1. Umanath K, Lewis JB. Update on diabetic nephropathy: core curriculum 2018.
Am J Kidney Dis 2018;71:884–895.


2. Wolf G. New insights into the pathophysiology of diabetic nephropathy: from haemodynamics to molecular pathology.
Eur J Clin Invest 2004;34:785–796.


3. Bhattacharjee N, Barma S, Konwar N, Dewanjee S, Manna P. Mechanistic insight of diabetic nephropathy and its pharmacotherapeutic targets: an update.
Eur J Pharmacol 2016;791:8–24.


6. Chen B, Li Y, Liu Y, Xu Z. circLRP6 regulates high glucose-induced proliferation, oxidative stress, ECM accumulation, and inflammation in mesangial cells.
J Cell Physiol 2019;234:21249–21259.



7. Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease.
Cell 2009;139:871–890.


8. Gonzalez DM, Medici D. Signaling mechanisms of the epithelial-mesenchymal transition.
Sci Signal 2014;7:re8.



9. Gao P, Li L, Yang L, et al. Yin Yang 1 protein ameliorates diabetic nephropathy pathology through transcriptional repression of TGFβ1.
Sci Transl Med 2019;11:eaaw2050.


12. Qiao S, Liu R, Lv C, et al. Bergenin impedes the generation of extracellular matrix in glomerular mesangial cells and ameliorates diabetic nephropathy in mice by inhibiting oxidative stress via the mTOR/β-TrcP/Nrf2 pathway.
Free Radic Biol Med 2019;145:118–135.


13. Shi X, Sun M, Liu H, Yao Y, Song Y. Long non-coding RNAs: a new frontier in the study of human diseases.
Cancer Lett 2013;339:159–166.


15. Gao J, Wang W, Wang F, Guo C. LncRNA-NR_033515 promotes proliferation, fibrogenesis and epithelial-to-mesenchymal transition by targeting miR-743b-5p in diabetic nephropathy.
Biomed Pharmacother 2018;106:543–552.


16. Liu DW, Zhang JH, Liu FX, et al. Silencing of long noncoding RNA PVT1 inhibits podocyte damage and apoptosis in diabetic nephropathy by upregulating FOXA1.
Exp Mol Med 2019;51:1–15.


17. Miyoshi N, Wagatsuma H, Wakana S, et al. Identification of an imprinted gene, Meg3/Gtl2 and its human homologue MEG3, first mapped on mouse distal chromosome 12 and human chromosome 14q.
Genes Cells 2000;5:211–220.



18. Ghafouri-Fard S, Taheri M. Maternally expressed gene 3 (MEG3): a tumor suppressor long non coding RNA.
Biomed Pharmacother 2019;118:109129.


19. Shihabudeen Haider Ali MS, Cheng X, Moran M, et al. LncRNA Meg3 protects endothelial function by regulating the DNA damage response.
Nucleic Acids Res 2019;47:1505–1522.


21. Li J, Jiang X, Duan L, Wang W. Long non-coding RNA MEG3 impacts diabetic nephropathy progression through sponging miR-145.
Am J Transl Res 2019;11:6691–6698.


22. Zha F, Qu X, Tang B, et al. Long non-coding RNA MEG3 promotes fibrosis and inflammatory response in diabetic nephropathy via miR-181a/Egr-1/TLR4 axis.
Aging (Albany NY) 2019;11:3716–3730.



23. Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function.
Cell 2004;116:281–297.


24. Mendell JT, Olson EN. MicroRNAs in stress signaling and human disease.
Cell 2012;148:1172–1187.



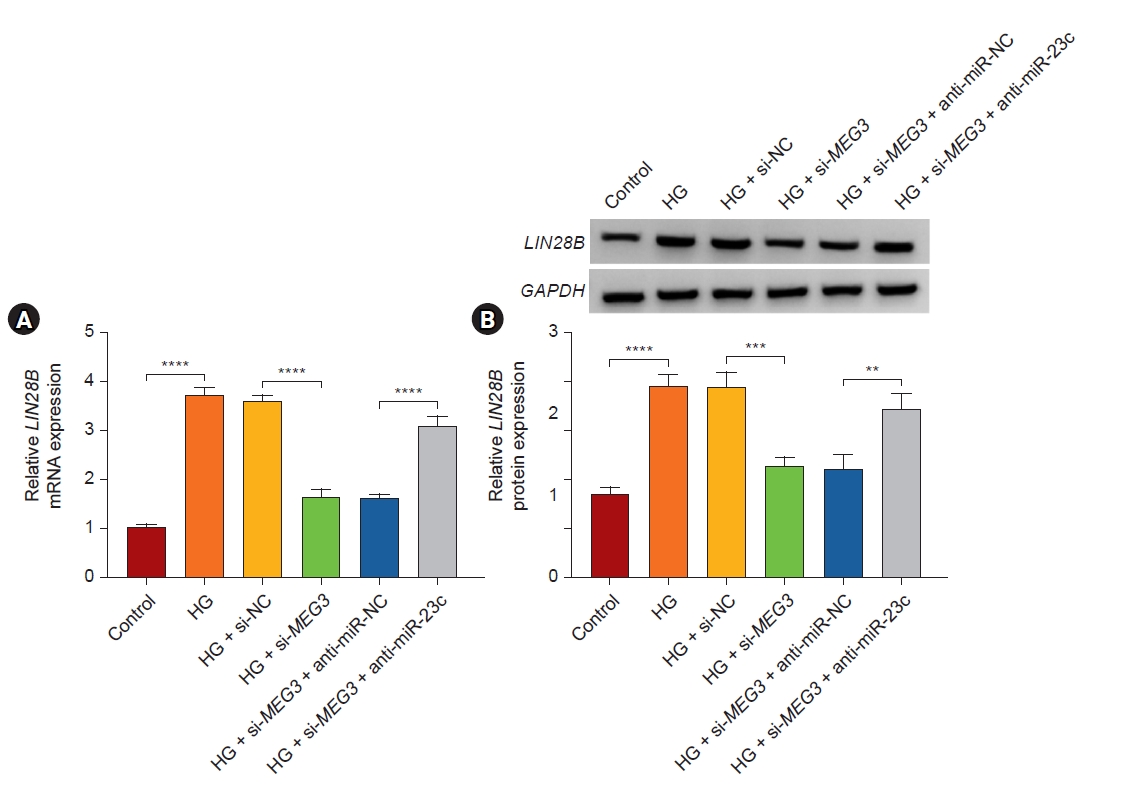
25. Lu M, Ding N, Zhuang S, Li Y. LINC01410/miR-23c/CHD7 functions as a ceRNA network to affect the prognosis of patients with endometrial cancer and strengthen the malignant properties of endometrial cancer cells.
Mol Cell Biochem 2020;469:9–19.



26. Zhang L, Wang L, Wang Y, et al. LncRNA KTN1-AS1 promotes tumor growth of hepatocellular carcinoma by targeting miR-23c/ERBB2IP axis.
Biomed Pharmacother 2019;109:1140–1147.


27. Li X, Zeng L, Cao C, et al. Long noncoding RNA MALAT1 regulates renal tubular epithelial pyroptosis by modulated miR-23c targeting of ELAVL1 in diabetic nephropathy.
Exp Cell Res 2017;350:327–335.


28. Li N, Jia T, Li YR. LncRNA NEAT1 accelerates the occurrence and development of diabetic nephropathy by sponging miR-23c.
Eur Rev Med Pharmacol Sci 2020;24:1325–1337.

29. Loganathan TS, Sulaiman SA, Abdul Murad NA, et al. Interactions among non-coding RNAs in diabetic nephropathy.
Front Pharmacol 2020;11:191.



30. Xu J, Chen Y, Xing Y, Ye S. Metformin inhibits high glucose-induced mesangial cell proliferation, inflammation and ECM expression through the SIRT1-FOXO1-autophagy axis.
Clin Exp Pharmacol Physiol 2019;46:813–820.



31. Wu J, Liu J, Ding Y, et al. MiR-455-3p suppresses renal fibrosis through repression of ROCK2 expression in diabetic nephropathy.
Biochem Biophys Res Commun 2018;503:977–983.


32. Carew RM, Wang B, Kantharidis P. The role of EMT in renal fibrosis.
Cell Tissue Res 2012;347:103–116.



33. Salmena L, Poliseno L, Tay Y, Kats L, Pandolfi PP. A ceRNA hypothesis: the Rosetta Stone of a hidden RNA language?
Cell 2011;146:353–358.



34. Zhang J, Ratanasirintrawoot S, Chandrasekaran S, et al. LIN28 regulates stem cell metabolism and conversion to primed pluripotency.
Cell Stem Cell 2016;19:66–80.


35. Guo W, Hu Z, Bao Y, et al. A LIN28B tumor-specific transcript in cancer.
Cell Rep 2018;22:2016–2025.


36. Fu X, Ou B. miR-152/LIN28B axis modulates high-glucose-induced angiogenesis in human retinal endothelial cells via VEGF signaling.
J Cell Biochem 2020;121:954–962.



37. Park JT, Kato M, Lanting L, et al. Repression of let-7 by transforming growth factor-β1-induced Lin28 upregulates collagen expression in glomerular mesangial cells under diabetic conditions.
Am J Physiol Renal Physiol 2014;307:F1390–F1403.



38. Li N, Wang LJ, Xu WL, Liu S, Yu JY. MicroRNA‑379‑5p suppresses renal fibrosis by regulating the LIN28/let‑7 axis in diabetic nephropathy.
Int J Mol Med 2019;44:1619–1628.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement figure 1
Supplement figure 1 Print
Print















