1. Robinson BM, Zhang J, Morgenstern H, et al. Worldwide, mortality risk is high soon after initiation of hemodialysis.
Kidney Int 2014;85:158–165.


2. Bradbury BD, Fissell RB, Albert JM, et al. Predictors of early mortality among incident US hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS).
Clin J Am Soc Nephrol 2007;2:89–99.


3. Foley RN, Chen SC, Solid CA, Gilbertson DT, Collins AJ. Early mortality in patients starting dialysis appears to go unregistered.
Kidney Int 2014;86:392–398.


5. Saran R, Li Y, Robinson B, et al. US Renal Data System 2015 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2016;67(3 Suppl 1):A7–A8.
6. Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2016 Annual Data Report: epidemiology of kidney disease in the United States.
Am J Kidney Dis 2017;69:A7–A8.


7. Parati G, Ochoa JE, Bilo G, et al. Hypertension in chronic kidney disease Part 1: out-of-office blood pressure monitoring: methods, thresholds, and patterns.
Hypertension 2016;67:1093–1101.


9. Aftab RA, Sellappans R, Ming CK, Shaik I. Taking a step further in identifying ideal blood pressure range among hemodialysis patients: a systematic review and a meta-analysis.
Front Pharmacol 2020;11:729.



10. Son HE, Ryu JY, Go S, et al. Association of ambulatory blood pressure monitoring with renal outcome in patients with chronic kidney disease.
Kidney Res Clin Pract 2020;39:70–80.



11. Viazzi F, Cappadona F, Leoncini G, et al. Two-day ABPM-derived indices and mortality in hemodialysis patients.
Am J Hypertens 2020;33:165–174.



13. Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Greenland S, Kopple JD. Reverse epidemiology of hypertension and cardiovascular death in the hemodialysis population: the 58th annual fall conference and scientific sessions.
Hypertension 2005;45:811–817.


14. K/DOQI Workgroup. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients.
Am J Kidney Dis 2005;45:S1–S153.

16. Robinson BM, Tong L, Zhang J, et al. Blood pressure levels and mortality risk among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study.
Kidney Int 2012;82:570–580.



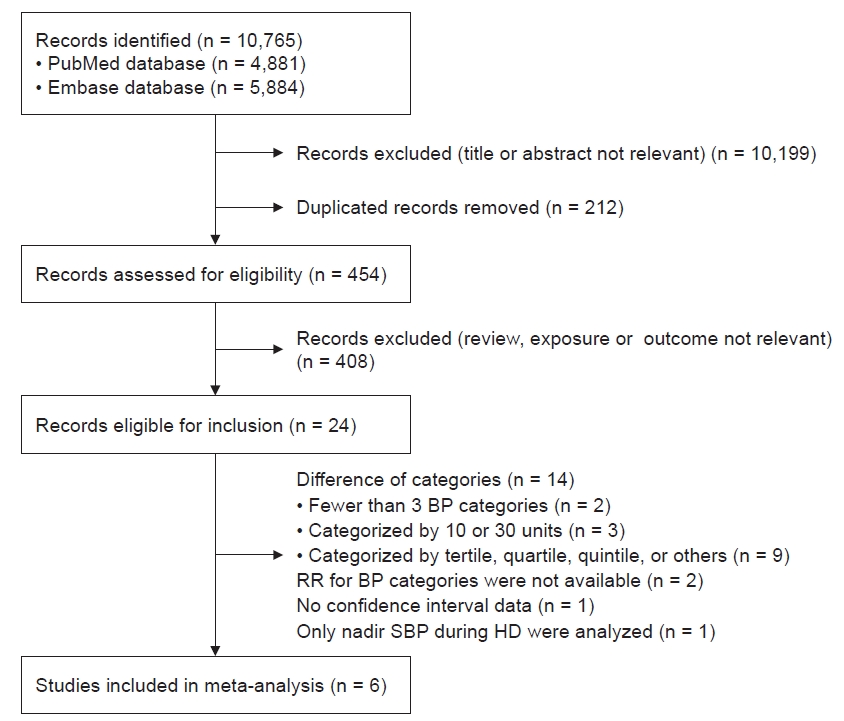
17. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration.
BMJ 2009;339:b2700.



18. Li Z, Lacson E Jr, Lowrie EG, et al. The epidemiology of systolic blood pressure and death risk in hemodialysis patients.
Am J Kidney Dis 2006;48:606–615.


19. Molnar MZ, Lukowsky LR, Streja E, et al. Blood pressure and survival in long-term hemodialysis patients with and without polycystic kidney disease.
J Hypertens 2010;28:2475–2484.



20. Chang TI, Friedman GD, Cheung AK, Greene T, Desai M, Chertow GM. Systolic blood pressure and mortality in prevalent haemodialysis patients in the HEMO study.
J Hum Hypertens 2011;25:98–105.



21. Sipahioglu MH, Usvyat L, Liu L, et al. Early systolic blood pressure changes in incident hemodialysis patients are associated with mortality in the first year.
Kidney Blood Press Res 2012;35:663–670.



22. Flythe JE, Inrig JK, Shafi T, et al. Association of intradialytic blood pressure variability with increased all-cause and cardiovascular mortality in patients treated with long-term hemodialysis.
Am J Kidney Dis 2013;61:966–974.



23. Inaba M, Karaboyas A, Akiba T, et al. Association of blood pressure with all-cause mortality and stroke in Japanese hemodialysis patients: the Japan Dialysis Outcomes and Practice Pattern Study.
Hemodial Int 2014;18:607–615.

24. Harnett JD, Kent GM, Barre PE, Taylor R, Parfrey PS. Risk factors for the development of left ventricular hypertrophy in a prospectively followed cohort of dialysis patients.
J Am Soc Nephrol 1994;4:1486–1490.


25. Patel RK, Oliver S, Mark PB, et al. Determinants of left ventricular mass and hypertrophy in hemodialysis patients assessed by cardiac magnetic resonance imaging.
Clin J Am Soc Nephrol 2009;4:1477–1483.



26. Kitahara T, Ono K, Tsuchida A, et al. Impact of brachial-ankle pulse wave velocity and ankle-brachial blood pressure index on mortality in hemodialysis patients.
Am J Kidney Dis 2005;46:688–696.


27. Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease.
Circulation 1999;99:2434–2439.


28. Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease.
Hypertension 2001;38:938–942.


29. Foley RN, Parfrey PS, Harnett JD, Kent GM, Murray DC, Barre PE. Impact of hypertension on cardiomyopathy, morbidity and mortality in end-stage renal disease.
Kidney Int 1996;49:1379–1385.


30. Silberberg JS, Barre PE, Prichard SS, Sniderman AD. Impact of left ventricular hypertrophy on survival in end-stage renal disease.
Kidney Int 1989;36:286–290.


31. London GM, Pannier B, Guerin AP, et al. Alterations of left ventricular hypertrophy in and survival of patients receiving hemodialysis: follow-up of an interventional study.
J Am Soc Nephrol 2001;12:2759–2767.

32. Zoccali C, Benedetto FA, Mallamaci F, et al. Left ventricular mass monitoring in the follow-up of dialysis patients: prognostic value of left ventricular hypertrophy progression.
Kidney Int 2004;65:1492–1498.


33. Wizemann V, Wabel P, Chamney P, et al. The mortality risk of overhydration in haemodialysis patients.
Nephrol Dial Transplant 2009;24:1574–1579.



34. Zoccali C, Moissl U, Chazot C, et al. Chronic fluid overload and mortality in ESRD.
J Am Soc Nephrol 2017;28:2491–2497.



36. Daugirdas JT. Measuring intradialytic hypotension to improve quality of care.
J Am Soc Nephrol 2015;26:512–514.


37. Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM. Association of mortality risk with various definitions of intradialytic hypotension.
J Am Soc Nephrol 2015;26:724–734.


38. Sands JJ, Usvyat LA, Sullivan T, et al. Intradialytic hypotension: frequency, sources of variation and correlation with clinical outcome.
Hemodial Int 2014;18:415–422.


39. Stefánsson BV, Brunelli SM, Cabrera C, et al. Intradialytic hypotension and risk of cardiovascular disease.
Clin J Am Soc Nephrol 2014;9:2124–2132.



40. Chang TI, Paik J, Greene T, et al. Intradialytic hypotension and vascular access thrombosis.
J Am Soc Nephrol 2011;22:1526–1533.



41. Port FK, Hulbert-Shearon TE, Wolfe RA, et al. Predialysis blood pressure and mortality risk in a national sample of maintenance hemodialysis patients.
Am J Kidney Dis 1999;33:507–517.


42. Zager PG, Nikolic J, Brown RH, et al. “U” curve association of blood pressure and mortality in hemodialysis patients.
Kidney Int 1998;54:561–569.


43. Shoji T, Tsubakihara Y, Fujii M, Imai E. Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients.
Kidney Int 2004;66:1212–1220.


44. Agarwal R. Hypertension and survival in chronic hemodialysis patients: past lessons and future opportunities.
Kidney Int 2005;67:1–13.


45. Burton JO, Jefferies HJ, Selby NM, McIntyre CW. Hemodialysis-induced cardiac injury: determinants and associated outcomes.
Clin J Am Soc Nephrol 2009;4:914–920.


46. Carney EF. Dialysis: U-shaped associations between changes in blood pressure during dialysis and patient survival.
Nat Rev Nephrol 2013;9:431.



47. Chaturvedi N. Ethnic differences in cardiovascular disease.
Heart 2003;89:681–686.



48. Meadows TA, Bhatt DL, Cannon CP, et al. Ethnic differences in cardiovascular risks and mortality in atherothrombotic disease: insights from the Reduction of Atherothrombosis for Continued Health (REACH) registry.
Mayo Clin Proc 2011;86:960–967.



49. Pu J, Hastings KG, Boothroyd D, et al. Geographic variations in cardiovascular disease mortality among Asian American subgroups, 2003-2011.
J Am Heart Assoc 2017;6:e005597.



50. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease.
Kidney Int 2021;99:S1–S87.


51. Visseren FL, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice.
Eur Heart J 2021;42:3227–3337.

52. National Kidney Foundation.. KDOQI clinical practice guideline for hemodialysis adequacy: 2015 update.
Am J Kidney Dis 2015;66:884–930.

53. Sarafidis PA, Persu A, Agarwal R, et al. Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) and the Hypertension and the Kidney working group of the European Society of Hypertension (ESH).
Nephrol Dial Transplant 2017;32:620–640.


54. Agarwal R. Blood pressure and mortality among hemodialysis patients.
Hypertension 2010;55:762–768.


55. Hara M, Tanaka S, Taniguchi M, et al. Prognostic value of pre-dialysis blood pressure and risk threshold on clinical outcomes in hemodialysis patients: the Q-Cohort Study.
Medicine (Baltimore) 2018;97:e13485.


56. Tsuruya K, Kanda E, Nomura T, Iseki K, Hirakata H. Postdialysis blood pressure is a better predictor of mortality than predialysis blood pressure in Japanese hemodialysis patients: the Japan Dialysis Outcomes and Practice Patterns Study.
Hypertens Res 2020;43:791–797.



57. Ezzatzadegan Jahromi S, Haghighi G, Roozbeh J, Ebrahimi V. Comparisons between different blood pressure measurement techniques in patients with chronic kidney disease.
Kidney Res Clin Pract 2019;38:212–219.


















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















