| Kidney Res Clin Pract > Epub ahead of print |
Abstract
Background
Method
Results
Notes
Funding
This study was supported by a grant (NRF-2020R1A2C2003438) from the National Research Foundation (NRF) funded by the Ministry of Science and ICT, Korea. It was also supported by the Soonchunhyang University Research Fund.
Data sharing statement
The data presented in this study are available on request from the corresponding author.
AuthorsŌĆÖ contributions
Conceptualization, Methodology: WJK, TO, EYL
Data curation: WJK, TO
Formal analysis: WJK, TO, NHH, KK, GES, SHJ
Funding acquisition: EYL
Investigation: SP, NJC, HWG, EYL, JHL
WritingŌĆōoriginal draft: WJK, TO, SP, EYL
WritingŌĆōreview & editing: WJK, TO, SP, EYL
All authors read and approved the final manuscript.
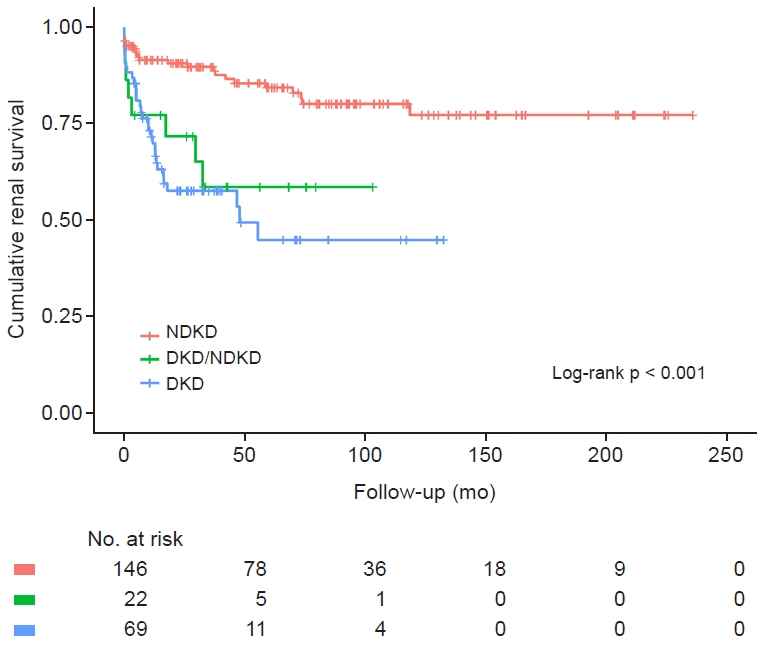
Figure┬Ā1.
Cumulative renal survival between the groups.
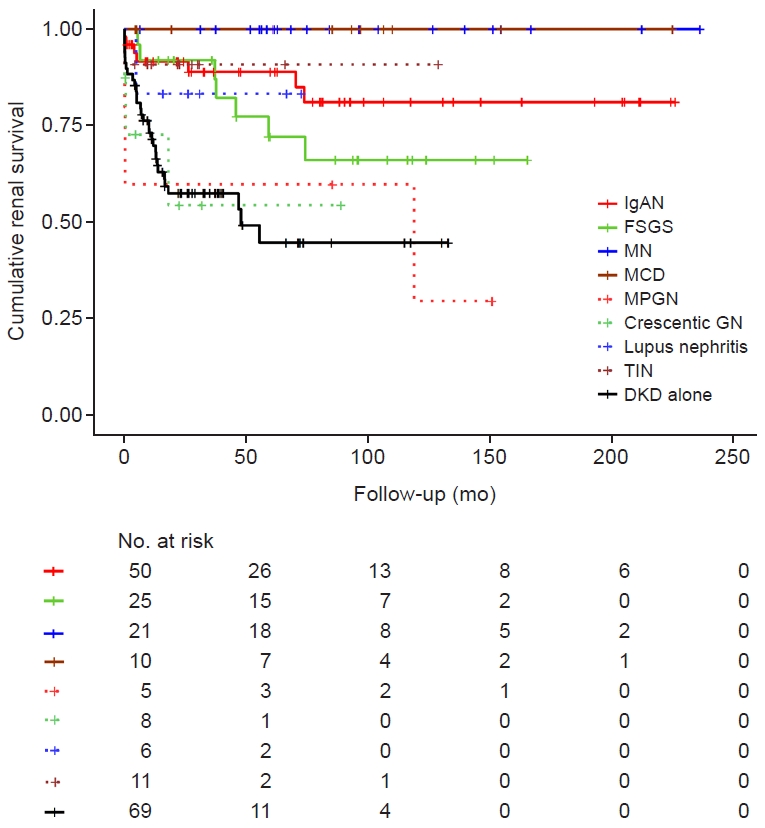
Figure┬Ā2.
Cumulative renal survival in the NDKD group compared to the DKD-alone group.
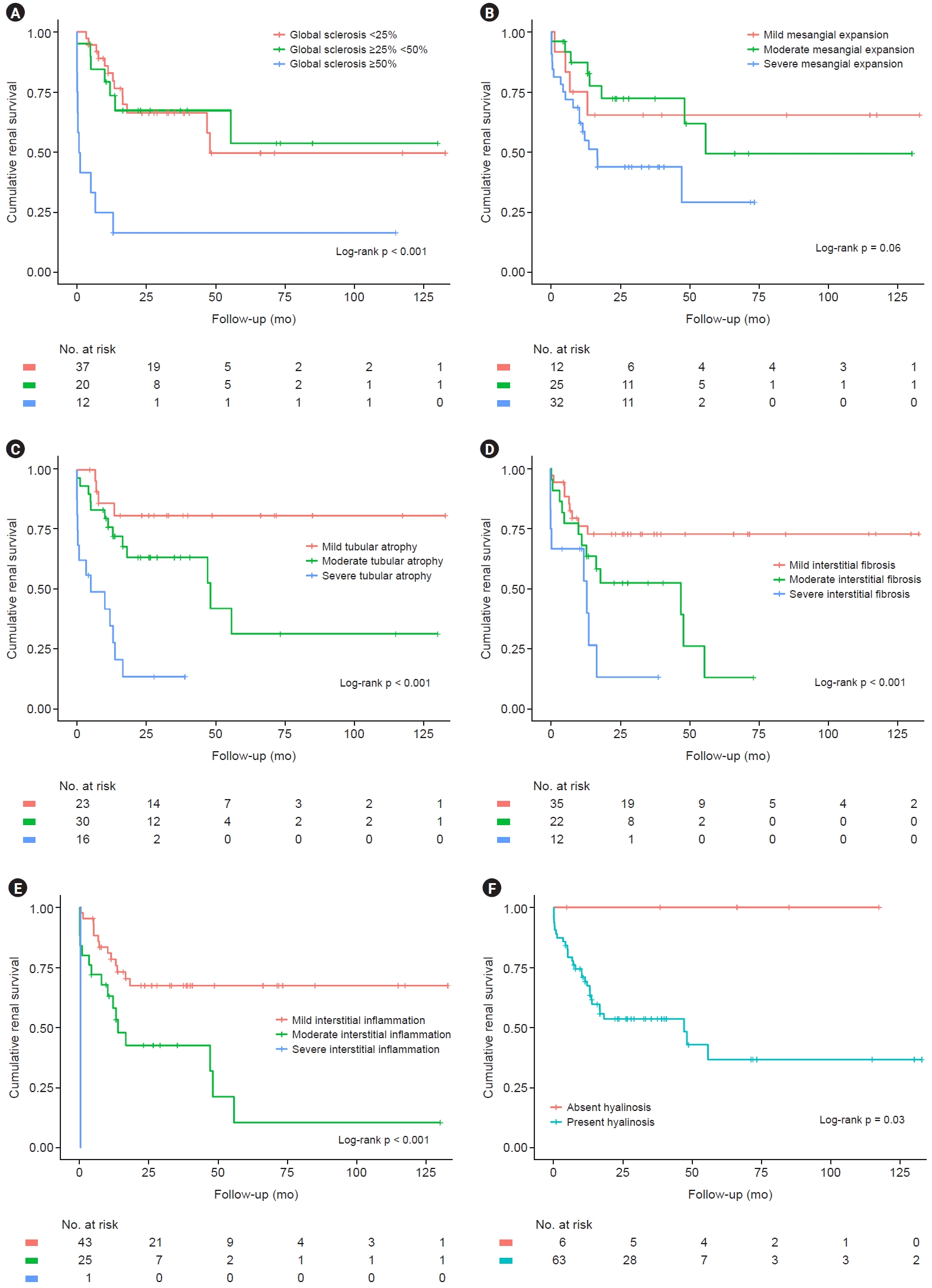
Figure┬Ā3.
Cumulative renal survival grouped by pathologic features in patients with DKD alone.
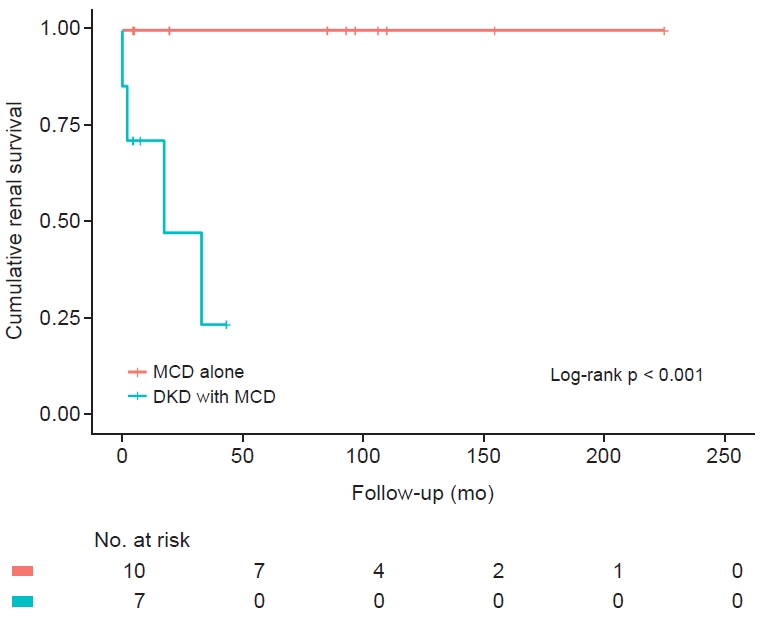
Figure┬Ā4.
Cumulative renal survival in patients with MCD alone and DKD with MCD.
Table┬Ā1.
Data are expressed as number only, mean ┬▒ standard deviation, or number (%).
ATN, acute tubular necrosis; BUN, blood urea nitrogen; Cr, creatinine; eGFR, estimated glomerular filtration rate; FSGS, focal segmental glomerulosclerosis; GN, glomerulonephritis; IgAN, immunoglobulin A nephropathy; MAP, mean arterial pressure; MCD, minimal change disease; MN, membranous nephropathy; MPGN, membranoproliferative glomerulonephritis; T2DM, type 2 diabetes mellitus; TIN, tubulointerstitial nephritis.
Table┬Ā2.
| Variable | DKD alone | NDKD | DKD/NDKD | p-value |
|---|---|---|---|---|
| No. of patients | 69 | 146 | 22 | |
| Age (yr) | 52.3 ┬▒ 12.5 | 55.7 ┬▒ 12.9 | 53.8 ┬▒ 14.4 | 0.18 |
| Male sex | 41 (59.4) | 91 (62.3) | 12 (54.5) | 0.76 |
| Body mass index (kg/m2) | 26.0 ┬▒ 4.8 | 25.8 ┬▒ 4.1 | 24.5 ┬▒ 3.5 | 0.35 |
| MAP (mmHg) | 98.8 ┬▒ 10.2 | 95.2 ┬▒ 16.3 | 96.8 ┬▒ 12.0 | 0.23 |
| Hypertension | 56 (81.2) | 91 (62.3) | 14 (63.6) | 0.02 |
| Hemoglobin (g/dL) | 10.8 ┬▒ 1.9 | 12.0 ┬▒ 2.3 | 10.8 ┬▒ 1.9 | <0.001a,b |
| Serum albumin (g/dL) | 3.2 ┬▒ 0.8 | 3.1 ┬▒ 0.9 | 3.0 ┬▒ 0.9 | 0.50 |
| BUN (mg/dL) | 29.7 ┬▒ 13.1 | 24.6 ┬▒ 15.9 | 30.0 ┬▒ 18.5 | 0.045a |
| Serum Cr (mg/dL) | 2.2 ┬▒ 1.7 | 2.0 ┬▒ 2.2 | 2.2 ┬▒ 1.7 | 0.69 |
| eGFR (mL/min/1.73 m2) | 42.7 ┬▒ 24.1 | 52.9 ┬▒ 29.3 | 42.1 ┬▒ 23.1 | 0.02a |
| 24-hr urinary protein (mg)c | 4,552 ┬▒ 3,249 | 3,558 ┬▒ 3,921 | 5,212 ┬▒ 5,816 | 0.08 |
| Biopsy resultsc | ||||
| ŌĆāDiabetic nephropathy | 69 (100) | 22 (100) | ||
| ŌĆāIgAN | 50 (34.2) | 4 (18.2) | ||
| ŌĆāFSGS | 25 (17.1) | 1 (4.5) | ||
| ŌĆāMN | 21 (14.4) | 4 (18.2) | ||
| ŌĆāMCD | 10 (6.8) | 7 (31.8) | ||
| ŌĆāMPGN | 5 (3.4) | |||
| ŌĆāCrescentic GN | 8 (5.5) | 1 (4.5) | ||
| ŌĆāLupus nephritis | 6 (4.1) | |||
| ŌĆāTIN | 11 (7.5) | 5 (22.7) | ||
| ŌĆāATN | 1 (0.7) | |||
| ŌĆāOthers | 9 (6.2) | |||
| Outcome | ||||
| ŌĆāESKD | 30 (43.5) | 23 (15.8) | 8 (36.4) | <0.001 |
| ŌĆāDeath | 1 (1.4) | 9 (6.2) | 0 (0) | 0.22 |
Data are expressed as number only, mean ┬▒ standard deviation, or number (%).
ATN, acute tubular necrosis; BMI, body mass index; BUN, blood urea nitrogen; Cr, creatinine; DKD, diabetic kidney disease; eGFR, estimated glomerular filtration rate; FSGS, focal segmental glomerulosclerosis; GN, glomerulonephritis; IgAN, immunoglobulin A nephropathy; MAP, mean arterial pressure; MCD, minimal change disease; MN, membranous nephropathy; MPGN, membranoproliferative glomerulonephritis; NDKD, non-diabetic kidney disease; TIN, tubulointerstitial nephritis.
Table┬Ā3.
| Group |
eGFR |
24-hr urinary protein |
||
|---|---|---|---|---|
| r | p-value | r | p-value | |
| DKD alone | ŌĆō0.143 | 0.03 | 0.088 | 0.18 |
| NDKD | 0.181 | 0.005 | ŌĆō0.142 | 0.03 |
| DKD/NDKD | ŌĆō0.070 | 0.23 | 0.097 | 0.14 |
Table┬Ā4.
Table┬Ā5.
| Variable | HR (95% CI) | p-value |
|---|---|---|
| Group | ||
| ŌĆāDKD alone (n = 69) | Reference | |
| ŌĆāNDKD (n = 143)a | 1.47 (0.52ŌĆō4.14) | 0.46 |
| ŌĆāDKD/NDKD (n = 22) | 2.73 (1.09ŌĆō6.85) | 0.03 |
| Age | 0.89 (0.69ŌĆō1.15) | 0.39 |
| Female sex | 0.56 (0.31ŌĆō1.00) | 0.048 |
| Body mass index | 0.98 (0.91ŌĆō1.06) | 0.69 |
| MAP | 1.13 (0.94ŌĆō1.36) | 0.20 |
| Hypertension | 1.37 (0.65ŌĆō2.86) | 0.41 |
| eGFR | 0.95 (0.94ŌĆō0.97) | <0.001 |
| 24-hr urinary proteinb | 1.32 (1.09ŌĆō1.60) | 0.004 |
| Global sclerosis (%) | ||
| ŌĆā<25 | Reference | |
| ŌĆāŌēź25, <50 | 0.96 (0.49ŌĆō1.88) | 0.91 |
| ŌĆāŌēź50 | 3.88 (1.75ŌĆō8.59) | 0.001 |
| Mesangial expansion | ||
| ŌĆāNone or mild | Reference | |
| ŌĆāModerate | 2.45 (1.02ŌĆō5.85) | 0.045 |
| ŌĆāSevere | 6.22 (2.34ŌĆō16.55) | <0.001 |
| Tubular atrophy | ||
| ŌĆāNone or mild | Reference | |
| ŌĆāModerate | 1.63 (0.70ŌĆō3.82) | 0.26 |
| ŌĆāSevere | 1.42 (0.45ŌĆō4.47) | 0.55 |
| Interstitial fibrosis | ||
| ŌĆāNone or mild | Reference | |
| ŌĆāModerate | 1.06 (0.48ŌĆō2.36) | 0.88 |
| ŌĆāSevere | 0.80 (0.30ŌĆō2.17) | 0.66 |
| Hyalinosis | 1.46 (0.63ŌĆō3.42) | 0.38 |
References
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 601 View
- 34 Download
- ORCID iDs
-
Wook-Joon Kim

https://orcid.org/0000-0003-4332-9861Taehoon Oh

https://orcid.org/0000-0002-2702-8332Nam Hun Heo

https://orcid.org/0000-0001-7278-2214Kyungsup Kwon

https://orcid.org/0000-0003-2954-3888Ga-Eun Shin

https://orcid.org/0000-0002-4489-6545Se-Hwi Jeong

https://orcid.org/0009-0005-4276-4943Ji Hye Lee

https://orcid.org/0000-0003-4214-1322Samel Park

https://orcid.org/0000-0002-5717-0743Nam-Jun Cho

https://orcid.org/0000-0002-9053-0499Hyo-Wook Gil

https://orcid.org/0000-0003-2550-2739Eun Young Lee

https://orcid.org/0000-0002-4513-9888 - Related articles
-
Nephrology consultation improves the clinical outcomes of patients with acute kidney injury



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















