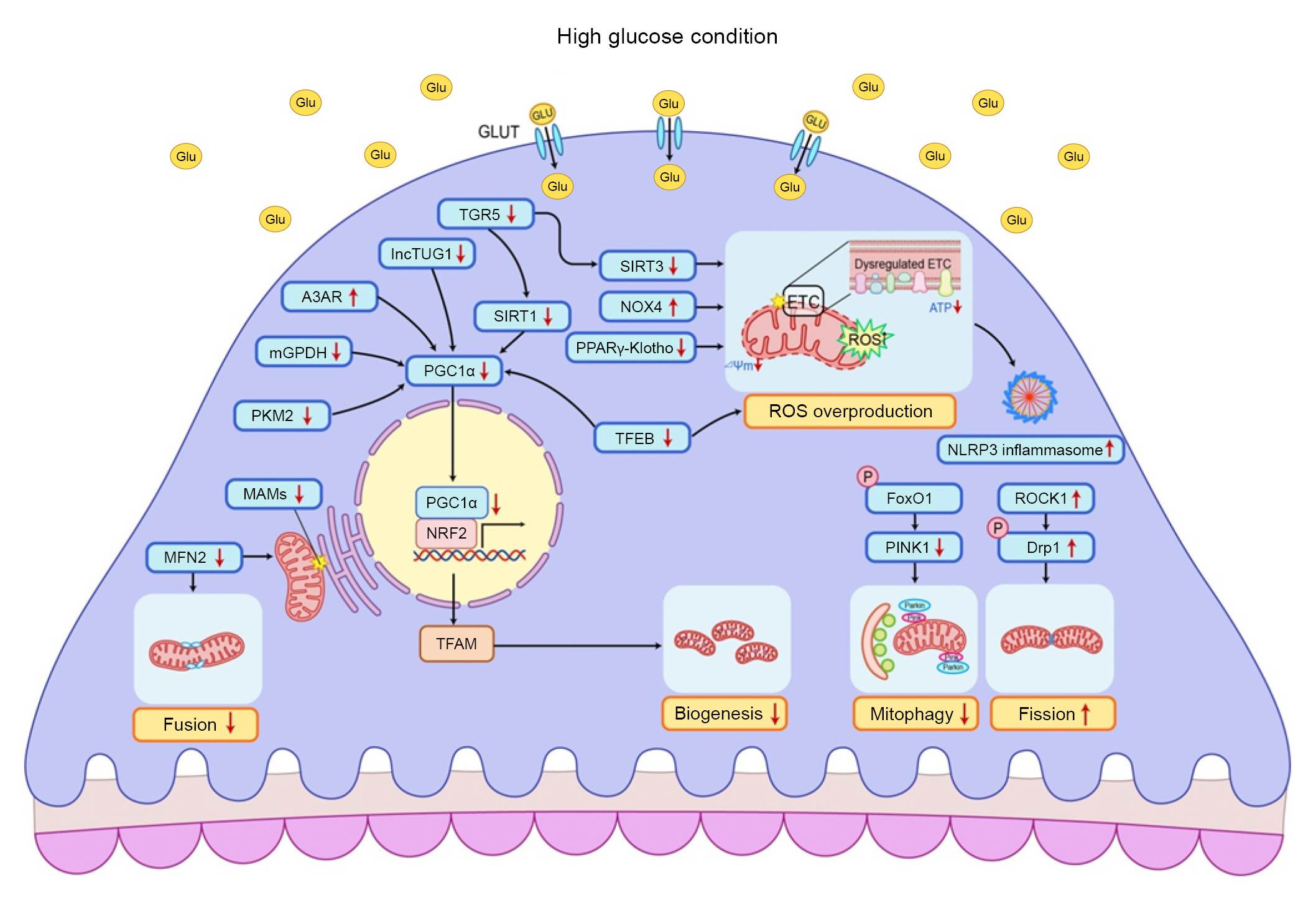
30. Munusamy S, MacMillan-Crow LA. Mitochondrial superoxide plays a crucial role in the development of mitochondrial dysfunction during high glucose exposure in rat renal proximal tubular cells.
Free Radic Biol Med 2009;46:1149ŌĆō1157.


31. Ogura Y, Kitada M, Monno I, Kanasaki K, Watanabe A, Koya D. Renal mitochondrial oxidative stress is enhanced by the reduction of Sirt3 activity, in Zucker diabetic fatty rats.
Redox Rep 2018;23:153ŌĆō159.



32. Ogura Y, Kitada M, Xu J, Monno I, Koya D. CD38 inhibition by apigenin ameliorates mitochondrial oxidative stress through restoration of the intracellular NAD+/NADH ratio and Sirt3 activity in renal tubular cells in diabetic rats.
Aging (Albany NY) 2020;12:11325ŌĆō11336.



33. Zheng X, Narayanan S, Xu C, et al. Repression of hypoxia-inducible factor-1 contributes to increased mitochondrial reactive oxygen species production in diabetes.
Elife 2022;11:e70714.


35. Coughlan MT, Nguyen TV, Penfold SA, et al. Mapping time-course mitochondrial adaptations in the kidney in experimental diabetes.
Clin Sci (Lond) 2016;130:711ŌĆō720.



36. Lee YH, Kim SH, Kang JM, et al. Empagliflozin attenuates diabetic tubulopathy by improving mitochondrial fragmentation and autophagy.
Am J Physiol Renal Physiol 2019;317:F767ŌĆōF780.


37. Liu X, Xu C, Xu L, et al. Empagliflozin improves diabetic renal tubular injury by alleviating mitochondrial fission via AMPK/SP1/PGAM5 pathway.
Metabolism 2020;111:154334.


38. Zhang Q, He L, Dong Y, et al. Sitagliptin ameliorates renal tubular injury in diabetic kidney disease via STAT3-dependent mitochondrial homeostasis through SDF-1╬▒/CXCR4 pathway.
FASEB J 2020;34:7500ŌĆō7519.



39. Zhan M, Usman I, Yu J, et al. Perturbations in mitochondrial dynamics by p66Shc lead to renal tubular oxidative injury in human diabetic nephropathy.
Clin Sci (Lond) 2018;132:1297ŌĆō1314.



40. Xiao L, Xu X, Zhang F, et al. The mitochondria-targeted antioxidant MitoQ ameliorated tubular injury mediated by mitophagy in diabetic kidney disease via Nrf2/PINK1.
Redox Biol 2017;11:297ŌĆō311.


43. Yang DY, Zhou X, Liu ZW, Xu XQ, Liu C. LncRNA NEAT1 accelerates renal tubular epithelial cell damage by modulating mitophagy via miR-150-5p-DRP1 axis in diabetic nephropathy.
Exp Physiol 2021;106:1631ŌĆō1642.



44. Liu L, Bai F, Song H, et al. Upregulation of TIPE1 in tubular epithelial cell aggravates diabetic nephropathy by disrupting PHB2 mediated mitophagy.
Redox Biol 2022;50:102260.



45. Tang H, Yang M, Liu Y, et al. Melatonin alleviates renal injury by activating mitophagy in diabetic nephropathy.
Front Endocrinol (Lausanne) 2022;13:889729.



46. Li C, Li L, Yang M, et al. PACS-2 ameliorates tubular injury by facilitating endoplasmic reticulum-mitochondria contact and mitophagy in diabetic nephropathy.
Diabetes 2022;71:1034ŌĆō1050.



52. Liu S, Yuan Y, Xue Y, Xing C, Zhang B. Podocyte injury in diabetic kidney disease: a focus on mitochondrial dysfunction.
Front Cell Dev Biol 2022;10:832887.



53. Susztak K, Raff AC, Schiffer M, B├Čttinger EP. Glucose-induced reactive oxygen species cause apoptosis of podocytes and podocyte depletion at the onset of diabetic nephropathy.
Diabetes 2006;55:225ŌĆō233.



54. Xing L, Fang J, Zhu B, et al. Astragaloside IV protects against podocyte apoptosis by inhibiting oxidative stress via activating PPAR╬│-Klotho-FoxO1 axis in diabetic nephropathy.
Life Sci 2021;269:119068.


55. Chen Z, Zhou Q, Liu C, Zeng Y, Yuan S. Klotho deficiency aggravates diabetes-induced podocyte injury due to DNA damage caused by mitochondrial dysfunction.
Int J Med Sci 2020;17:2763ŌĆō2772.



56. Xing L, Guo H, Meng S, et al. Klotho ameliorates diabetic nephropathy by activating Nrf2 signaling pathway in podocytes.
Biochem Biophys Res Commun 2021;534:450ŌĆō456.


57. You YH, Quach T, Saito R, Pham J, Sharma K. Metabolomics reveals a key role for fumarate in mediating the effects of NADPH oxidase 4 in diabetic kidney disease.
J Am Soc Nephrol 2016;27:466ŌĆō481.


58. Liang Y, Liu H, Fang Y, et al. Salvianolate ameliorates oxidative stress and podocyte injury through modulation of NOX4 activity in db/db mice.
J Cell Mol Med 2021;25:1012ŌĆō1023.



59. Shahzad K, Bock F, Dong W, et al. Nlrp3-inflammasome activation in non-myeloid-derived cells aggravates diabetic nephropathy.
Kidney Int 2015;87:74ŌĆō84.


60. Qiu YY, Tang LQ. Roles of the NLRP3 inflammasome in the pathogenesis of diabetic nephropathy.
Pharmacol Res 2016;114:251ŌĆō264.


61. Wang W, Wang Y, Long J, et al. Mitochondrial fission triggered by hyperglycemia is mediated by ROCK1 activation in podocytes and endothelial cells.
Cell Metab 2012;15:186ŌĆō200.



62. Ayanga BA, Badal SS, Wang Y, et al. Dynamin-related protein 1 deficiency improves mitochondrial fitness and protects against progression of diabetic nephropathy.
J Am Soc Nephrol 2016;27:2733ŌĆō2747.



63. Cao Y, Chen Z, Hu J, et al. Mfn2 regulates high glucose-induced MAMs dysfunction and apoptosis in podocytes via PERK pathway.
Front Cell Dev Biol 2021;9:769213.



64. Li W, Du M, Wang Q, et al. FoxO1 promotes mitophagy in the podocytes of diabetic male mice via the PINK1/Parkin pathway.
Endocrinology 2017;158:2155ŌĆō2167.


66. Zhang L, Liu J, Zhou F, Wang W, Chen N. PGC-1╬▒ ameliorates kidney fibrosis in mice with diabetic kidney disease through an antioxidative mechanism.
Mol Med Rep 2018;17:4490ŌĆō4498.



67. Li SY, Susztak K. The role of peroxisome proliferator-activated receptor ╬│ coactivator 1╬▒ (PGC-1╬▒) in kidney disease.
Semin Nephrol 2018;38:121ŌĆō126.



69. Hong Q, Zhang L, Das B, et al. Increased podocyte Sirtuin-1 function attenuates diabetic kidney injury.
Kidney Int 2018;93:1330ŌĆō1343.



70. Qi W, Keenan HA, Li Q, et al. Pyruvate kinase M2 activation may protect against the progression of diabetic glomerular pathology and mitochondrial dysfunction.
Nat Med 2017;23:753ŌĆō762.


71. Wang XX, Edelstein MH, Gafter U, et al. G protein-coupled bile acid receptor TGR5 activation inhibits kidney disease in obesity and diabetes.
J Am Soc Nephrol 2016;27:1362ŌĆō1378.


72. Dorotea D, Cho A, Lee G, et al. Orally active, species-independent novel A3 adenosine receptor antagonist protects against kidney injury in db/db mice.
Exp Mol Med 2018;50:1ŌĆō14.


73. Kang Y, Li Y, Zhang T, Chi Y, Liu M. Effects of transcription factor EB on oxidative stress and apoptosis induced by high glucose in podocytes.
Int J Mol Med 2019;44:447ŌĆō456.



74. Qu H, Gong X, Liu X, et al. Deficiency of mitochondrial glycerol 3-phosphate dehydrogenase exacerbates podocyte injury and the progression of diabetic kidney disease.
Diabetes 2021;70:1372ŌĆō1387.



75. Wang C, Li C, Peng H, et al. Activation of the Nrf2-ARE pathway attenuates hyperglycemia-mediated injuries in mouse podocytes.
Cell Physiol Biochem 2014;34:891ŌĆō902.


76. Fu J, Lee K, Chuang PY, Liu Z, He JC. Glomerular endothelial cell injury and cross talk in diabetic kidney disease.
Am J Physiol Renal Physiol 2015;308:F287ŌĆōF297.


77. Weil EJ, Lemley KV, Mason CC, et al. Podocyte detachment and reduced glomerular capillary endothelial fenestration promote kidney disease in type 2 diabetic nephropathy.
Kidney Int 2012;82:1010ŌĆō1017.



78. Yuen DA, Stead BE, Zhang Y, et al. eNOS deficiency predisposes podocytes to injury in diabetes.
J Am Soc Nephrol 2012;23:1810ŌĆō1823.



79. Qi H, Casalena G, Shi S, et al. Glomerular endothelial mitochondrial dysfunction is essential and characteristic of diabetic kidney disease susceptibility.
Diabetes 2017;66:763ŌĆō778.



80. Tervaert TW, Mooyaart AL, Amann K, et al. Pathologic classification of diabetic nephropathy.
J Am Soc Nephrol 2010;21:556ŌĆō563.


81. An Y, Xu F, Le W, et al. Renal histologic changes and the outcome in patients with diabetic nephropathy.
Nephrol Dial Transplant 2015;30:257ŌĆō266.


82. Okada T, Nagao T, Matsumoto H, Nagaoka Y, Wada T, Nakao T. Histological predictors for renal prognosis in diabetic nephropathy in diabetes mellitus type 2 patients with overt proteinuria.
Nephrology (Carlton) 2012;17:68ŌĆō75.


83. Lee YH, Kim KP, Park SH, et al. Urinary chemokine C-X-C motif ligand 16 and endostatin as predictors of tubulointerstitial fibrosis in patients with advanced diabetic kidney disease.
Nephrol Dial Transplant 2021;36:295ŌĆō305.


85. Nguyen D, Ping F, Mu W, Hill P, Atkins RC, Chadban SJ. Macrophage accumulation in human progressive diabetic nephropathy.
Nephrology (Carlton) 2006;11:226ŌĆō231.


87. Jagannathan-Bogdan M, McDonnell ME, Shin H, et al. Elevated proinflammatory cytokine production by a skewed T cell compartment requires monocytes and promotes inflammation in type 2 diabetes.
J Immunol 2011;186:1162ŌĆō1172.



90. Dai W, Lu H, Chen Y, Yang D, Sun L, He L. The loss of mitochondrial quality control in diabetic kidney disease.
Front Cell Dev Biol 2021;9:706832.



92. Pena MJ, de Zeeuw D, Andress D, et al. The effects of atrasentan on urinary metabolites in patients with type 2 diabetes and nephropathy.
Diabetes Obes Metab 2017;19:749ŌĆō753.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















